Starved for normality
- Share via
Bryan Bixler is dying.
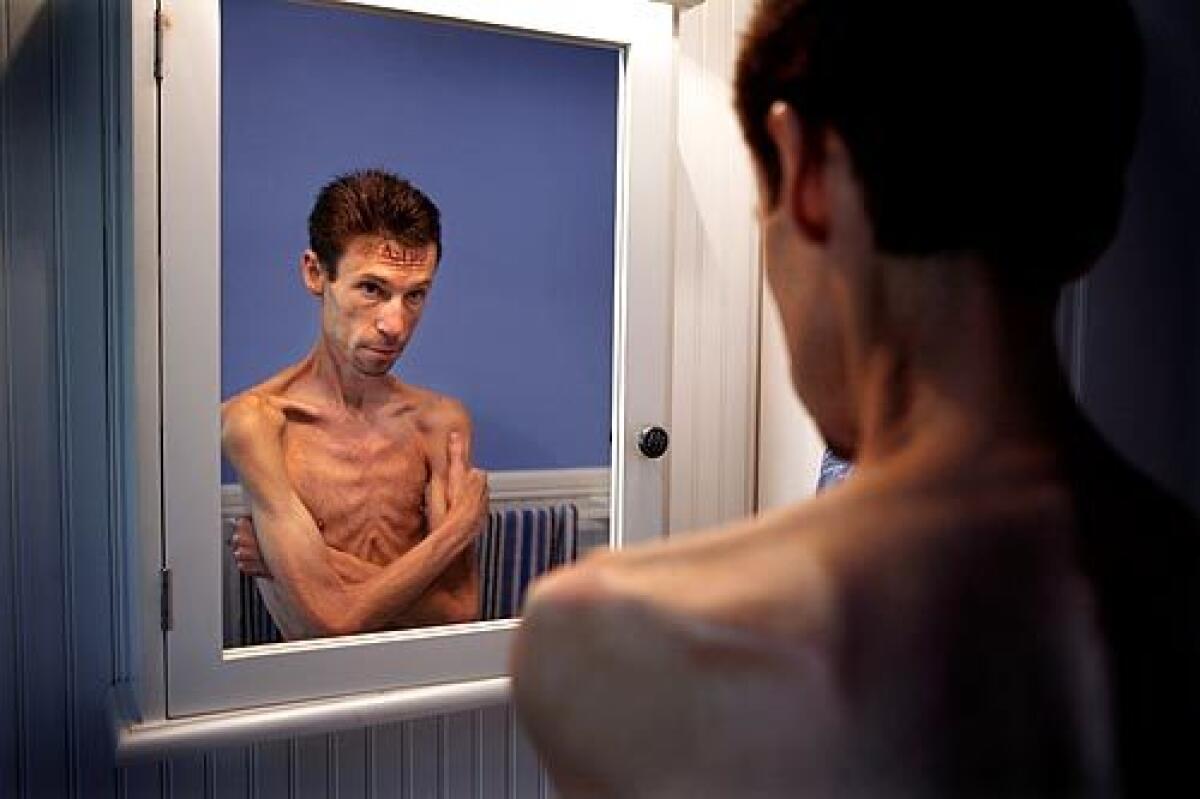
He feels it in his bones a little more each day, as if passing the mirror in his Laguna Beach apartment and glancing at himself isn’t evidence enough. Here’s what greets him: sunken eyes, paper-thin arms and legs that hang like a puppet’s, the slow-motion gait that he fears will define his movements for the rest of his days. What happened, he wonders, to that young man who once ran half-marathons?
It’s all so crazy. That’s what he tells himself. Dying a bit more every day and knowing how to fix it but being unable to do it. Knowing that if he would just start eating like a normal person, he’d give himself a fighting chance.
But he’s not a normal person, not anymore. Not at 5 feet 9 and 82 pounds. Not when he’s got a master’s degree and knows how the body works and yet can’t make himself fix spaghetti or drink a chocolate malt.
Bixler is 39 and anorexic, suffering from an eating disorder traditionally associated with young women but which generally has been thought to include a 5% to 10% male component. In recent years, however, some researchers suggest that figure may be approaching 15%.
He doesn’t remember a day or week or month that he turned the corner and inexorably headed down the path to anorexia nervosa, but he and family members think it was a slow-moving journey that started in his teens. He remembers those years as a time when his parents went through a difficult divorce and he was simultaneously caught up in the fitness craze and bent on avoiding junk food.
“I was Mr. Healthy,” he says. “I was a vegetarian, I wanted to be a runner. Before I knew it, I lost weight without realizing it.”
As he moved through his 20s, the disorder plunged him into what he calls “the vortex,” a swirling downward spiral of weight loss and a deepening inability to reverse course.
But if there was a time back then when Bixler either denied he was anorexic or thought people were overreacting to his looks, those days are gone. “I see when I look in a mirror a walking caricature of a human being,” he says. “A skeleton.”
But what’s different now than, say, even a year or so ago is a new resoluteness. The most primal cause of all.
“I want to live,” he says.
To do that, he believes, he needs intensive coordinated treatment at an eating disorder center. Bixler’s Medi-Cal insurance would pay for medical help and psychiatric or psychological treatment -- through care providers Kaiser Permanente and the Orange County Health Care Agency -- but not for long-term coordinated treatment at an eating disorder clinic.
The gap between what he needs and what his insurance will cover has been played out around the country. Many insurance companies increasingly have questioned the need for long-term residential treatment programs and balked at paying the high costs for them.
Seven years ago, with his parents footing the bill, Bixler spent several months at a treatment center in Wisconsin. Even though his weight climbed from 92 pounds to 120, he considered it a prison. When his parents’ money ran out, he left and immediately relapsed.
Last fall, Bixler returned to the Wisconsin center but stayed only six days. Assigned to a psychiatric unit, he refused treatment, and his parents told him they could no longer afford the bill.
Since then, Bixler insists, he’s seen the light and would stay in a long-term treatment program as long as it took. The only other option, he says, is death. “Obviously, my way is not working.”
Neither is the limited psychological or psychiatric care he can get through Medi-Cal, says Terry Schwartz, medical director at an eating disorders program at UC San Diego. She supervised a recent psychiatric exam of Bixler, which he requested in the hope that it would bolster a claim he’s made with the state for increased Medi-Cal coverage. The claim is pending.
Bixler isn’t at an acute stage, Schwartz says, but his laboratory results and weight put him at “high risk” of dying from anorexia. American Psychiatric Assn. guidelines alone, she says, put him in the category of someone who needs either inpatient or residential care.
What he needs is a coordinated program that would run the gamut of medical, psychological, psychiatric, nutritional and dietary treatment. Bixler would be most vulnerable, she says, to sudden cardiac death or an inability to fight off an infection because of his depleted white blood cell count.
While convinced it’s nowhere near what he needs, Bixler still avails himself of the counseling services offered through the county and Medi-Cal. If nothing else, he reasons, it’ll perhaps send a signal that he’s trying to play ball.
On his more charitable days, Bixler tries to avoid recriminations.
“I’m not blaming anybody,” he says, “not Kaiser, not the county. I try not to blame myself, because of course I feel like I caused it. For me, it’s the anger, the sadness that a life doesn’t mean anything unless you have money.”
In his 20s, before he fully grasped what was happening to him, Bixler saw a future for himself. With degrees from UC San Diego and the University of Georgia, Bixler wanted to work in the education department of zoos or aquariums. Instead, the eating disorder overtook him, and after short stints at two zoos and teaching while a graduate student, he went on full-time disability nine years ago.
He subsists on Social Security and lives in a studio apartment with a view of the Pacific Ocean, the beneficiary of cheap rent because his parents own the building.
He typically sleeps until late morning and stays up late. His sister, Kimberly Leeds, thinks that’s so he can avoid normal social contacts and justify living his life mostly in the night.
She’s the one who pulled his shirt over his head about 15 years ago and made him look at his rib cage. “Look at yourself,” she said. “How can you think you’re OK?”
Even though she understands the disorder, her brother’s eating habits both cause her to marvel and madden her.
“He will not eat any dairy, but he eats frozen yogurt all the time,” she says. “He won’t eat certain lettuce because it gets caught in his teeth, but he will eat iceberg lettuce. He’ll eat popcorn all night long but won’t eat roast beef because it sticks in his teeth.”
If they go out to eat, she says, “He can’t order something off the menu. There are about five or six statements that have to go along with it.” Forget rice or beans, if that comes with the entree. He has to have shredded lettuce and cilantro on the side. He will eat vegetables and protein foods, but carbohydrates are a non-starter, she says.
Leeds may be frustrated, but she hasn’t given up on her brother. To the contrary, she’s joined him in his fight to get more extensive care.
Their parents, she says, have been dealing with the situation for half of Bryan’s life and it is wearying.
“Mother feels like she’s done everything. She’s mentally, physically and emotionally exhausted,” Leeds says. “Her life has been dedicated to him for the last 20 years.”
All of which Bixler knows and which makes him sigh.
His father tells him he’s not trying hard enough. What’s so hard about fixing a bowl of oatmeal and eating it? They have shelled out the money before and might again, but the failing economy has hurt their finances.
“They blame me, their blame reinforces my own self-blame,” he says. “I’m my own worst critic. I look in the mirror at night, saying I’m insane. What’s wrong with me?”
He knows the answer, of course: a disorder with numerous dark corners that enveloped and then overwhelmed him.
“I can’t understand why I can’t do what a 6-year-old can do -- feed myself.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.