Patients Often Pay More of Medical Bills Than Realized : Health care: Some insurers don’t pass on savings negotiated with providers. Consumer share can be as much as half.
- Share via
WASHINGTON — Millions of Americans with health insurance who have believed for years that they were paying 15% to 20% of their medical bills have often been paying a larger share, as much as half the bill for certain kinds of services.
Most of the people affected--some covered by private insurers and others by Medicare--have been getting misleading explanations of benefits from their insurers. Information forms often fail to disclose that the health plan paid a rate sharply discounted from the retail price charged by a hospital or doctor’s office.
Instead of passing that discount on, certain health plans calculate the patient’s share of the bill based on the higher retail charge, shifting a greater percentage of the total expense to the patient.
Here’s how the math works: Suppose you undergo a simple medical procedure and are billed $1,000.
Your insurer has an agreement with the hospital that allows only $600 for the procedure. Under the controversial formula, your share would be calculated at $200, which is 20% of the $1,000. The insurer would pay $400--the difference between your share and the $600 allowance. You’ve paid 33% of the actual bill, not 20%. If your insurer gave you the full benefit of the discount, your share would be $120 and the insurer would pay $480.
The misleading billing system has shifted billions of dollars of additional costs to patients in the last few years, a disparity that is increasing. If current trends in the Medicare program continue, elderly and disabled people will pay 68% of their bills for certain hospital outpatient services by 2005. New federal estimates suggest that the camouflaged burden could shift $210 billion in costs to Medicare patients over the next decade.
Consumer groups sharply criticize the failure of insurers to share the discounts, a failure so widespread that it may affect tens of millions of Americans. In Medicare, the disputed billing method is used legally for many hospital outpatient services. But for parts of many private insurance plans, the method is under legal challenge in a majority of states. Private insurers defend their billing formulas, saying they are patterned after Medicare’s. Few of the people affected are aware that insurers are not sharing the discounts.
“Most people just don’t even know about it,” said former Texas Insurance Commissioner Bob Hunter, now director of insurance at the Consumer Federation of America. “That’s the problem. You know they have discounts and you assume the discount is being passed along to the consumer.”
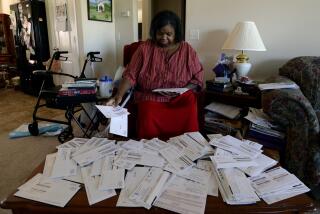
A few eagle-eyed seniors, poring over their medical bills, have picked up on the practice in the last few years and complained. Donald C. Layman, of Miramar, Fla., said he first got suspicious when a hospital tried to charge him $190 for 10 drops of eye medicine. Eventually he realized that he wasn’t getting the benefit of Medicare’s discounts, and he got the American Assn. of Retired Persons to look into it.
“I felt cheated,” said Layman, who is 77 and in failing health. “I paid 55% when it should have been 20%.”
The scope of the cost shift differs from state to state and from one insurance plan to another. Most commercial insurers apparently give beneficiaries the full benefit of discounts, but some do not.
The shift is most pronounced in Medicare and many of the state Blue Cross-Blue Shield plans, which together cover more than 100 million people--almost half the nation’s insured population.
Word of the hidden cost shift is spreading, and people across the nation are filing class-action lawsuits against private insurers. In response, the companies have argued that their contracts make clear that they don’t intend to pass along discounts. People haven’t been reading the fine print, they say.
The insurers also argue that charging sick people more helps everybody covered by a particular policy. By lowering insurers’ costs, the disputed method helps keep premiums down. Georgia Sen. Sam Nunn has described the system as a massive transfer of money from the sick to the healthy.
AT&T; has sued 17 Blue Cross plans across the country, accusing them of overcharging its employees by not sharing discounts. The company and the plans reached a settlement this year that the insurers insisted be kept confidential.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.