Medicare, FDA agree to share data
- Share via
WASHINGTON — Two major government health agencies that have traditionally operated as self-contained bureaucratic fiefdoms announced a joint venture Thursday that promises to improve prescription drug safety for all Americans, while potentially reducing wasteful spending on medications.
The Food and Drug Administration and Medicare agreed on rules for using information from Medicare’s giant claims databases to create a computerized early-warning network for problems with medications and medical devices that come to light after they go on the market.
Though Medicare will not turn over individual patients’ data to the FDA, the two agencies’ computers will now be able to talk to each other, in effect, to pose and answer questions that may reveal potentially risky side effects in new drugs. Since pre-market testing usually involves a limited number of patients, serious problems sometimes become evident only after hundreds of thousands of people begin using a product.
The new system, called the Sentinel Initiative, will eventually include private insurers as well, to fill in information gaps about drugs that elderly patients don’t use, such as contraceptives.
The FDA’s current early-warning system is nowhere near as comprehensive as the new system is expected to be. It relies on self-reporting by drug makers, hospitals and doctors, and is believed to capture only 1% to 10% of problems. Since the elderly are the major consumers of medications, Medicare’s trove of inpatient, outpatient and prescription plan data is considered particularly rich.
Health and Human Services Secretary Mike Leavitt compared the FDA’s current safety system to “looking at the stars from your backyard with the naked eye.” The new system will provide a precise telescope, he added, and “you will see the stars trying to send you messages.”
Setting up the network will not entail any major new expense for technology, officials said. Instead, the main task involves getting data experts from both agencies to work together under a mutually agreed-on framework.
Sentinel could save money, said Kerry Weems, acting administrator of the U.S. Centers for Medicare and Medicaid Services, citing estimates that the cost of treating preventable drug reactions in the elderly is as high as $900 million a year.
“Our understanding of how well drugs work and how safe they are for the elderly or disabled has been limited,” Weems said. “Clinical trials often exclude the very old, patients with multiple chronic conditions, and those taking multiple medications. Those cohorts comprise the vast majority of Medicare beneficiaries.”
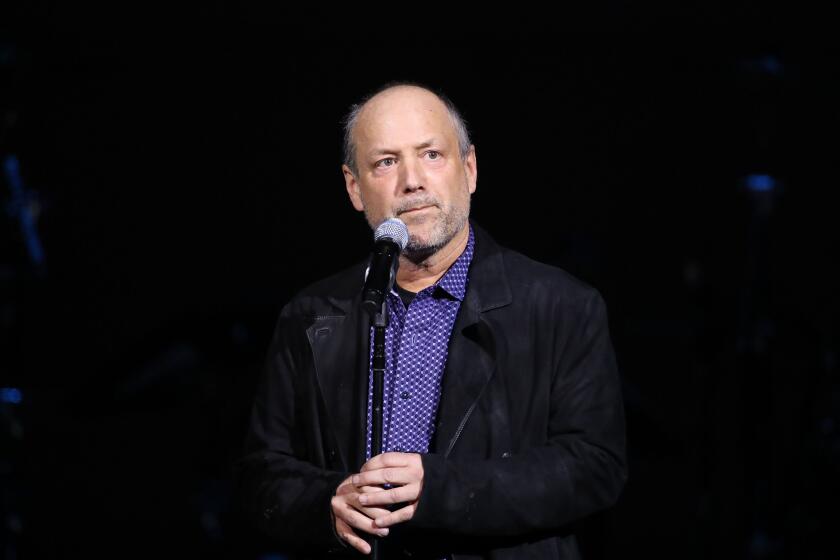
While collaboration between the FDA and Medicare sounds simple, it has taken years to bring this plan to fruition. The concept got a major push earlier in the Bush administration from Mark B. McClellan, who served as FDA commissioner and later as Medicare administrator. Congress included it in drug safety legislation passed last year.
The new system could shorten the time it takes to detect drug safety problems from years to months, McClellan said in an interview. “What will be possible with this broader framework will be much larger-scale analysis,” he said. “It has the promise to detect potential problems far more quickly, and you can also learn about risks to particular groups of patients.”
There has been relatively little criticism of the new approach.
However, privacy advocates are expected to scrutinize the rules for information-sharing between Medicare and the FDA, which will take effect in 30 days. And drug companies have expressed some concern, arguing that studies of large populations of patients in the real world are not as precise as controlled clinical trials, and could generate false alarms.
Janet Woodcock, who heads the FDA center that reviews new drugs, acknowledged that possibility but said the alternative was worse.
“We completely understand and agree that getting information in this way isn’t as free of bias as what we get in a clinical trial,” she said.
“However, in most cases, we don’t have any way of getting this information at all right now.”
The FDA is working on standards for interpreting the data, and Woodcock said she hoped that would reduce the chances of false alarms.
One of the major uses of the Sentinel network will be to address lingering doubts about new medications, Woodcock said.
For example, suppose that pre-approval clinical trials had raised suspicion that a new drug might pose a particular kind of risk, but not enough information could be gleaned from the trials to resolve the question with certainty.
In such a case, Woodcock said, the FDA would query the Medicare databases to see if patients who took the medication had bad reactions. The agency would get statistical answers, but no information on individual patients. However, public health agencies have authority under other federal laws to obtain private information in an investigation.
“Say we had a some hint or report that there was some adverse event that was distinctive,” said Woodcock. “We could take that signal . . . and do a study. Though it wouldn’t answer all the questions, it would provide a much better source of information, probably pretty rapidly.”
--
ricardo.alonso-zaldivar@ latimes.com
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.