Lazarus: Patients’ choices narrower, yet cost of insurance rises

- Share via
It’s hard enough having a serious condition like cancer or kidney failure. It’s even worse, some might think, when your health insurer says you have to buy your medicine from the pharmacy of its choice — or pay the full amount for expensive life-saving drugs elsewhere.
Yet that’s precisely what Anthem Blue Cross is telling people who require so-called specialty medicines, which are used for complex conditions and can cost thousands of dollars a month.
As of Jan. 1, the insurer says, such people can either buy their drugs from the mail-order pharmacy CuraScript or pay full fare at a retail drugstore.
“Using a retail pharmacy will be considered going out-of-network,” Anthem says in a letter being sent to many users of specialty meds. “And your plan doesn’t have coverage for that. So you’ll have to pay the full price of the drug.”
Jacques Liberman, 57, of Cathedral City received one of the letters the other day. He is HIV-positive and takes a drug called Atripla to help prevent his condition from transforming into full-blown AIDS.
Atripla, jointly made by Bristol-Myers Squibb and Gilead, isn’t cheap. It costs about $60 per pill and has to be taken every day. That’s at least $1,800 a month.
In Liberman’s case, Anthem covers part of his prescription-drug costs. After that, he relies on an AIDS Drugs Assistance Program funded by state and federal dollars.
Quiz: Test your healthcare knowledge
What Liberman resents most is the loss of personal freedom.
“Who is Anthem to tell me where I have to buy my medicine?” he said. “Why should I have to buy it from some mail-order company instead of the drugstore that I have been going to for a long time?”
These are fair questions. The answers, however, are complicated and cut to the heart of our country’s healthcare system.
Put simply, the practice of an insurer dictating terms to patients is the price we pay for an employer-based insurance system under which for-profit companies negotiate terms to keep costs down.
If that denies consumers the ability to choose where and when they’ll shop or to know the actual price of medical treatment, tough patooties.
“I’d love a more transparent healthcare market,” said Craig E. Thompson, executive director of the AIDS Project Los Angeles, a nonprofit group that advocates on behalf of people with HIV/AIDS. “I’d love to know how much healthcare actually costs.
“But as long as I’m OK with having an insurance plan from my employer, I have to be OK with that insurance company telling my employer that I have to buy specialty drugs from a mail-order pharmacy.”
Thompson also is HIV-positive, and as an Anthem customer, he too faces the prospect of having to buy his meds from CuraScript as of the first of the year. But he feels none of Liberman’s outrage.
Insurers and employers have to do whatever they can to keep medical costs down, Thompson said. Otherwise we’d see even higher premiums, co-pays and deductibles.
He also believes that mail-order pharmacies with experience in specialty drugs are best-suited to handle such prescriptions.
“These medications are fairly complicated,” Thompson said. “I’m not sure every pharmacy should be dispensing these drugs.”
It sounds as if he’s making the best of a bad situation. I asked Thompson which he’d prefer if he had a choice: our current employer-based insurance system or a single-payer, Medicare-for-all system.
He didn’t hesitate.
“A single-payer system would definitely be best,” Thompson said. “That would eliminate a lot of these problems.”
Darrel Ng, an Anthem spokesman, said that buying specialty drugs in bulk and mailing them directly to people’s homes will save money.
“We think this is important at a time when businesses and individuals are deciding whether they can afford to continue to maintain health benefits coverage,” he said.
This is healthcare as practiced by Gordon Gekko: back-room negotiations and sweetheart deals. It may result in lower costs, but the patient is practically an afterthought in the equation, a line item on a business contract.
And we’ll see more of this sort of thing as consolidation continues among healthcare companies, allowing fewer businesses to exert greater control over the market.
CuraScript, for example, is owned by Express Scripts, the country’s biggest pharmacy benefits manager. Such companies serve as middlemen in helping insurers and employers handle prescription-drug programs.
Express Scripts acquired rival Medco Health Solutions last year for $29 billion. That deal followed similar buyouts of ValueRx, Diversified Pharmaceutical Services and National Prescription Administrators.
Express Scripts now accounts for almost 1 of every 3 prescriptions written in the United States.
Anthem Blue Cross, meanwhile, is owned by WellPoint, which runs Blue Cross or Blue Shield operations in more than a dozen states.
WellPoint, the country’s largest private health insurer, acquired rival insurer Amerigroup for nearly $5 billion in July. Other recent purchases include contact-lens retailer 1-800 Contacts and CareMore, a provider of managed care for the elderly.
So let’s return to Liberman’s questions. “Who is Anthem to tell me where I have to buy my medicine?” he wanted to know. “Why should I have to buy it from some mail-order company instead of the drugstore that I have been going to for a long time?”
Anthem is a corporate behemoth whose parent earned $2.6 billion in profit last year by managing people’s insurance claims while charging as much as possible in premiums and co-pays.
The company is now seeking an average 18% rate hike for more than 630,000 individual policyholders in California, with some customers facing increases of as much as 25%.
Liberman and others who need specialty meds have to use the drugstore of Anthem’s choosing because, well, that’s in Anthem’s best interest. It’s likely in the patients’ best interest as well, at least as far as costs go.
But Liberman also is correct: Personal choice is important. When it comes to healthcare, nobody should have decisions forced upon them.
What will our healthcare system look like when we have even fewer options for coverage and prescriptions? Think about the cable industry and how that’s turned out after decades of consolidation.
Bummer, huh?
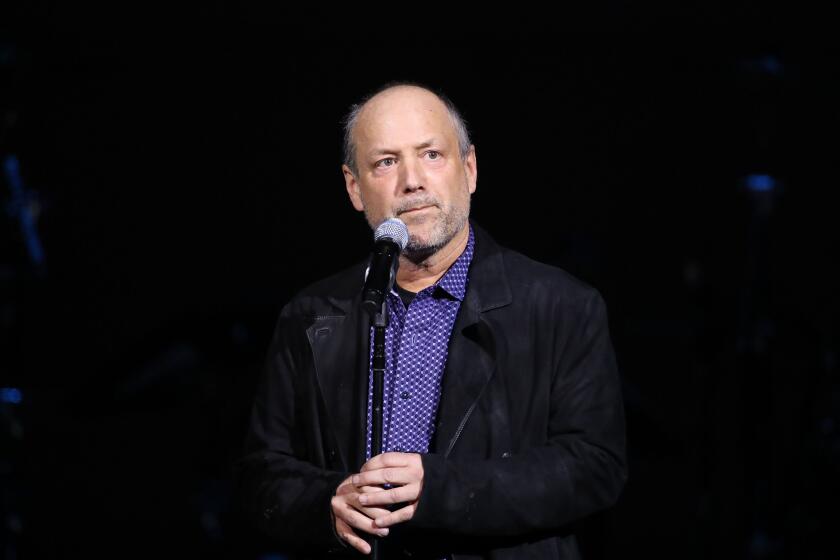
David Lazarus’ column runs Tuesdays and Fridays. He also can be seen daily on KTLA-TV Channel 5 and followed on Twitter @Davidlaz. Send tips or feedback to david.lazarus@latimes.com.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.