HIV infection causes immune cells to self-destruct, study says
- Share via
Scientists say they have discovered a key process by which the AIDS virus kills key immune cells: It triggers a preprogrammed self-destruct sequence within the cell that is intended to alert fellow immune cells of a crisis.
In papers published simultaneously Thursday in Science and Nature, researchers at the Gladstone Institutes and UC San Francisco wrote that they had not only discovered this little-understood process, but had also identified an existing drug that may halt it.
“Our studies have investigated and identified the root cause of AIDS,” said Gilad Doitsh, a coauthor of both studies and a Gladstone virologist. “Despite some 30 years of HIV research, this key HIV/AIDS process has remained pretty much a black box,” he said in a prepared statement.
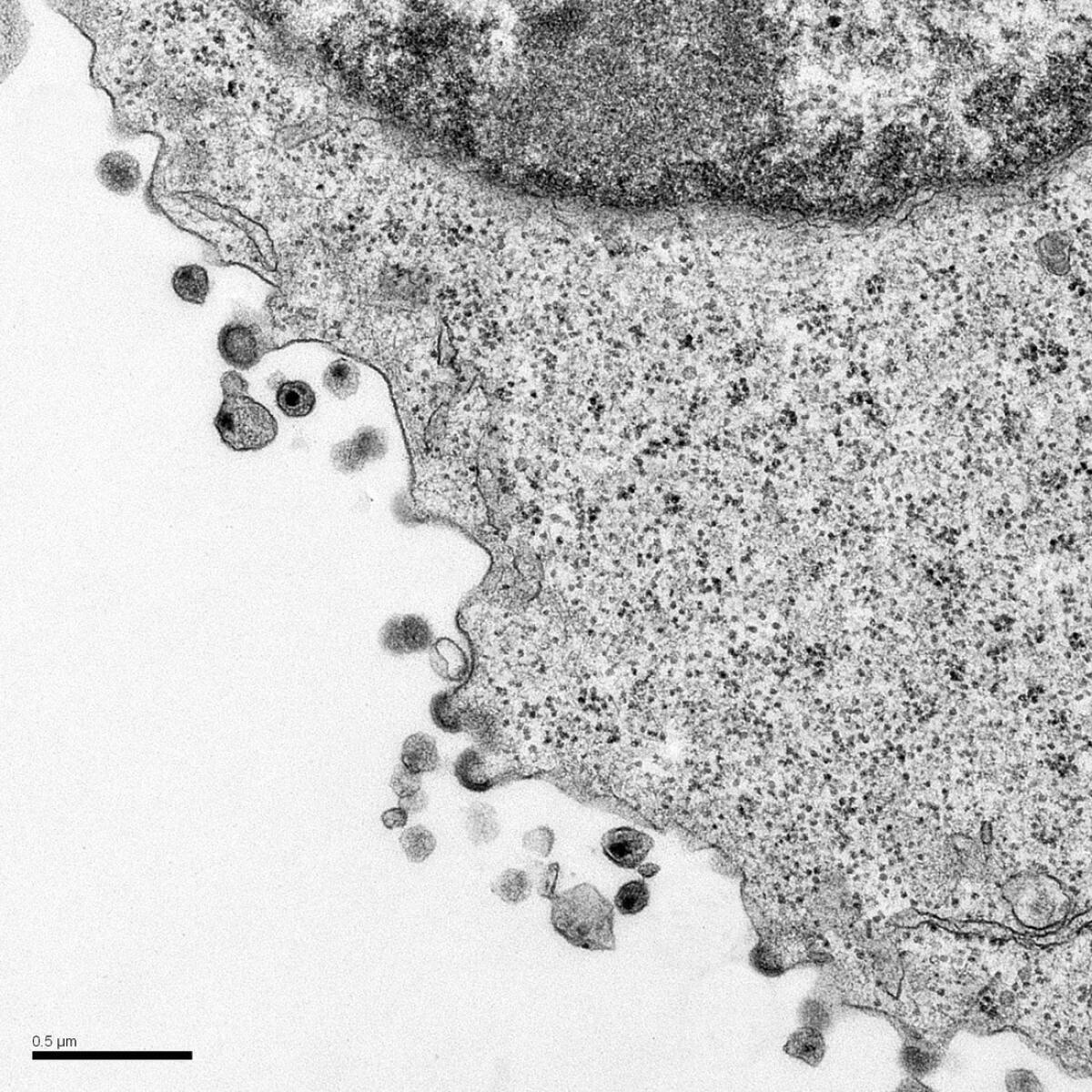
Both studies focus on the body’s CD4 T cells, white blood cells that help defend against infection. These cells are also the primary target of the human immunodeficiency virus, or HIV, which injects its own genetic material into the immune cell, causing the host cell to reproduce the virus many times over.
Yet there are many immune cells in which the viral reproduction process fails, and the host cell never becomes a reproduction factory for the virus. These cells are sometimes called “bystander” cells, and it has long puzzled scientists as to why they died, eventually leaving the body with so few immune cells that it can no longer defend itself against even minor illnesses.
Dr. Warner Greene, the senior author of both studies, and Gladstone’s director of virology and immunology research, wrote that after studying HIV infected tonsil and spleen tissues, he and his colleagues determined that the bystander cells were dying from pyroptosis, a form of cellular suicide.
Pyroptosis, which in Greek means to go down in flames, is one of a number of preprogammed self-destruction processes that cells are equipped with. In pyroptosis, a cell begins to swell and then bursts, releasing its contents, as well as inflammatory compounds. Those inflammatory compounds then attract other immune cells, which seek to fight the infection.
In the case of HIV, however, the arrival of new immune cells provides further targets for the virus, and the cycle continues.
Greene and his colleagues wrote that the cell initiates pyroptosis in response to the accumulation of viral genetic material within the cell. Although the material is unable to create new viral particles, the cell recognizes the material as a threat and essentially sacrifices itself in attempt to summon other immune cells.
“The cycle of abortive infection, inflammatory death and recruitment of new cells likely explains how this innate host response is undermined and, in fact, centrally contributes to HIV pathogenesis,” authors wrote.
Through experimentation, researchers determined that the dangerous genetic material was detected by interferon-gamma-inducible protein 16 (IFI16), which in turn activated the cell’s trigger for pyroptosis, an enzyme called caspase 1.
Armed with that knowledge, the researchers tested different caspase 1 inhibiting compounds on infected tissues and found that some were as effective in preventing the depletion of CD4 T cells as viral inhibiting drugs.
Researchers are planning a clinical trial to determine whether one of the anti-inflammatory drugs tested can help stop the progression of disease in HIV-infected people.
“It may be possible to break this pathogenic cycle with safe and effective caspase 1 inhibitors,” the authors wrote. “These agents could form a new and exciting ‘anti-AIDS’ therapy for HIV-infected subjects in which the treatment targets the host instead of the virus.”



