Study reveals toll of being Black in U.S.: 1.6 million excess deaths over 22 years

- Share via
Research has long shown that Black people live sicker lives and die younger than white people.
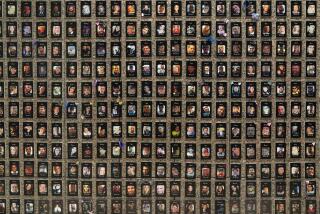
Now a new study, published Tuesday in the medical journal JAMA, casts the nation’s racial inequities in stark relief, finding that the higher mortality rate among Black Americans resulted in 1.63 million excess deaths relative to white Americans over more than two decades.
Because so many Black people die young — when they had so many years of life ahead of them — their higher mortality rate from 1999 to 2020 resulted in a cumulative loss of more than 80 million years of life compared with the white population, the study showed.
Although the nation made progress in closing the gap between white and Black mortality rates from 1999 to 2011, that advance stalled from 2011 to 2019. In 2020, the enormous number of deaths from COVID-19 — which hit Black Americans particularly hard — erased two decades of progress.
Two decades of progress in closing a yawning gap between the life expectancy of Black and white Americans has been erased by COVID-19.
Authors of the study describe it as a call to action to improve the health of Black Americans, whose early deaths are fueled by higher rates of heart disease, cancer and infant mortality.
“The study is hugely important for about 1.63 million reasons,” said Dr. Herman Taylor, an author of the study and director of the cardiovascular research institute at the Morehouse School of Medicine.
“Real lives are being lost. Real families are missing parents and grandparents,” Taylor said. “Babies and their mothers are dying. We have been screaming this message for decades.”
High mortality rates among Black people have less to do with genetics than with the country’s long history of discrimination, which has undermined educational, housing and job opportunities for generations of Black people, said Dr. Clyde Yancy, an author of the study and chief of cardiology at Northwestern University’s Feinberg School of Medicine.
Black neighborhoods that were red-lined in the 1930s — designated too “high risk” for mortgages and other investments — remain poorer and sicker today, Yancy said. Formerly red-lined ZIP codes also had higher rates of COVID infection and death. “It’s very clear that we have an uneven distribution of health,” Yancy said. “We’re talking about the freedom to be healthy.”
A companion study estimates that racial and ethnic inequities cost the U.S. at least $421 billion in 2018, based on medical expenses, lost productivity and premature death.
A new California Health Care Foundation survey found Black and Latino Californians were more likely to have negative health provider experiences and medical debt.
In 2021, non-Latino white Americans had a life expectancy at birth of 76 years, while non-Hispanic Black Americans could expect to live only to 71. Much of that disparity is explained by the fact that non-Latino Black newborns are 2½ times as likely to die before their 1st birthdays as non-Latino whites. Non-Latina Black mothers are more than three times as likely as non-Latina white mothers to die of a pregnancy-related complication. (Latino people can be of any race or combination of races.)
Racial disparities in health are so entrenched that even education and wealth don’t fully erase them, said Dr. Tonia Branche, a neonatal-perinatal medicine fellow at Lurie Children’s Hospital of Chicago who was not involved in the JAMA study.
Black women with a college degree are more likely to die of pregnancy complications than white women without a high school diploma. Although researchers can’t fully explain this disparity, Branche said it’s possible that stress, including from systemic racism, takes a greater toll on the health of Black mothers than previously recognized.
Death creates ripples of grief throughout communities. Research has found that every death leaves an average of nine people in mourning.
Black people shoulder a great burden of grief, which can undermine their mental and physical health, said Khaliah Johnson, chief of pediatric palliative care at Children’s Healthcare of Atlanta. Given the high mortality rates throughout their life span, Black people are more likely than white people to be grieving the death of a close family member at any point in their lives.
“We as Black people all have some legacy of unjust, unwarranted loss and death that compounds with each new loss,” said Johnson, who was not involved with the new study. “It affects not only how we move through the world, but how we live in relationship with others and how we endure future losses.”
Her parents lost two sons — one who died a few days after birth and another who died as a toddler. In an essay published last year, Johnson recalled, “My parents asked themselves on numerous occasions, ‘Would the outcomes for our sons have been different, might they have received different care and lived, had they not been Black?’”
Johnson said she hopes the new study gives people greater understanding of all that’s lost when Black people die prematurely. “When we lose these lives young, when we lose that potential, that has an impact on all of society,” she said.
And in the Black community, “our pain is real and deep and profound, and it deserves attention and validation,” Johnson said. “It often feels like people just pass it over, telling you to stop complaining. But the expectation can’t be that we just endure these things and bounce back.”
Ahead of a new documentary about racial inequities in healthcare, the TV host opens up to The Times about her own experiences.
Teleah Scott-Moore said she struggles with the death of her 16-year-old son, Timothy, an athlete who hoped to attend Boston College and study sports medicine. He died of sudden cardiac arrest in 2011, a rare condition that kills about 100 young athletes a year. Research shows that hypertrophic cardiomyopathy, an underlying heart condition that can lead to sudden cardiac death, often goes unrecognized in Black patients.
Scott-Moore still wonders whether she should have recognized warning signs. She also has blamed herself for failing to protect her two younger sons, who found Timothy’s body after he collapsed.
At times, she said, she wanted to give up.
Instead, she said, the family created a foundation to promote education and health screenings to prevent such deaths. She hears from families all over the world, and supporting them has helped heal her pain.
“My grief comes back in waves, it comes back when I least expect it,” said Scott-Moore, of Baltimore County, Md. “Life goes on, but it’s a pain that never goes away.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — an independent source of health policy research, polling and journalism. Learn more about KFF.