Biotech’s bright hope
- Share via
TO the shrill whine of a high-speed drill, neurosurgeon Dr. Paul Larson makes two nickel-sized holes in Shirley Cooper’s skull. Guided by a computerized MRI map, he plunges a long, thin needle through one hole and deep into the brain -- and empties the syringe.
A very special payload trickles into her brain: genes that, if all goes well, will help her control the movement of her muscles.
It is a day in late May and Cooper, 60, an artist who lives near Seattle, has come to the UC San Francisco Medical Center to find some relief from the Parkinson’s disease that is stealing her identity. Without medication, she has trouble walking and talking, and can’t hold a paint brush. And the drugs are wearing off -- as they eventually do for all Parkinson’s patients. After that, she probably will deteriorate rapidly.
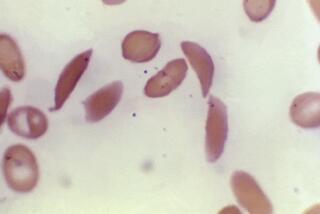
The experimental treatment Cooper is undergoing is intended to reverse that process. Parkinson’s destroys cells in the brain that make dopamine, and the loss of this key brain transmitter triggers the disease’s crippling symptoms: tremors in the arms, legs and face, stiff or frozen limbs, and impaired balance and coordination. In the trial she’s involved in -- the earliest of clinical tests, designed to assess safety -- scientists have engineered a harmless, stripped-down virus to carry a gene that will boost brain dopamine through the enzyme it encodes: amino acid decarboxylase, or AADC.
When the virus is injected into her brain, they hope the gene will be incorporated into healthy brain cells and steadily produce the enzyme.
Gene therapy is making a comeback after a series of serious setbacks that threatened to permanently derail human tests. In recent years, European scientists have cured more than two dozen patients suffering from three rare, and in some cases lethal, immune disorders.
Spurred by this success, plus the development of new techniques aimed at making the therapy safer and more effective, more than 300 gene therapy trials, including the one for Parkinson’s at UC San Francisco, are underway in the U.S. and abroad.
The approaches include what people traditionally think of as gene therapy: inserting functional genes to replace single, faulty ones to treat relatively rare genetic diseases such as muscular dystrophy, cystic fibrosis, sickle cell anemia, beta thalassemia and hemophilia. But, more and more, gene therapy is being studied as a treatment for lethal ills that are not inherited in any clear, simple way -- cancer, hepatitis, AIDS, heart disease -- and which also plague millions.
Today, scientists are injecting genes into people to try to block the formation of deadly cancerous tumors. They’re implanting genes that stimulate cell growth in an attempt to regenerate heart muscle cells and grow blood vessels in patients with congestive heart failure; halt disease progression in people with macular degeneration; and slow the death of brain cells in Alzheimer’s as well as Parkinson’s patients.
Though most of these treatments are still in the early phases of human tests, a gene therapy drug to combat cancer could be available within the year. (See related story).
“There is genuine excitement in the field,” says Dr. Ronald Crystal, a gene therapy pioneer and chairman of the department of genetic medicine at Weill Medical College of Cornell University in New York.
“Gene therapy,” he predicts, “will evolve into a major therapeutic method.”
Progress amid trials
Today’s upbeat mood is in stark contrast to the gloom that pervaded the field in the late 1990s. After the rise of genetic engineering in the late ‘70s, gene therapy had been touted as a magic bullet that would quickly fix an array of debilitating and often fatal inherited ills.
It was nowhere near that simple.
The first human trial was performed in September 1990 at the National Institutes of Health in Bethesda, Md., on a young girl suffering from a rare genetic disease called ADA-SCID, in which the immune system doesn’t function properly. Healthy versions of the ADA-SCID gene were successfully added to the girl’s blood cells, but she was still taking medication for her condition and doctors couldn’t conclude that the gene was providing any benefit.
Even so, it was a breakthrough to show that genes could be added to the body -- and in the wake of that pioneering experiment, more than 450 gene therapy tests were launched, involving 4,000 volunteers.
Not one of those tests cured anyone, according to a 1995 National Institutes of Health report that was commissioned to determine where the field stood scientifically. More damningly, the report concluded that the technology had been tainted by hype, leading to “the mistaken and widespread perception that gene therapy is further developed and more successful than it actually is,” the report stated.
Scientists had been stymied by a host of unanticipated technological problems. They didn’t know how to get the genes to the sites in the body where they would do any good. They didn’t know how to make those genes function properly even if they got to intended sites. “The concept was so simple, but some of these barriers were tougher to overcome than people originally thought,” says Dr. Mark A. Kay, a geneticist at the Stanford University School of Medicine in Palo Alto.
Part of the problem was that researchers used a scattershot method of delivery: Millions of genes were infused into patients through the bloodstream, in the hope that enough genes would land where they were needed.
However, even when the genes were incorporated into the right cells -- which didn’t happen very often -- their effects were only transitory. After a couple of weeks, they’d stop working.
And the “carriers” used to ferry genes inside cells sometimes caused problems. Because naked pieces of DNA can’t penetrate cell membranes, scientists generally insert copies of the genes into viruses, which can easily enter cells. The viruses, and scientists have used various types, are stripped of their genes so they cannot reproduce or cause disease -- but, as researchers soon discovered, they can still elicit an immune response.
In a 1993 experiment, for example, scientists successfully added “good” genes to airway cells in the lungs of 10 patients suffering from the lethal inherited disorder, cystic fibrosis. But the effect was short-lived. After a week or two, the patients’ immune system recognized the virus particles as foreign and eliminated the cells, says Crystal, who conducted these experiments.
Then in 1999, an 18-year-old volunteer in a gene therapy test at the University of Pennsylvania died after a fatal immune reaction to the modified virus used in the trial. The incident cast a pall over the field and funding for research dried up. The U.S. Food and Drug Administration halted several other trials and increased its oversight, requiring far more stringent monitoring and documentation.
Yet the trials did continue.
Success, when it finally came, was tempered with sadness. In trials in France and Britain, scientists successfully corrected the genetic mistake causing X-SCID, which leaves sufferers with no infection-fighting white blood cells, in 11 young boys.
But between 2002 and 2005, three of the French boys developed a leukemia-like disease. Though the boys had been cured of their genetic disease, the inserted DNA had inadvertently switched on a cancer-causing gene. One of the children later died of complications from the leukemia treatment.
In the wake of this disaster, dozens of gene therapy trials that employed the same approach -- using retroviruses to carry genes into blood-producing stem cells -- were shut down temporarily in the U.S. and other countries. “We were on and off hold for almost two years,” says Dr. Donald Kohn, a gene therapy pioneer at Childrens Hospital Los Angeles who is in the midst of a similar study in children with ADA-SCID.
Researchers scrambled to uncover what had caused the leukemia. They tried to find better ways to safely transport genes to the right parts of the body without accidentally turning on other genes or triggering an immune reaction. And they tried to improve the chance that cells, once genes were added, would continuously secrete therapeutic doses of the desired compounds.
Though there’s still much to be done in all these fronts, significant progress has been made, scientists say.
In Europe, for example, the gene therapy protocols that caused leukemia in the children have been modified by adding chemotherapy. That stops the dangerous overproduction of white blood cells.
And researchers have improved their ability to control the genes that they insert -- restricting the genes’ activities to only certain types of cells and allowing them to remain active longer.
Scientists are also using safer viral transporters that are less likely to turn cells cancerous or trigger immune responses.
One crucial advance is the development of a new gene transporter based on a family of harmless viruses known as adeno-associated virus, or AAV. They’ve become popular DNA vehicles because, first of all, AAV viruses don’t trigger an adverse immune response.
But another benefit is that AAV comes in different types that home in on different cells. For example, one form of AAV has an affinity for nerve cells, another is attracted to the liver while yet a third type targets muscle cells. This means that scientists can select the AAV transporter based on where they want their gene to end up and it will go directly to the right place in the body, says Dr. Michael Kaplitt, a neurosurgeon at Weill Medical College who helped develop the AAV vectors.
Advances in imaging technology also make it easier to narrowly target therapies: Instead of flooding the bloodstream with millions of genes, researchers can inject small amounts of genetic material to specific regions of the body.
“This way, you don’t have to make gigantic amounts of the vectors, and there’s a safety advantage because you’re not exposing the entire body to what could be a potent agent,” says Rich Gregory, a biochemist and senior vice president of research at Genzyme Corp., the Cambridge, Mass., biotech company that has developed some of these treatments, including the experimental Parkinson’s therapy underway at UC San Francisco.
In the Parkinson’s trial, for example, the genetic material is encased in an AAV vector that is attracted to nerve cells in the brain, and injected into a discrete region of the brain that governs movement.
A similar strategy was used in another Parkinson’s experiment recently completed on 12 patients at Weill Medical College that used gene therapy to normalize the overactive nerve cells of Parkinson’s patients. A year later, the patients had a 27% improvement in stability and ability to walk, and less stiffness and tremors on the treated side of the body, says Kaplitt, who helped devise this technology.
Although some of the original obstacles have been overcome, scientists say they still have more to do.
“We’re very aware of the challenges but I don’t think it’s now being over-hyped,” says Kohn, who plans to resume his own, long-delayed ADA-SCID trials at Childrens this fall. “The field is advancing steadily if slowly.”
Gene therapy is also being tested as a treatment for angina, a debilitating condition in which the blood supply to the heart is severely impaired because of blockages to the coronary arteries. Cardiologists at medical centers around the country have injected a gene known as VEGF-2 into the hearts of 400 patients. They hope that the DNA material will spark the growth of tiny blood vessels and increase blood flow to oxygen-starved cells. (Results are expected later this year.)
And gene therapy may also improve blood flow in the legs of patients with peripheral arterial disease. In an ongoing clinical trial that will involve about 300 patients, volunteers are being given about 20 injections in each leg of a gene called HIF-1 alpha, which controls the body’s response to low oxygen, in the hope that new blood vessels will grow. In other human experiments, gene therapy is being looked at for conditions as varied as Alzheimer’s and arthritis: A preliminary trial for the latter, for example, showed a 20% to 30% reduction in swelling when 14 patients were treated with a gene to interfere with an inflammation-causing chemical.
In animals, scientists are exploring even broader possibilities, such as therapies to restore someone’s hearing, or clear clogged arteries and thus prevent heart attacks. Despite its troubled history, researchers now believe that gene therapy is finally coming of age and that DNA-based medicine will one day become an integral part of mainstream medical practice.
“The initial treatments may not be curative but will be helpful additions to the therapeutic arsenal,” says Stanford’s Kay. “And as the technology gets refined, we may move from things that merely improve quality of life to actual cures.”
For Parkinson’s patient Shirley Cooper, these advances may be coming just in time, but it is too soon to tell. She’s only the fifth patient in the world to be treated in this trial, and it is designed, primarily, to test safety. If the therapy works, however, “it could greatly prolong the time that patients get benefit from their medication,” says Dr. Chad Christine, a neurologist at UC San Francisco Medical Center and a co-investigator for the trial.
Cooper, now home from the hospital with two permanent titanium caps plugging the holes in her skull, is hoping for the best. “I just want to feel like myself again,” she says.