Millions of Americans are about to lose their healthcare coverage. Many have no idea

- Share via
Millions of Americans may have breathed a sigh of relief when the federal government declared the national pandemic emergency to have ended as of May 11.
That doesn’t include Medicaid advocates and millions of Medicaid enrollees, however. The reason is that the end of the emergency meant the end of rules protecting those enrollees from losing their coverage for any reason.
As a result, 15.5 million people will the thrown off Medicaid, according to an estimate from the Congressional Budget Office. Of that number, 6.2 million will become uninsured. That may be a conservative figure; the healthcare research organization KFF estimates that as many as 24 million people may lose their Medicaid coverage.
We are expecting children to take the biggest hit here. They’re not going to have somewhere else to go.
— Joan Alker, Center for Children and Families, Georgetown University
According to the Center for Children and Families at Georgetown University, as many as 6.7 million children alone may lose their Medicaid coverage, leaving them “at considerable risk for becoming uninsured for some period of time,” the center says.
“We’ve been worrying about this for more than two years,” says Joan Alker, the center’s executive director. “We are expecting children to take the biggest hit here. They’re not going to have somewhere else to go.” That’s because many of the low-income families that are Medicaid’s core clientele don’t have access to employer-sponsored health coverage for children.
Get the latest from Michael Hiltzik
Commentary on economics and more from a Pulitzer Prize winner.
You may occasionally receive promotional content from the Los Angeles Times.
The CBO projects that the nation’s uninsured rate, which has fallen to 8.3% this year, will ratchet back up to 10.4% in 2029.
In stark terms, the U.S. is replacing one public health crisis — the COVID-19 pandemic — with another.
What has Medicaid advocates especially concerned is the high percentage of enrollees already getting kicked off the program not because of formal determinations of ineligibility (typically because their incomes have come to exceed state thresholds) but for “procedural” reasons.
These generally involve a failure to complete or submit renewal paperwork. That can happen because the enrollee has moved sometime in the last few years and thus never received a renewal application, or was confused by the application or mistook it for junk mail and ignored or discarded it.
“There are myriad ways the procedure can go awry,” Alker told me. The state might be mistaken in determining ineligibility. Applicants may have trouble obtaining help from call centers via overloaded phone lines. In many states, backlogs in processing renewals can stretch into weeks or months, while eligible families struggle with uncovered bills. Some may not know they’ve been disenrolled until they try to renew a prescription at a drugstore, only to be told their pills are no longer covered.
Pressure to end COVID-19 emergency rules is way premature.
Since disenrollments began earlier this year, 73% of disenrollments have been due to procedural reasons, according to the enrollment and unwinding tracker maintained by KFF, compiled from data from the 32 states that have submitted reports to the government. That translates to 2.72 million out of the 3.72 million Medicaid enrollees thrown out of the program as of July 25. An undetermined number may still be eligible.
Let’s step back for a primer on how this situation came to be.
It started with the Families First Coronavirus Relief Act, signed by President Trump in March 2020 as the first relief package addressing the pandemic. Among the act’s provisions was a bump of up to 6.2% in the federal share of Medicaid costs, to last through the end of the pandemic emergency.
In return for the money, the states had to commit to freezing eligibility standards at pre-pandemic levels and to maintaining “continuous coverage” — they couldn’t disenroll anyone from Medicaid unless the enrollee consented or moved out of state.
That put a halt on customary annual eligibility tests that were written into state rules, though often weakly enforced.
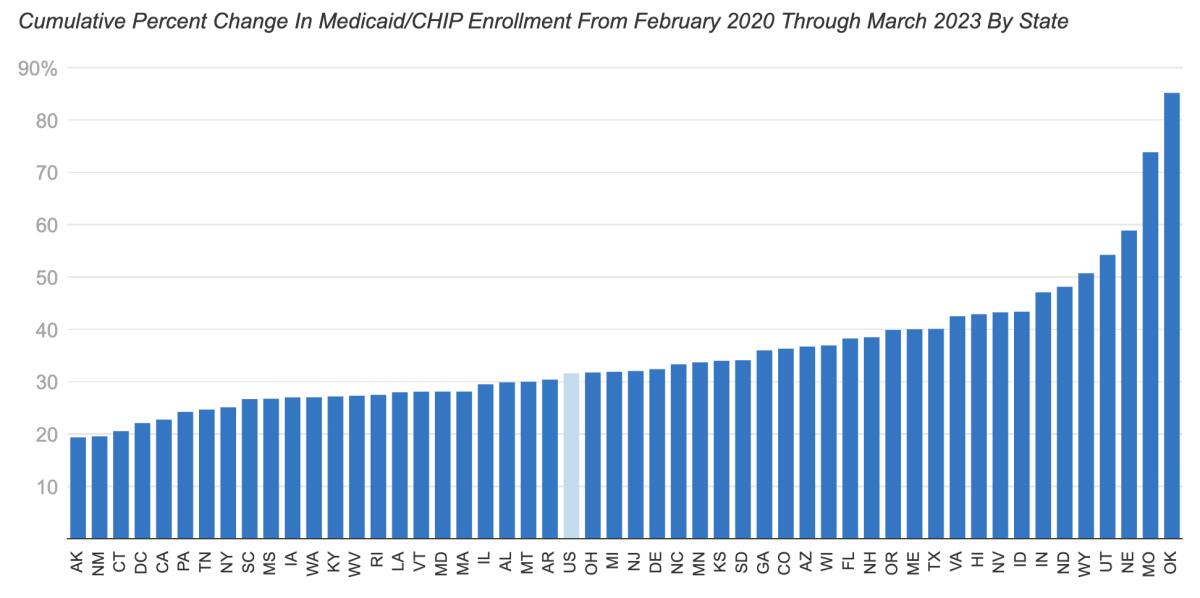
The rule changes were a boon to public health during the COVID-19 crisis. Enrollment in Medicaid and its Children’s Health Insurance Program (CHIP) grew by 21.2 million, or 29.8%, from February 2020 through December 2022, with the caseload increasing in every state.
The budget bill signed by President Biden in December set an expiration date of March 31 for the continuous coverage provision. States were given up to 14 months after April 1 to complete the process. The great unwinding was cleared to begin.
Every state is grappling with the complexities of turning the clock back on Medicaid. In every state, it’s likely that tens or hundreds of thousands of enrollees at least will be tossed out of the program.
Some states are launching that process with rather more enthusiasm than others. That category includes Arkansas, where Republican Gov. Sarah Huckabee Sanders has boasted with great glee about having launched the unwinding on May 1. Under a state law enacted before she took office, Arkansas must complete disenrollments within six months, not 14.
“This is the fastest pace in the nation,” Sanders crowed in an op-ed for the Wall Street Journal. “I’m proud Arkansas is leading the nation in getting back to normal. ... As other states end temporary pandemic measures, they know where to look for guidance.”
Sanders told a lie about her state’s process, however. “We’re simply removing ineligible participants from the program to reserve resources for those who need them and follow the law,” she wrote.
The state’s own figures contradict her. As of the end of June, according to “unwinding” reports the state submitted to the federal government, only about 35,300 of the 171,025 Arkansans thrown off its Medicaid program lost their coverage because they were deemed ineligible.
The rest — 135,700, or about 80% — were disenrolled for procedural reasons. Some may indeed be ineligible, but obviously the state can’t know that. More than one-third of the Arkansas disenrollees are children; many of them are likely to still be eligible, because the income limits for children are higher than they are for adults. Right off the bat, Arkansas disenrolled 11,000 newborns.
That may not be surprising, because Arkansas has long had a documented hostility to Medicaid. It was the only state to implement work requirements for the program. Its rules resulted in the disenrollment of 17,000 Arkansans between 30 and 49 years of age in the first phase of the rollout, a toll that was so unexpected that a federal judge ordered the effort stopped.
Hiltzik: Confirmed--Medicaid work rules are a health disaster for the poor and don’t produce jobs
Ever since Arkansas implemented its first-in-the-nation work requirements for Medicaid in June 2018, the state has functioned as a laboratory for the concept of placing unnecessary obstacles in the way of low-income people seeking health coverage.
The same judge blocked several other states that were poised to implement similar rules. The Biden administration rescinded Trump’s approval of Medicaid work requirements in every state shortly after taking office.
Arkansas was one of 14 states to start disenrollments in May. Four others — Idaho, South Dakota, Oklahoma and New Hampshire — started in April. Twenty states and the District of Columbia started in June and 11, including California, this month.
The toll is mounting because after three years of continuous coverage, the relaunch of eligibility testing has created chaos at state Medicaid agencies. In California, as my colleague Emily Alpert Reyes reports, 225,000 Californians have been disenrolled, nearly 90% for procedural reasons, in just the first two or three weeks of July.
The figure includes more than 34,000 households in Los Angeles County — an estimated 30,000 of which have lost coverage because their paperwork was not received or processed by the county in time. The actual number of individuals affected is certain to be much higher.
It’s fair to say that the eventual end of the pandemic emergency was always pre-ordained, if not its timing. That doesn’t make the chaos afflicting the vulnerable Americans dependent on Medicaid any less disgraceful.
Medicaid is the nation’s largest healthcare program, with a caseload of 93 million. It may not be perfect, but its value to beneficiaries is indisputable. Among other things, the program’s expansion under the Affordable Care Act has accounted for one-third to one-quarter of the decline in personal bankruptcy filings.
The nation is now poised to walk back the gains in health coverage that were achieved during a horrifically challenging public health emergency. Can any rational person explain why?
More to Read
Get the latest from Michael Hiltzik
Commentary on economics and more from a Pulitzer Prize winner.
You may occasionally receive promotional content from the Los Angeles Times.













