Having to think about the unthinkable
- Share via
“I could show you case after case,” said Dr. Neil S. Wenger. “I could bet you million-to-1 odds these patients would not want to be in this situation.”
He was talking about patients in critical condition who are “attached to machines, being kept alive” in hospitals, many of them suffering.
A common reason for that, said Wenger, director of UCLA’s Health System Ethics Center, is that fewer than one-third of us make our healthcare wishes known in advance of critical illness or injury. So if we end up comatose after an accident, or with severe memory loss in old age, we’re kept alive, regardless of the cost and regardless of what our wishes might be or how grim the prognosis.
It’s understandable. Nobody wants to think in advance about life ending. In our satisfied state of denial, we want to believe medical advances will keep us healthy until we die in our sleep at a ripe old age. But death doesn’t always come on our terms, and failing to face up to other possibilities can put crushing burdens on loved ones — not to mention that soaring end-of-life medical costs are at the center of the national budget crisis.
“We use healthcare resources far out of proportion to any other country on the planet,” said Wenger, who researches elder care for the Rand Corp. “We need to have a conversation about where society wants to put its resources [and we] might decide there are certain kinds of life extension that are not as important to us as educating kids and having adequate infrastructure.”
Of course, none of us individually can solve all of these societal issues. But there are things we can do to make our own situations better at the end of life. It’s never easy to think about your own demise, or the demise of those you love, or to start uncomfortable but necessary conversations about death. But since my father’s health began to deteriorate this summer, I’ve talked to many medical people who say we need to get over our fears. Today, I’m passing along their advice. Consider it your guide to the final frontier.
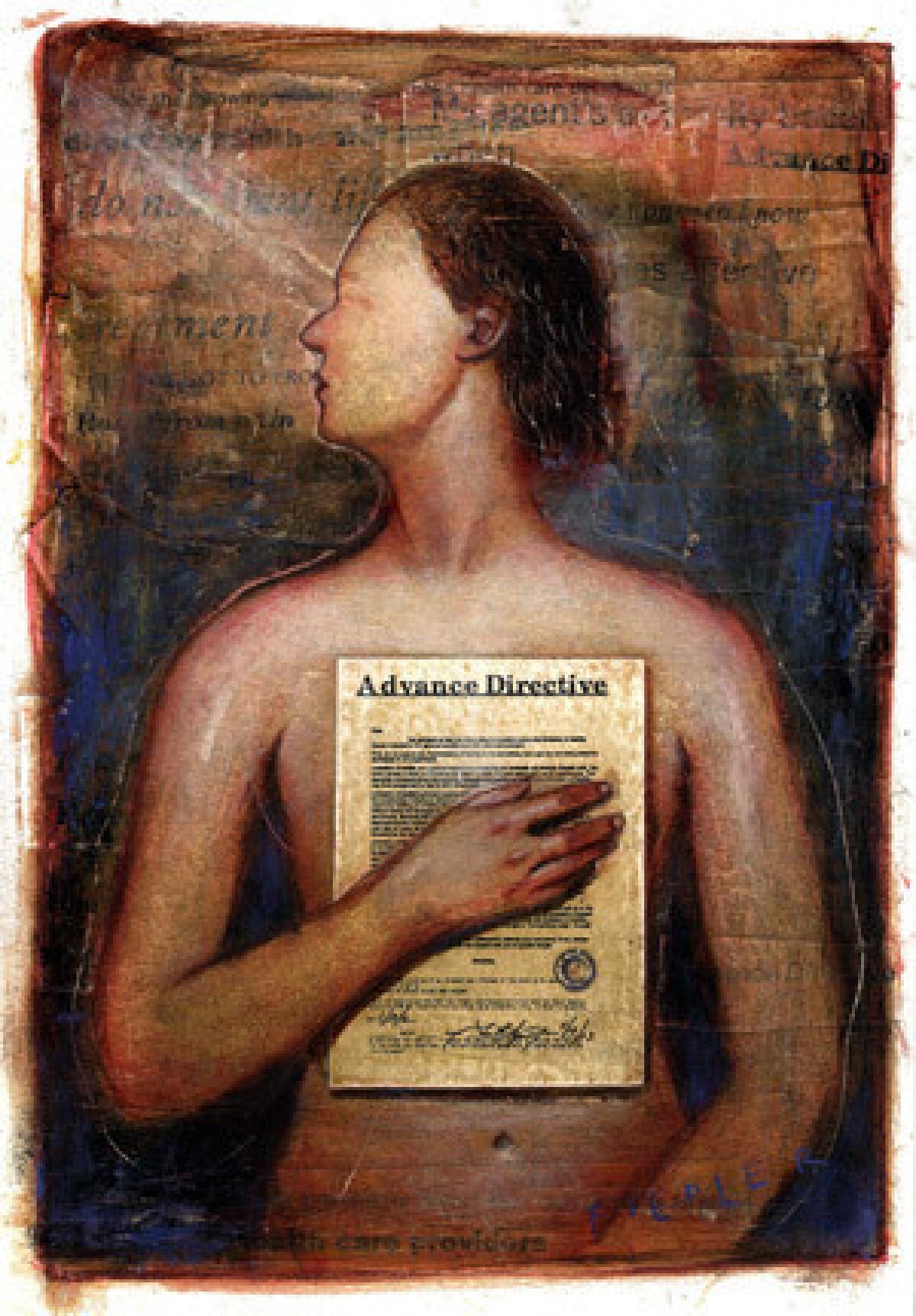
One of the first decisions to make — in advance of any crisis — is whom you want making healthcare decisions if you’re unable to do so on your own because of illness or injury. And that has to be done in writing.
Judy Citko, executive director of the Coalition for Compassionate Care of California, advises completing what’s known as an Advance Healthcare Directive. An easy way to learn more about this is to visit her nonprofit agency’s website, https://www.coalitionccc.org, which is loaded with good information on planning. And no matter what state you live in, you can get an Advance Healthcare Directive by going to Caring Connections at https://www.caringinfo.org.
The California form, which doubles as a living will, is free and can be printed from the website. On it, you can authorize a loved one or someone else to have power of attorney — or serve as your agent — to make healthcare decisions for you if you’re unable. You can indicate whether you want your life “to be prolonged as long as possible” or, alternatively, that you don’t want your life “to be prolonged if the likely risks and burdens of treatment would outweigh the expected benefits.”
The directive is valid if signed by a notary public or by two witnesses. Another directive, known as Five Wishes, can be purchased online, and an explanation of how it works and where to get one can be found on Citko’s website.
She also recommends that people with advanced illnesses talk to their doctors about a form known as POLST, or Physician Orders for Life-Sustaining Treatment, in which patients can indicate whether they want resuscitation, feeding tubes, ventilators and other life-sustaining procedures. The form is usually bright pink to make it easier for emergency responders to locate.
Doctors tell me that a lot of patients say they’ve signed one form or another, but can’t remember exactly what it was or where it is. So be sure to keep the person you’ve designated as your agent informed about your directives, make several copies and file one with healthcare providers. And make sure to include enough information. I’ve heard many complaints from patients and doctors that even though forms had been filled out, the patients’ intentions are unclear.
Wenger says it’s better to avoid listing medical procedures you do or don’t want and instead list limitations and compromises you’re not willing to endure. A patient might say “no feeding tube” but then be in a situation in which a temporary feeding tube could help return him to relatively good health.
In the spaces provided on the directives, Wenger said, you might write, “I would not be willing to live in a state where I can’t recognize the people who are important to me…or where I can’t be independent” in managing personal hygiene.
Families should also do their homework on where they want to receive care, said Dr. Bruce Chernof of SCAN, a Long Beach foundation devoted to improving medical and human services for senior citizens.
“Families spend a lot of time thinking about choices when it comes to things like maternity decisions,” said Chernof, and they should do the same for elder care, whether it’s an outpatient service, a hospital or a nursing home.
Medicare patients can qualify for free in-home hospice care — which includes a wide range of palliative care and services — if they have chosen to forgo curative interventions and a doctor concludes they are likely to be in the last six months of life. Palliative care is also available to those with a serious illness who will continue to receive treatment either in a hospital setting or at home. And rather than think of these programs as death sentences, think of them as a way to get the most out of the rest of your life. Palliative and hospice care can be cheaper than traditional care, but patient satisfaction and even life expectancy are often higher than in traditional care.
If nursing homes are a consideration, you can find ratings at https://www.medicare.gov/nhcompare, and if you’d like to locate an elder-care attorney or find links to other information on aging, go to https://www.aging.ca.gov.
None of this is pleasant business, for sure. But keep one thing in mind:
There’s a better chance of avoiding taxes than that other thing.
To read more of Steve Lopez’s columns on this subject or to share your stories about the end of life go to https://www.latimes.com/lifeanddeath
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.











