Number of uninsured children climbs, reversing more than a decade of progress, report finds

- Share via
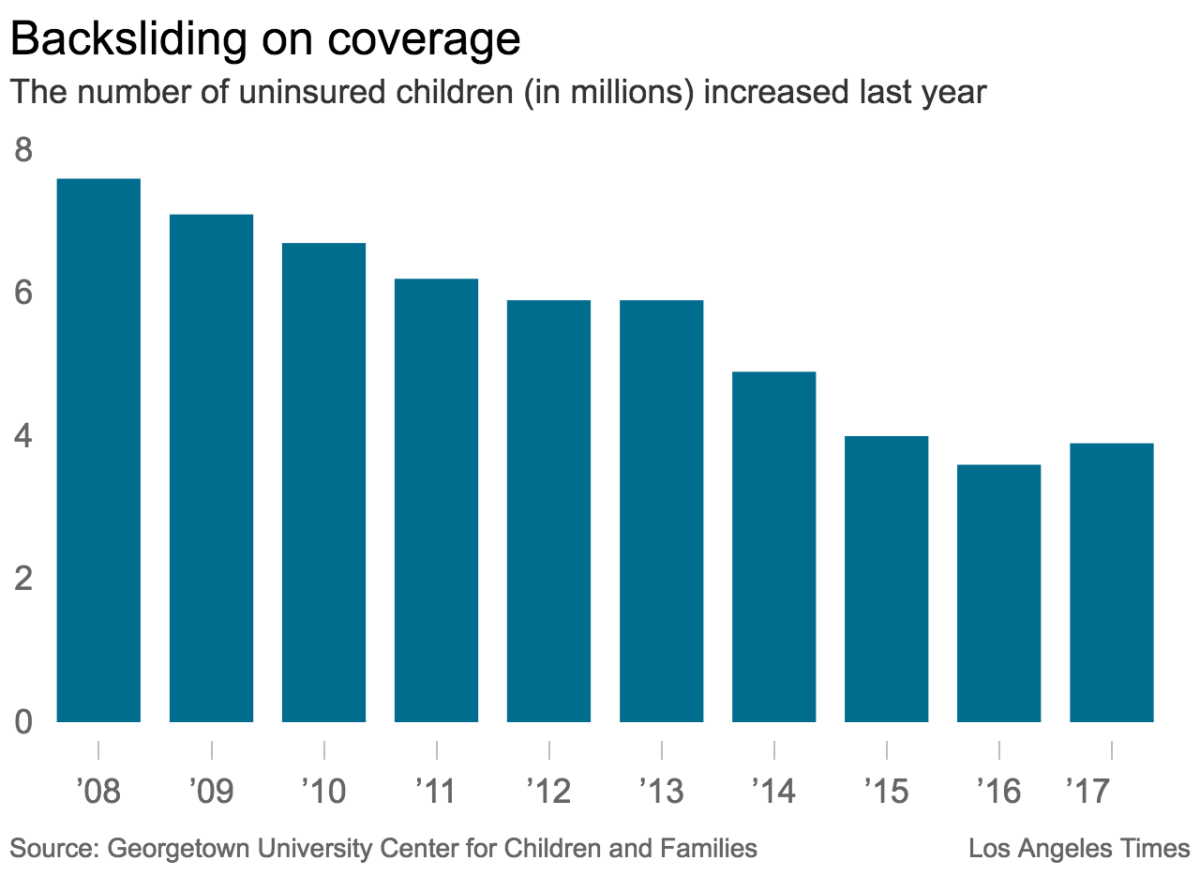
Reporting from Washington — The number of children in the United States without health insurance increased last year for the first time in more than a decade, according to a new report that highlights potentially worrisome backsliding in pediatric care.
The erosion in health insurance came despite a robust economy, which in the past has helped fuel expansions in coverage.
For the record:
8:35 a.m. Nov. 29, 2018A previous version of this article said there were 27,000 additional uninsured children in 2017. There were 270,000 more uninsured children.
It likely reflects a number of steps taken by the Trump administration and the Republican-controlled Congress that have targeted safety net programs such as Medicaid and the Children’s Health Insurance Program known as CHIP, note the authors of the new report from Georgetown University’s Center for Children and Families.
“With an improving economy and a very low unemployment rate, the fact that our nation is going backwards on children’s health coverage is very troubling,” said Joan Alker, the center’s director and the report’s lead author.
“Without serious efforts to get back on track, the decline in coverage is likely to continue in 2018 and may, in fact, get worse for America’s children,” Alker added.
A spokeswoman for Health and Human Services Secretary Alex Azar, who has responsibility for coverage programs for children, referred questions about the coverage decline to the federal Centers for Medicare and Medicaid Services.
A spokesman for that agency did not address the report’s findings, saying only that the agency “coordinates a national outreach and enrollment initiative that reaches out to families with children and teens eligible for Medicaid and CHIP.”
Pediatricians and public health experts widely agree that health insurance is key to ensuring children get recommended care, including regular health screenings and vaccinations.
And over the last quarter-century, Democrats and Republicans at the federal and state levels have worked to close coverage gaps by expanding public programs, a move that has helped drive down the uninsured rate for children to historically low levels.
In 2016, just 4.7% of children 18 and younger lacked health insurance, according to the census data. That was down from 9.7% in 2008.
The gains were particularly critical in many poor, rural parts of the country. Medicaid and CHIP cover more than half of all children in nearly a quarter of U.S. counties, data show.
“Coverage is just so critical for kids,” said Dr. Dennis Cooley, a pediatrician in Topeka, Kan., who chairs the American Academy of Pediatrics’ subcommittee on access to care. “When kids have coverage, they come in when they should. The result is you can pick up illnesses early on and catch developmental issues early before they get worse.”
In 2017, however, progress reversed, as the uninsured rate among children ticked up from 4.7% to 5%.
That translates to about 270,000 more children without health coverage, according to the new report, which is based on an analysis of census data.
The coverage losses were most pronounced in nine states: South Dakota, Texas, Georgia, South Carolina, Florida, Ohio, Tennessee, Utah and Massachusetts.
With the exception of Ohio and Massachusetts, these Republican-led states have elected not to expand Medicaid coverage through the Affordable Care Act.
In Texas, more than one in 10 children now lacks health insurance, making Texas the only state with a children’s uninsured rate greater than 10%. By contrast, the uninsured rate among Massachusetts children is just 1.5%.
Across the country, not a single state saw a significant decline in the number of uninsured children in 2017, the Georgetown report found, the first time that has happened in at least a decade.
“The absence of significant progress across the country suggests that even states with the best intentions were unable to withstand strong national currents to protect children from losing coverage,” the report notes.
Among those trends was the concerted effort in 2017 by President Trump and congressional Republicans to roll back the 2010 healthcare law, often called Obamacare, and cut hundreds of billions of dollars in federal aid for Medicaid and CHIP.
That campaign was ultimately unsuccessful, but many low-income parents may have been discouraged from enrolling their children in government plans out of fear the coverage would not be available, Alker said.
Compounding that problem, Congress for months delayed legislation to reauthorize CHIP funding for states. That prompted state health officials across the country to warn parents that their children might lose coverage.
Created in 1997, CHIP is a government health insurance plan for children of working families who earn too much to qualify for fully subsidized Medicaid coverage but cannot afford most commercial health plans.
In addition to targeting Medicaid and CHIP, the Trump administration has dramatically scaled back marketing and assistance to inform Americans about health coverage on marketplaces created by the healthcare law and to help them sign up.
Administration officials have also issued warnings that immigrant parents who enroll their children in government health plans such as Medicaid risk losing the ability to get green cards, even if the children are U.S. citizens.
The administration in October issued a formal proposal for the new policy.
The proposed rule has been widely condemned by health officials, physician groups, hospitals and patient advocates across the country, who warn that it risks discouraging people from seeking necessary care.
The Department of Homeland Security acknowledged in its proposal that the new regulation may lead to “worse health outcomes, including increased prevalence of obesity and malnutrition, especially for pregnant or breastfeeding women, infants or children.”
The rule is nonetheless expected to be finalized early next year.
More stories from Noam N. Levey »
Twitter: @noamlevey
More to Read
Get the L.A. Times Politics newsletter
Deeply reported insights into legislation, politics and policy from Sacramento, Washington and beyond. In your inbox twice per week.
You may occasionally receive promotional content from the Los Angeles Times.











