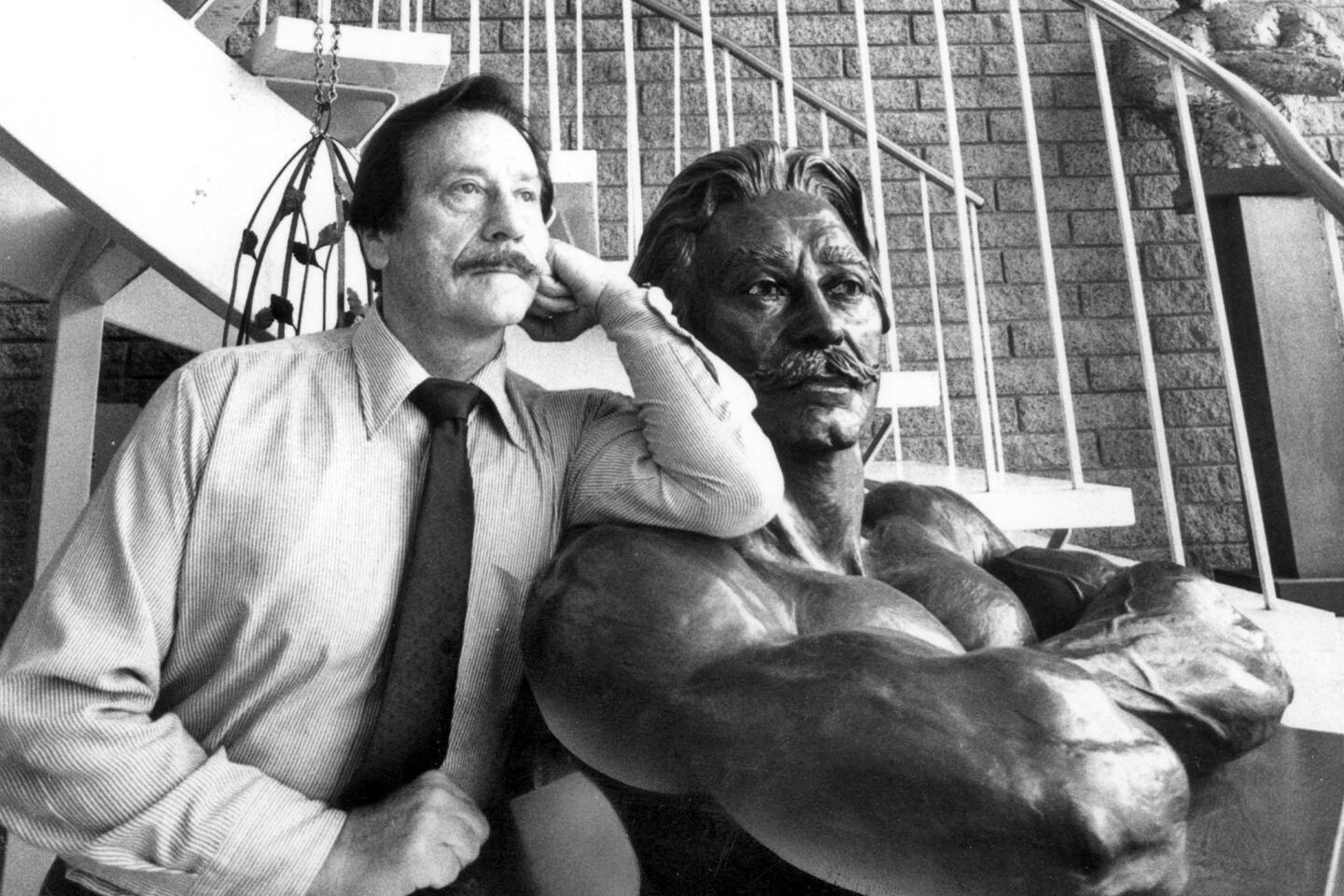
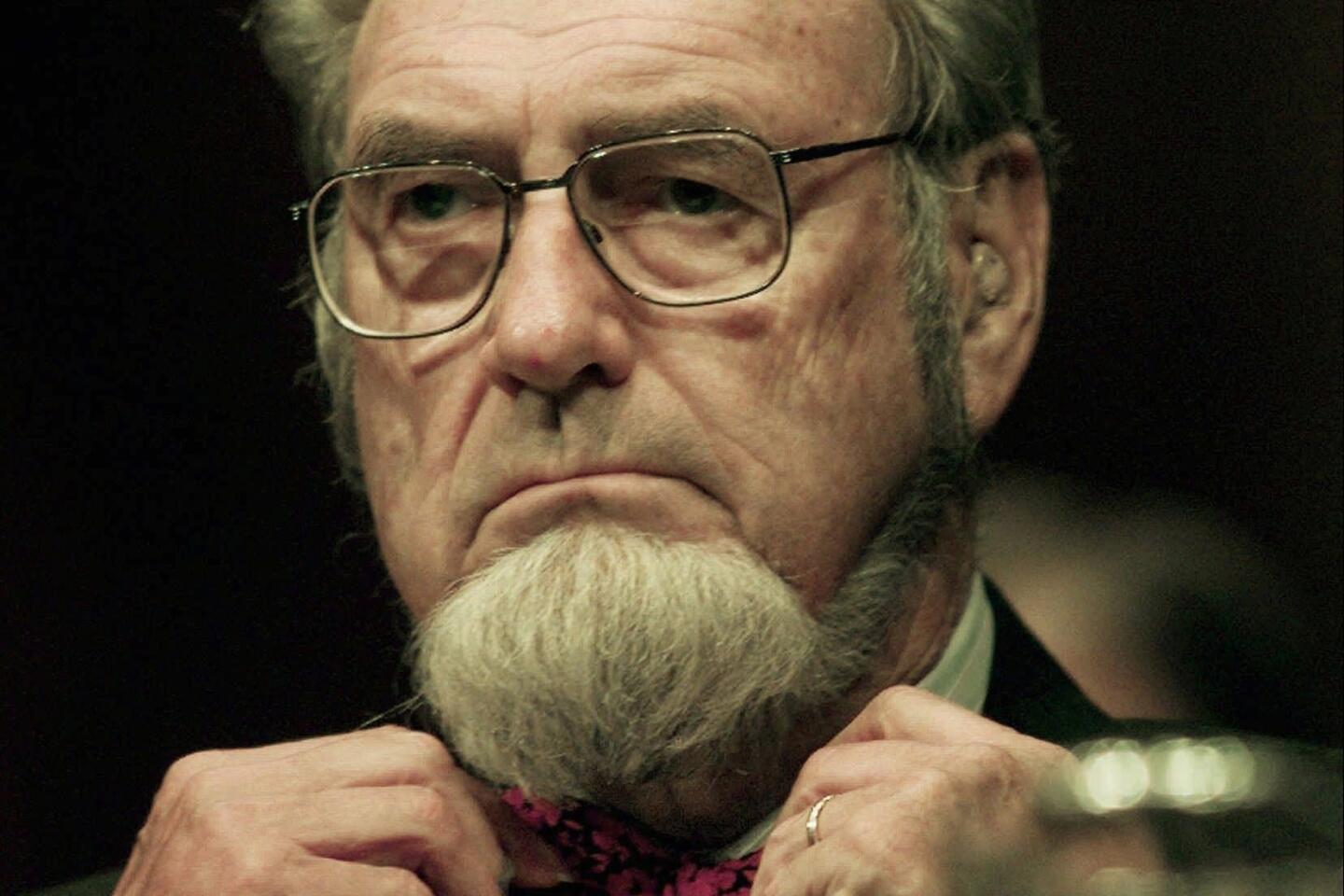
Leonard Apt dies; UCLA pediatric ophthalmologist was 90
- Share via
During the first half of the 20th century, pediatricians generally believed that children’s eye problems were largely self-corrective — that a child would grow out of his or her crossed eyes or poor vision. But they were wrong.
Unless a vision problem is detected and corrected early, the child will have vision problems in that eye for the rest of his or her life. Subsequent studies have shown that 2% to 5% of preschool children have vision problems, many of them not apparent.
In the late 1940s, a small group of physicians began to recognize this problem. One of them was Dr. Leonard Apt, a pediatrician who spent most of his career at UCLA. “During my pediatric training, I would request a consultation for a baby who was having a vision problem and the ophthalmologists would ask, ‘How do you get information from a baby?’” he said. “That’s when I realized I could adapt my pediatric techniques to ophthalmology.”
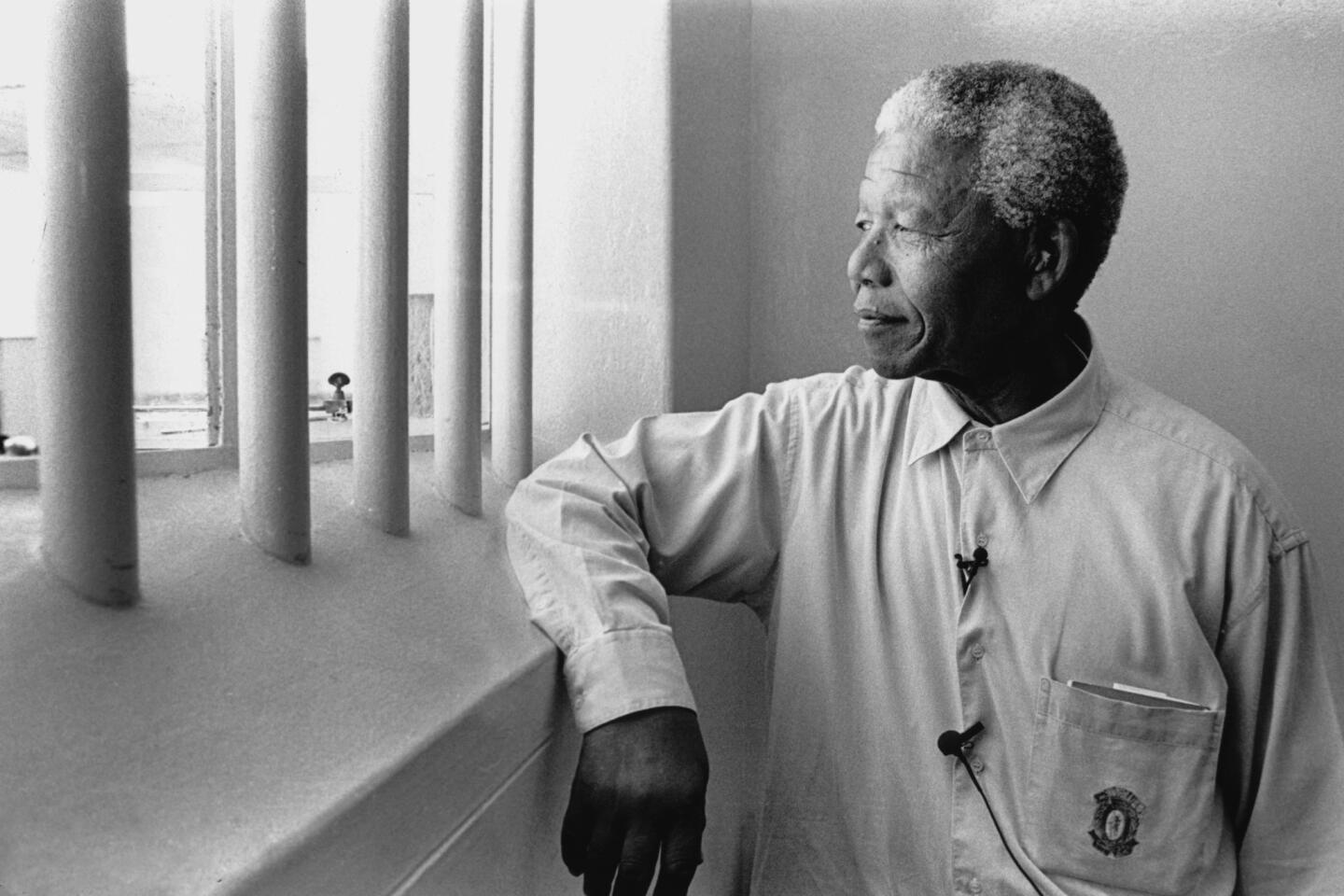
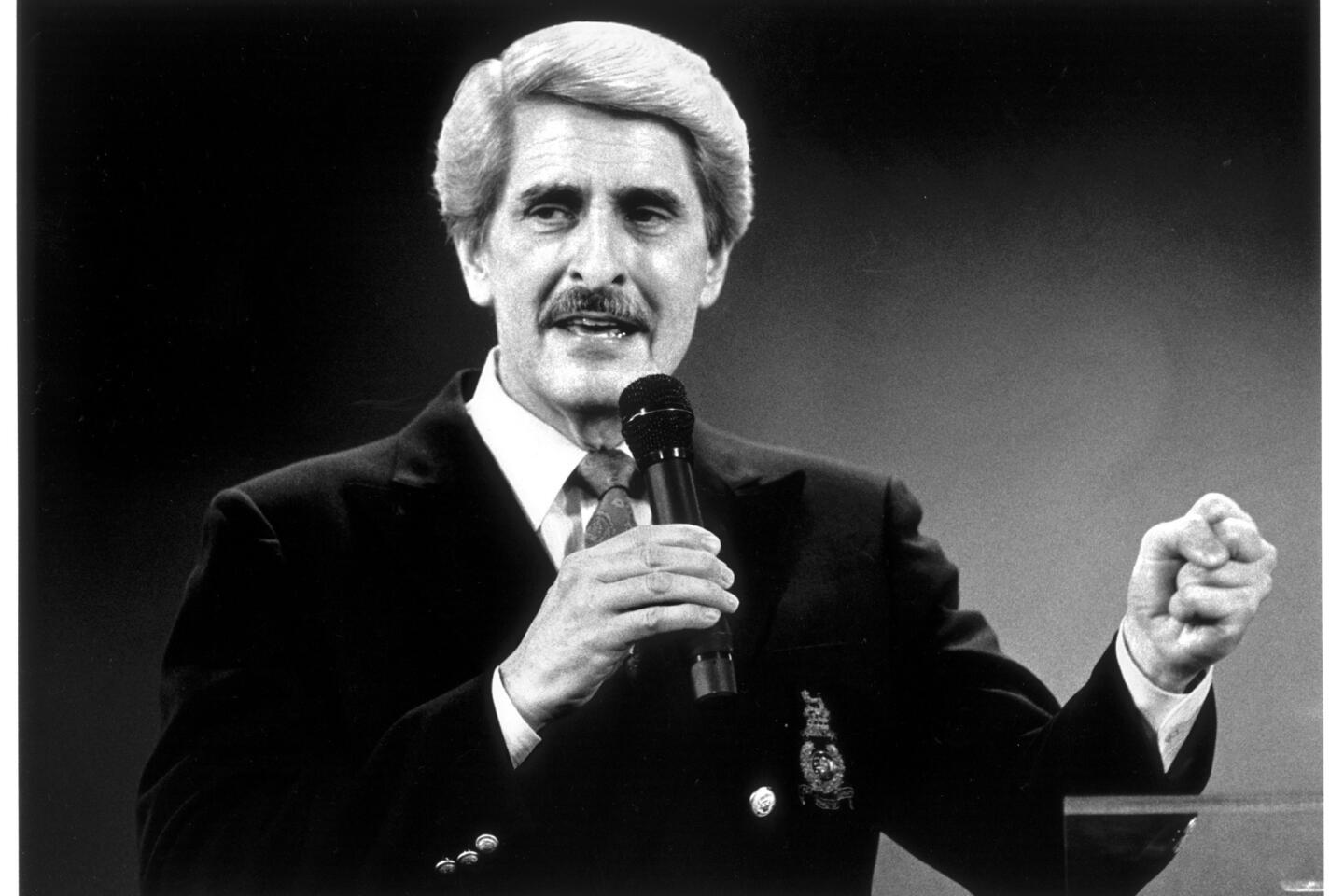
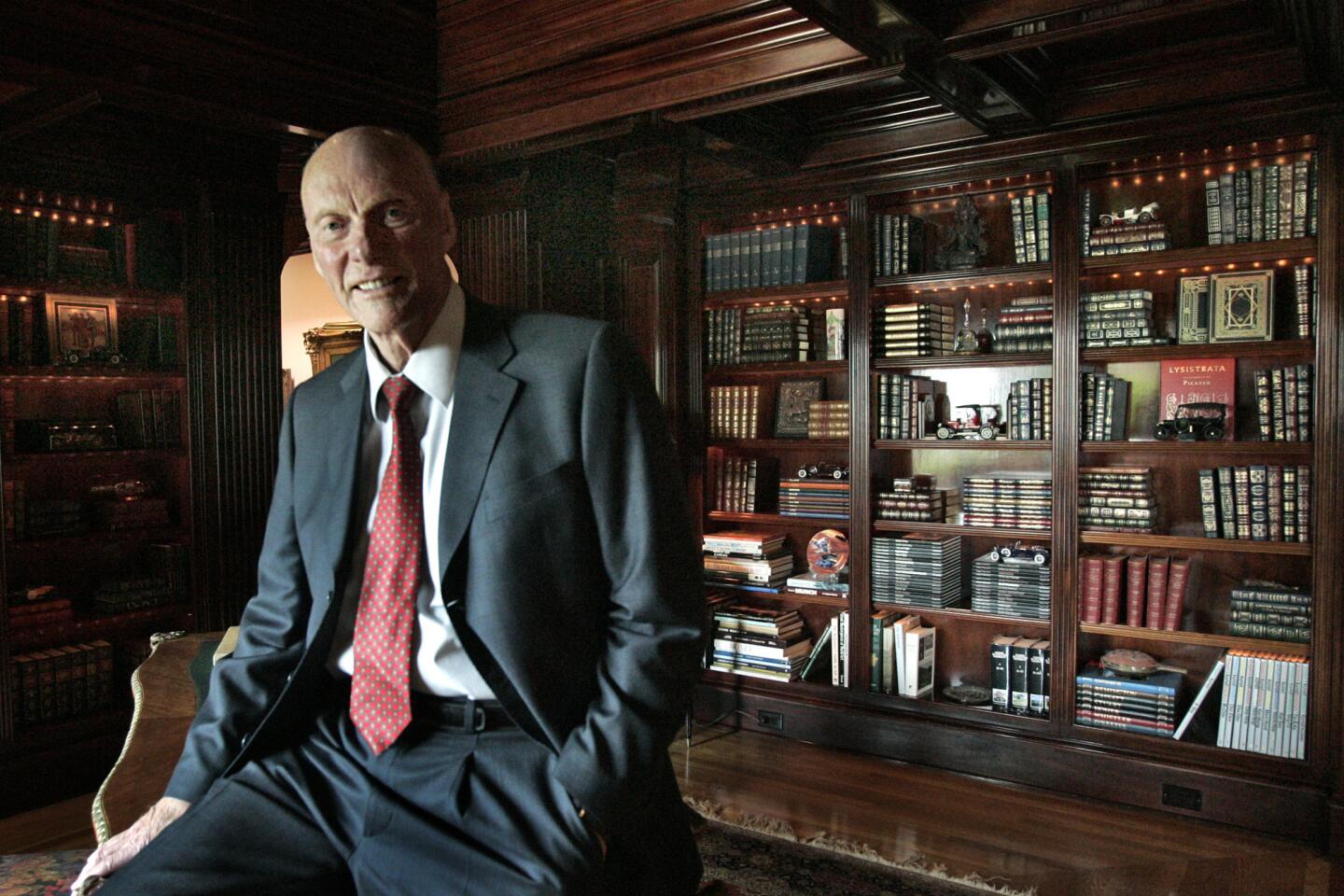
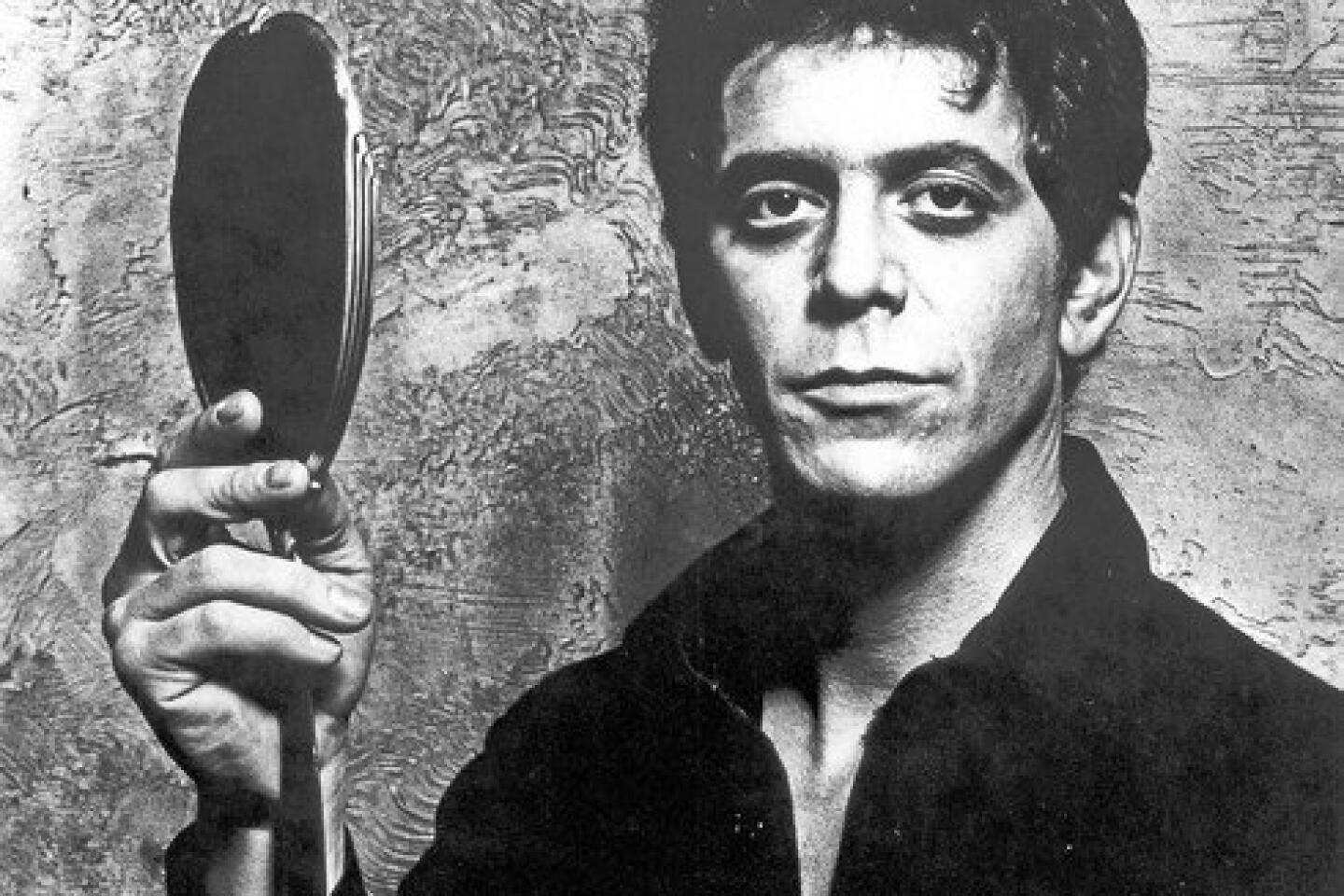
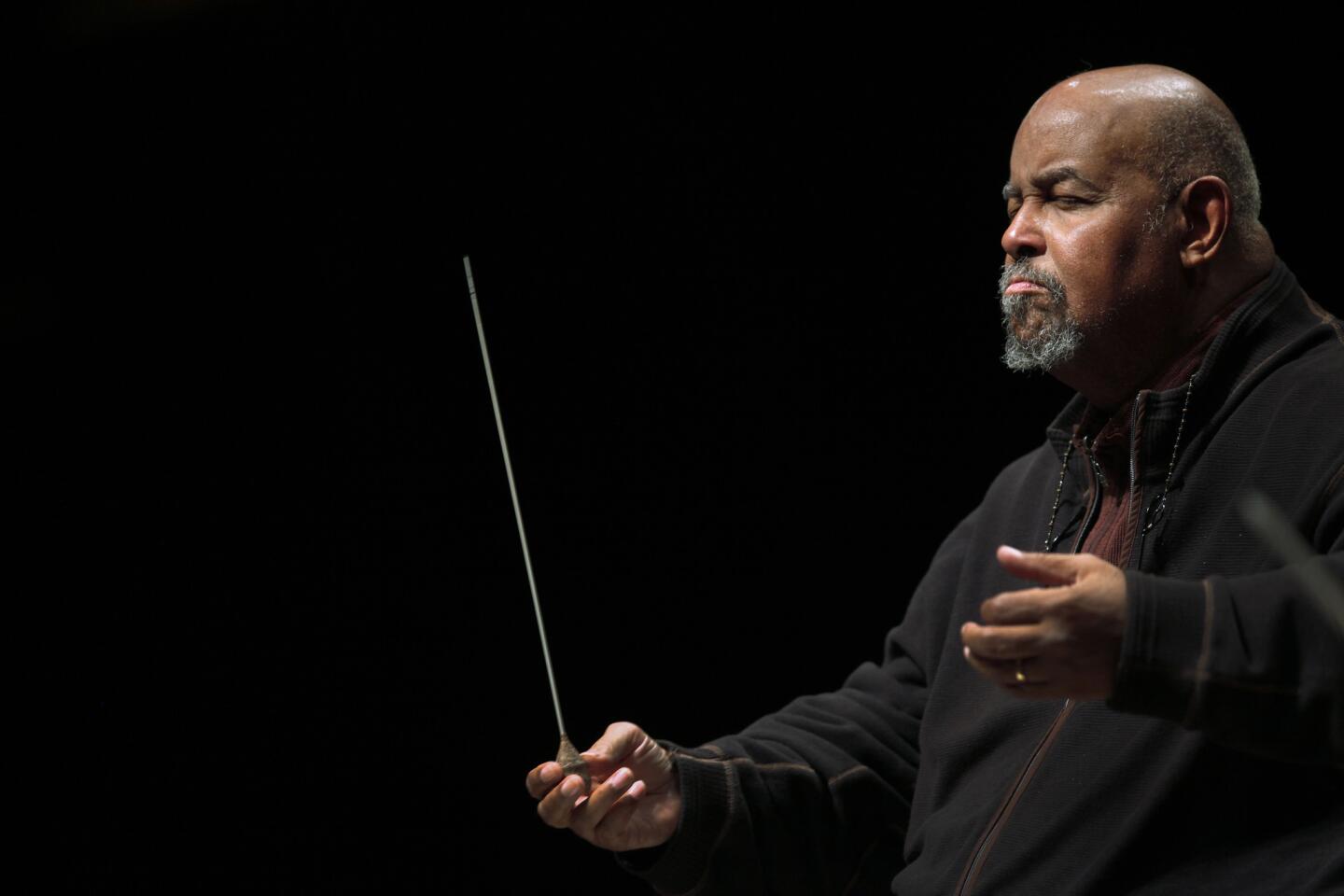
PHOTOS: Notable deaths of 2013
Apt stepped aside from his pediatric work and learned ophthalmology, becoming the first person to have a fellowship in pediatric ophthalmology at the National Institutes of Health and the first physician to be board-certified in both pediatrics and ophthalmology. At UCLA, he established the first division of pediatric ophthalmology at a U.S. medical school and was one of the five founders of the Jules Stein Eye Institute.
Apt died Friday at UCLA Santa Monica Medical Center after a brief illness, the university announced. He was 90.
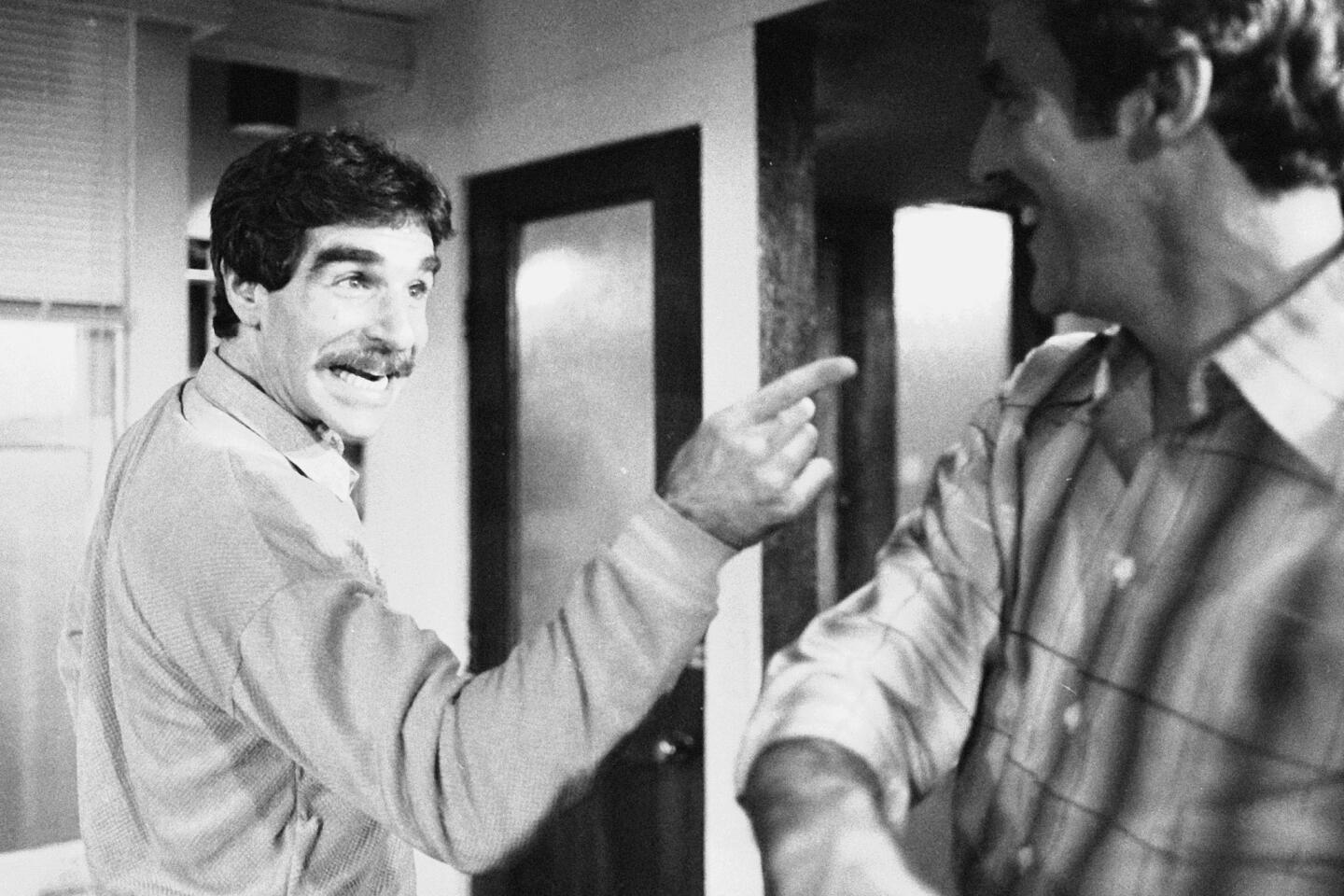
Innovations pioneered by Apt saved the eyesight of hundreds of thousands — if not millions — of children. “He was truly one of a kind,” said his colleague Dr. Sherwin Isenberg of UCLA.
Apt is probably best known for the Apt test, developed while he was a pediatrician at Harvard Medical School in the early 1950s. When a pregnant woman exhibits vaginal bleeding or a newborn infant has bloody stools or vomitus, it is crucial to determine whether the blood belongs to mother or child.
Apt developed a simple test to distinguish between the two types of blood, focusing on hemoglobin, the oxygen-carrying portion of blood. Fetal hemoglobin has a slightly different composition than that of adult hemoglobin and is substantially more resistant to degradation by a base, such as sodium hydroxide.
The Apt test involves isolating hemoglobin from a small amount of blood, then exposing it to sodium hydroxide and examining it under a microscope. If the hemoglobin then appears pinkish, it is from the fetus; if it is yellowish-brown, it is from the mother. The Apt test “was a major breakthrough,” Isenberg said. It is still widely used, but it is being supplanted by a newer test that determines proportions of fetal and maternal blood.
Apt was also the first physician to describe agammaglobulinemia, a genetic defect in which the immune system does not produce crucial components called B-lymphocytes, and mothball anemia, a severe loss of blood cells produced when children eat naphthalene-containing mothballs.
He was also among the first to use plastic tubing and other equipment for blood transfusions. Physicians had previously used glass and metal apparatus. But people tend to forget his pediatric contributions, Isenberg said, “because they remember his ophthalmic innovations.”
Among Apt’s early work in the field were studies of nematode endophthalmitis, an inflammation of children’s’ eyes caused by infections with dog and cat roundworms, and of melanomas of the uvea layer of the eye, which he demonstrated were more common in children than previously suspected. He also studied allergies to the catgut and collagen sutures once used in children’s eyes, a common side effect that could lead to severe visual impairment. He demonstrated that the reactions could be predicted by first placing a suture in the child’s forearm to observe potential reactions, allowing the surgeon to use alternate materials when necessary.
Apt and Isenberg spent much of the last three decades studying ways to prevent eye infections. Before they began, eye surgeons routinely sterilized the patients’ eyes with silver nitrate or antibiotics in an attempt to prevent infections. The pair showed that this procedure actually increases infections.
For infections that did result after the surgery, the team found that a diluted solution of povidone-iodine — known commercially as Betadine — was more effective than either silver nitrate or antibiotics and was less likely to produce allergic reactions.
In the 1990s, they demonstrated in a large study in Kenya that Betadine was more effective and safer than either silver nitrate or antibiotics in preventing conjunctivitis in newborns. Such infections occur when the fetus contracts a bacterium while passing through the vagina. Both silver nitrate and antibiotics were too expensive for routine use in Third World countries, but Betadine is just pennies a dose.
They subsequently demonstrated that the drug is also effective against keratitis, which blinds 400,000 children per year worldwide, and fungal infections.
Leonard Apt was born in Philadelphia on June 28, 1922. He entered the University of Pennsylvania at 14, graduating with highest honors, and received his medical degree from Jefferson Medical College in Philadelphia in 1945. After a series of positions around the country, he joined UCLA in 1961 and remained there the rest of his career. He was still active at his death.
He co-founded the UCLA Center to Prevent Childhood Blindness and in 1999 established an extensive preschool vision testing program at the university.
With funds from family trusts, Apt was also a generous philanthropist, endowing both a chair and a fellowship in ophthalmology at UCLA and contributing extensively to alumni programs at his various schools, as well as to the arts.
Apt never married and was preceded in death by his three sisters. He had no immediate survivors.
More to Read
Start your day right
Sign up for Essential California for the L.A. Times biggest news, features and recommendations in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.