Coronavirus Today: The isolation conundrum
- Share via
Good evening. I’m Karen Kaplan, and it’s Tuesday, Aug 9. Here’s the latest on what’s happening with the coronavirus in California and beyond.
There are so many things we still don’t understand about COVID-19, and one of the most perplexing is knowing when it’s safe to stop isolating after a positive coronavirus test.
The guidelines from the Centers for Disease Control and Prevention are clear. In most cases, you can rejoin the world after five full days as long as you satisfy two key criteria — you have to be fever-free for at least 24 hours without the aid of medicine, and your symptoms have to have improved since your initial diagnosis. (If you are immunocompromised or you became severely ill, the CDC advises you to isolate for 10 days.)
If you exit isolation after Day 5, you should continue to wear a mask when you’re around other people through the end of Day 10. But what you won’t have to do, according to the CDC, is test negative for a coronavirus infection.
The state of California disagrees. According to the Department of Public Health, the soonest you can end your isolation is the end of the fifth full day. But officials in Sacramento want you to have a negative test as well. If you don’t, you’ll need to remain in isolation until you do.
Which policy is right? The answer depends on whether you’d rather make people spend several extra days holed up in a room even if chances are good that they’re no longer contagious, or if you’re willing to take the chance that some seemingly recovered patients who rejoin the world might still be infectious (though, if they’re following state and federal guidelines, they’ll be wearing a well-fitting mask).
The problem is that scientists don’t know how much to trust a coronavirus test under these circumstances.
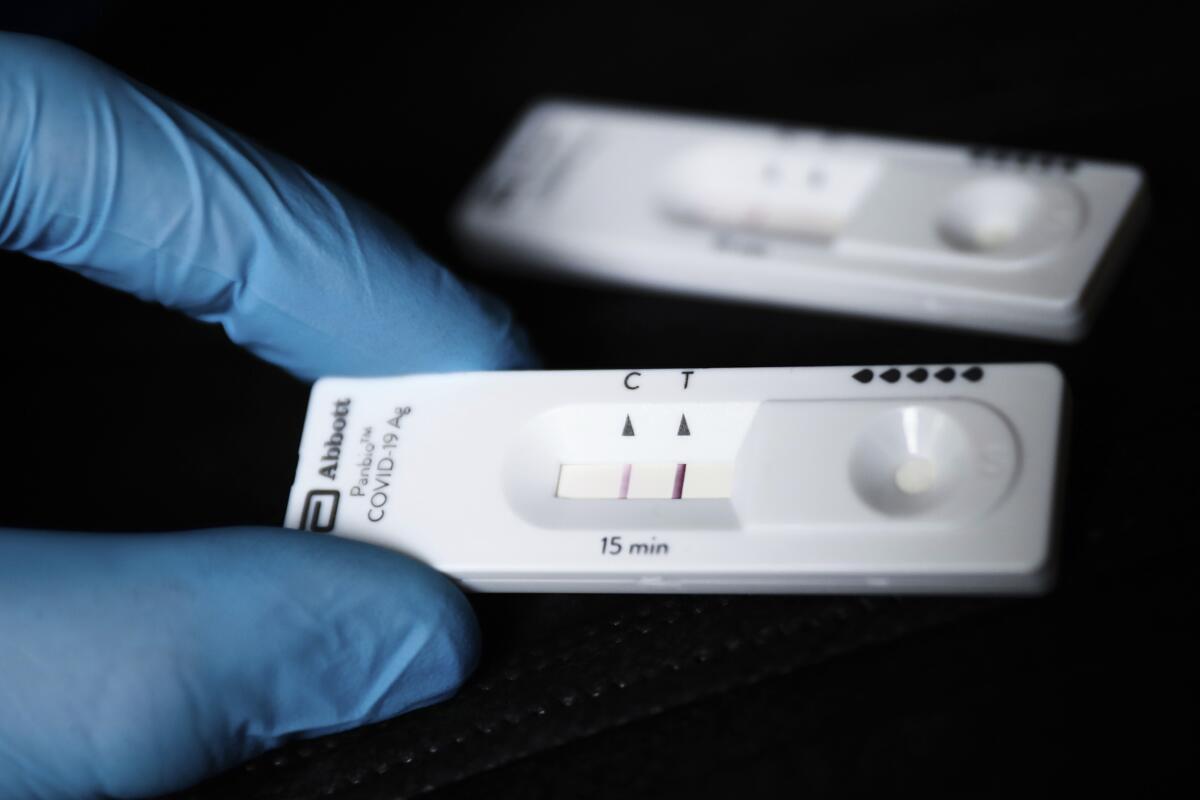
A study of 729 people who took a BinaxNow antigen test at least five days after becoming infected found that 54% of them tested positive, even though, by the CDC’s standards, enough time had passed that their isolation could end. People who had developed COVID-19 symptoms were more likely to test positive during this time, but even 21% of those who had asymptomatic infections continued to see two pink lines on their BinaxNow cards.
Overall, the odds of testing positive fell with time — 55% of people did so on Day 6, compared with 39% on Day 9.
“A positive antigen test result does not necessarily mean that a person is infectious,” wrote the authors of the study, which was published in February in the CDC’s Morbidity and Mortality Weekly Report. “Similarly, a negative test result does not necessarily mean that a person is not infectious.”
A second study attempted to evaluate whether rapid antigen tests actually determine infectiousness.
Researchers recruited 17 people who had coronavirus infections and collected specimens from them six days after they first tested positive. The specimens were taken to a lab and cultured to see if the coronavirus was still present. Six of those tests came back positive. All six of those patients also tested positive on rapid antigen tests on the same day. However, another six patients tested positive on rapid tests but got negative results on their culture tests.
In other words, if you just finished your five-day isolation period and then tested positive on a rapid antigen test, there was only a 50-50 chance that you actually harbored coronaviruses that could grow in a lab — the kind of test the researchers called “the best proxy” for determining whether a person was still infectious, according to their report last week in the journal JAMA Network Open.
(The other five people who tested negative on the rapid antigen tests had negative culture results as well.)
The 17 volunteers were among a group of 40 people who tested themselves daily once they were eligible to end their isolation. Only 10 of those 40 got a negative result on a rapid antigen test on Day 6. In fact, it took an average of eight days for those with asymptomatic infections to test negative, and nine days for those who had any COVID-19 symptoms to do so. Of the 90 tests administered to study volunteers on days when they had no COVID-19 symptoms, 68% came back positive.
The upshot, the researchers wrote, is that requiring a negative antigen test to rejoin the world would unnecessarily extend the isolation periods of many people who aren’t contagious. However, they added, if you test negative on a rapid test, you can feel reassured about ending your isolation without putting others in jeopardy.
It took President Biden a full week to test negative after he experienced a rebound infection. Dr. Kevin O’Connor, the president’s physician, said the president would continue following “strict isolation measures” until he racked up two consecutive negative tests. The second of those tests came in Sunday, clearing the way for him to resume his “public engagement and presidential travel,” O’Connor said.
By the numbers
California cases and deaths as of 5:15 p.m. on Tuesday:
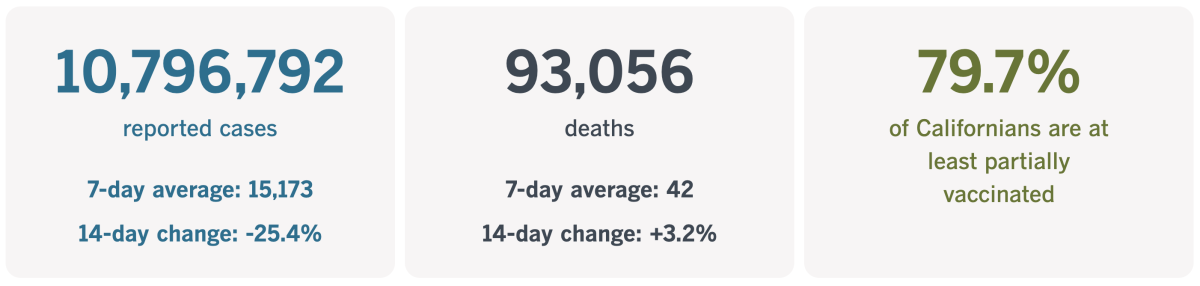
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
A different kind of pandemic isolation
Dominic Green was in graduate school at Loma Linda University near San Bernardino when the arrival of the coronavirus forced the state into lockdown. His public health courses went online, so he moved back to his parents’ home in southern Michigan and logged in from his bedroom there.
As the pandemic dragged on, several rites of passage in Green’s life were dealt with remotely. Instead of graduating in a formal ceremony, he received his master’s degree last year in a drive-through event. When he interviewed for jobs, he used videoconferencing software to impress his prospective employers. And after he landed a job as a contract epidemiologist with the Los Angeles County Department of Public Health, he moved into his own one-bedroom apartment in Koreatown and set up a remote workstation there.
He never met his new work colleagues in person, but some of them came to know one another virtually. Not only was he a terrific epidemiologist with a strong work ethic but also cooperative and kind, they said.
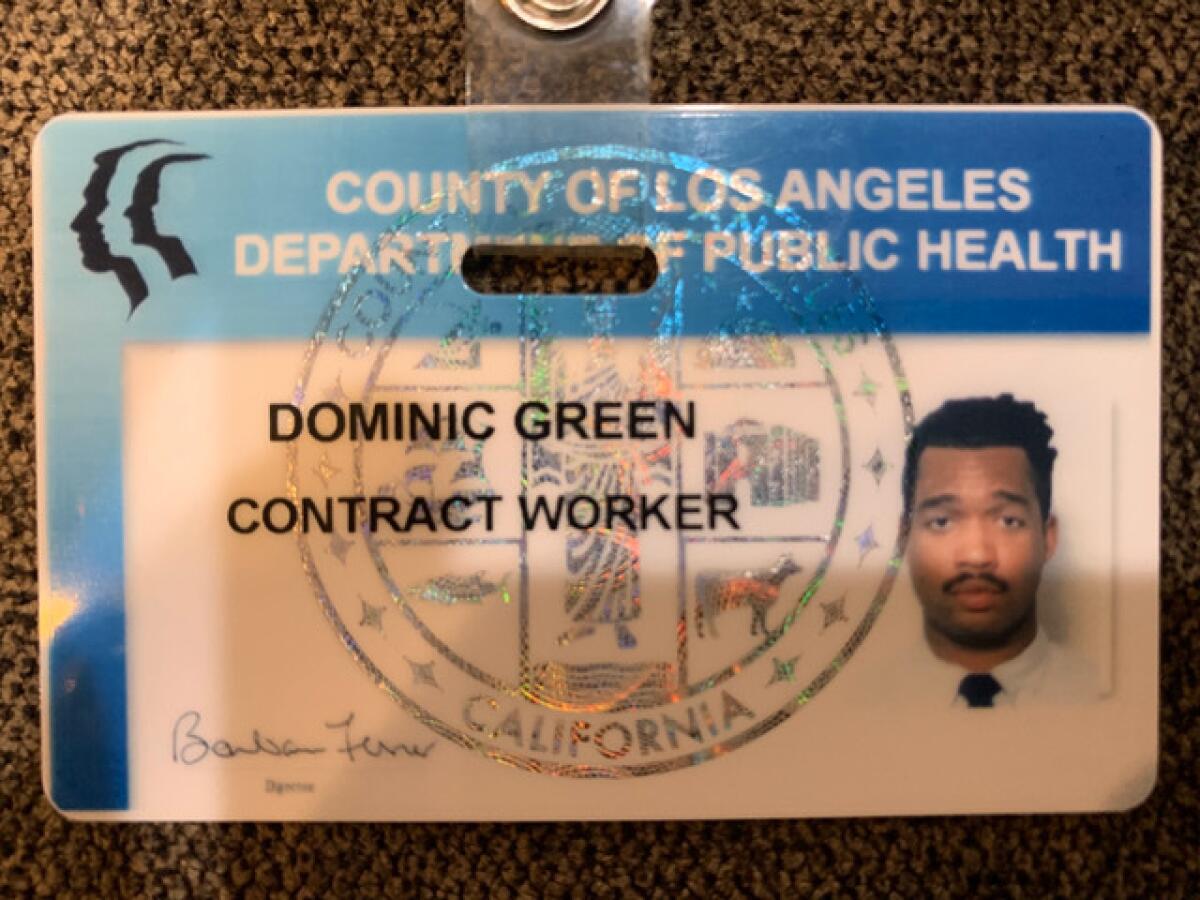
About 4 in 10 white-collar workers are still doing their jobs from home. They’re less likely to be exposed to the coronavirus this way, but they’re also less likely to bond with other people.
That was particularly true in Green’s case. He was a natural introvert and knew only a few people in L.A. when he moved here. Because of the pandemic, he wasn’t going to the kinds of places where he’d normally make new friends. In fact, he hardly left his apartment unless it was to pick up dinner. (In those cases, a long drive was a welcome respite.)
So when he didn’t report for work on Jan. 13, there was no one in his circle who was concerned enough to check in on him. And when he skipped his online check-in on Jan. 14, the result was the same.
It was only after the entire Martin Luther King Jr. holiday weekend passed without Green sending a single text that his parents realized something was amiss, my colleague Kiera Feldman reports.
Green’s father, Joseph, a recently retired lieutenant colonel in the Air Force, checked the records for the family’s cellular plan and saw that his son hadn’t made or received a call for five days. Green’s mother, Jeannine, a former registered nurse, likewise saw no activity on their joint bank account.
Joseph saw that someone with a Los Angeles phone number had sent his son two text messages. He called the texter and found himself talking to Lisa Smith, a supervisor at the county health department. Smith told the elder Green that she hadn’t heard from his son since Wednesday, and she was concerned.
Joseph and Jeannine wondered why they weren’t notified when their punctual son missed two days of work with no warning. They were listed as his emergency contacts, and when his bosses were looking for him, they could have helped.
Green’s parents were also dismayed that his supervisors didn’t go to his apartment.
“Why didn’t you check on him?” Joseph asked one of them. The supervisor responded that he was in charge of 100 people, and he didn’t want Green to get in any trouble by drawing attention to his unexplained absence.
His intentions might have been good, but Joseph and Jeannine told Feldman that more should have been done. In their view, employers have a moral responsibility to check on workers who suddenly and inexplicably go missing.
Green’s parents asked the police to conduct a wellness check on their son on the night of Martin Luther King Jr. Day. They also asked a family friend in the Los Angeles area to meet the officers at their son’s apartment.
When the friend arrived, he peered into a window and saw Green’s lifeless body lying on his bed.
Joseph and Jeannine flew to L.A. but couldn’t get many answers. They found a leftover Chipotle burrito in the fridge and a freshly unboxed video game controller near his Xbox. They were comforted to see that their son had spent his final hours with some of his favorite things.
They waited four months to get the autopsy results. In all likelihood, Green went to bed that Wednesday night and never woke up. The cause of death was cardiomyopathy, a heart condition that can cause sudden death even in people who seem healthy.

The pandemic wasn’t directly responsible, but it does explain why it took five days for anyone to realize Green had died. By then, his body was unrecognizable; officials had to use his few remaining fingerprints to verify his identity.
“How many people out there may be single and don’t have somebody else at home to see that they’re OK?” Joseph asked.
California’s vaccination progress
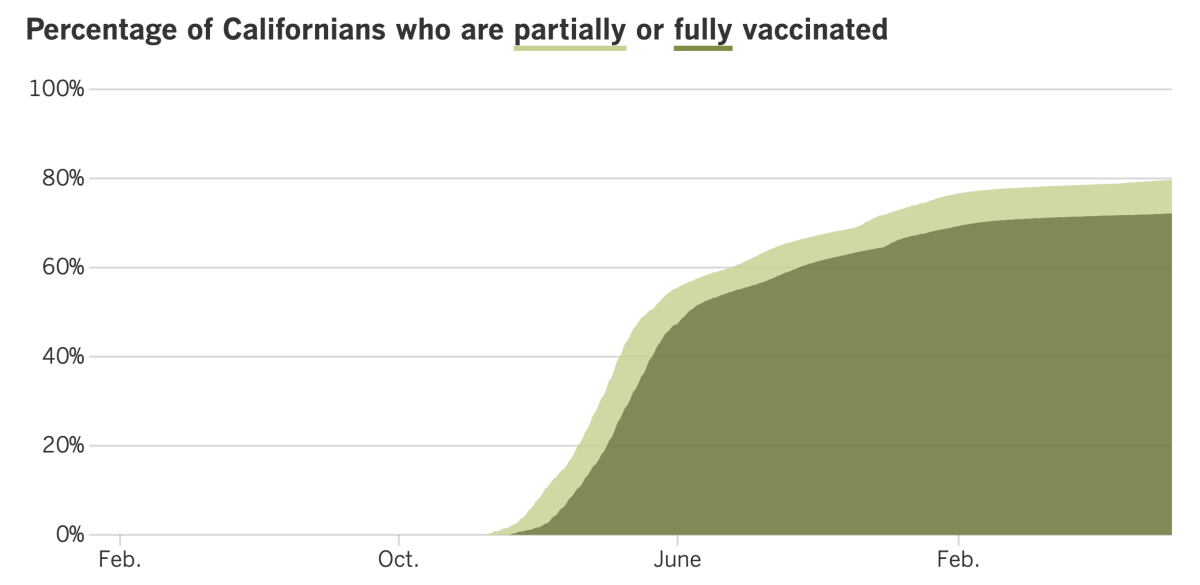
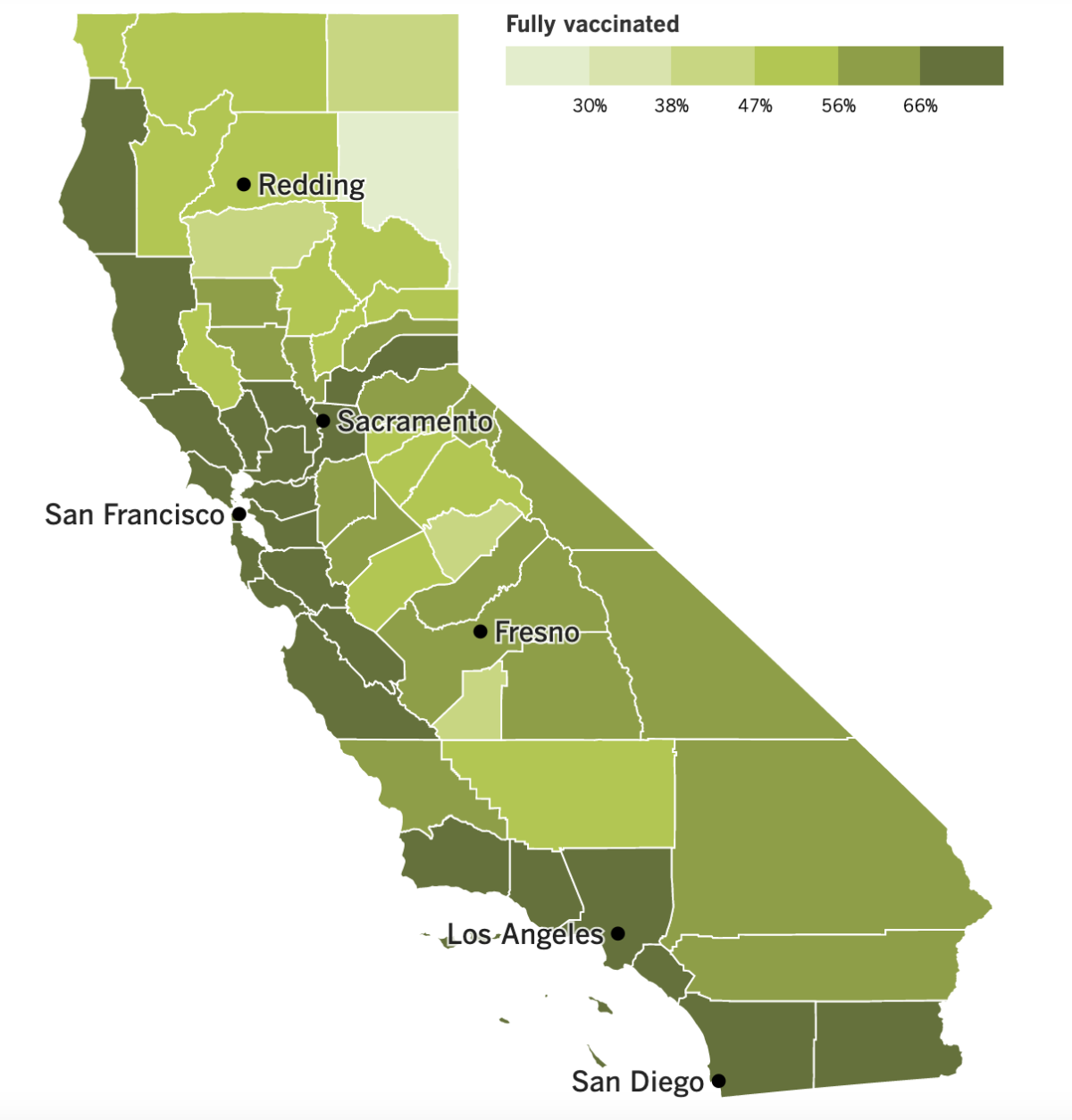
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Students throughout Los Angeles will return to classrooms on Monday, and their upcoming school year will feature much fewer swabs poked into their nostrils.
Under new Supt. Alberto Carvalho, L.A. Unified will continue to defer its COVID-19 vaccination mandate and allow mask use to remain voluntary. But what kids will notice most is the end of the weekly coronavirus testing program that screened for infections among the district’s 400,000-plus students. Baseline testing won’t be required before kids step into their classrooms either.
Instead, the nation’s second-largest school district will shift to a “response testing” program. That means tests will be required only for students who are sick and for their close contacts. Tests will also be deployed when they’re needed to help squelch an outbreak, officials said.
If a student — or teacher or staff member — does test positive, they will need to isolate for at least five days. But quarantines are no longer required for close contacts as long as they are healthy and test negative for an infection.
Most of the 80 school systems in Los Angeles County are following a similar course, according to Public Health Director Barbara Ferrer. But a few are mulling over a more aggressive approach to testing. Culver City Unified, for instance, will give students rapid tests to take at home before school starts next Thursday. Weekly testing on campus will begin during Week 2.
Some LAUSD parents would like to see their district test more aggressively too. More than 6,000 of them have sent letters to the district demanding “a better COVID plan to protect in-person learning” — one that also includes improved air quality through updated HVAC systems, high-grade HEPA filters and low-cost DIY filters, among other things.
Parents aren’t entirely at the mercy of their school system. State health officials reminded them that if they want to maximize their kids’ protection, they can make sure they’re up to date on their COVID-19 vaccinations.
“Not only do vaccinations provide individual-level protection, but high vaccination coverage reduces the burden of disease in schools and communities and may help protect individuals who are not vaccinated or those who may not develop a strong immune response from vaccination,” the state Department of Public Health wrote in its latest guidance for schools.
According to The Times’ vaccination tracker, 67% of California adolescents ages 12 to 17 are fully vaccinated. But among those ages 5 to 11, just 36% have had their initial COVID-19 shots.
“I’m predicting that after the kids come back to school ... we probably will have another wave in early fall,” Dr. Clayton Chau, director of the Orange County Health Care Agency, said last week. In O.C., 34% of 5- to 11-year-olds and 66% of 12- to 17-year-olds are fully vaccinated, according to our tracker.
Serious cases of COVID-19 are far less common in children than adults, but they can happen. On Friday, L.A. County announced that an adolescent patient had died of the disease, the 12th pediatric death in the county.
In other news, the final version of an independent report on L.A.’s emergency response to COVID-19 concluded that the lack of formal discussions about who was in charge of emergency operations led to a breakdown in coordination and communication among city departments. On the other hand, it praised Mayor Eric Garcetti for acting “quickly and decisively on many fronts, often with innovative initiatives to help protect the city and its people.”
The 220-page report by CPARS Consulting Inc. also softened or removed several criticisms of the mayor that were present in an earlier draft. For instance, gone is a reference to how several department leaders said Garcetti’s weekly “cabinet” meetings “often felt more like dictations rather than discussions.” Also excised were complaints from staffers at the Emergency Management Department that their work tasks were “politically driven.”
But the report did note that the EMD said Garcetti was less involved in emergency preparedness than his predecessors had been. The mayor’s office disputed this view.
At the federal level, the U.S. immigration system has nearly ground to a halt as it struggles to deal with the immense backlog stemming from pandemic closures. Millions of visas, work permits, green cards, naturalization petitions and cases in immigration courts are facing unprecedented delays.
Nearly 410,000 immigrant visa applicants have finished all their paperwork and are just waiting for an interview, according to figures from the State Department. In 2019, before the pandemic, the typical figure was 61,000.
The human cost of those delays can be profound. One analysis by the Cato Institute estimates that 1.6 million people who have been sponsored for a green card will die before they are able to enter the country legally.
Experts say it will be impossible for the government to catch up unless significant reforms are made. That doesn’t seem likely — it’s been more than 30 years since Congress approved a major overhaul of the U.S. immigration system.
Your questions answered
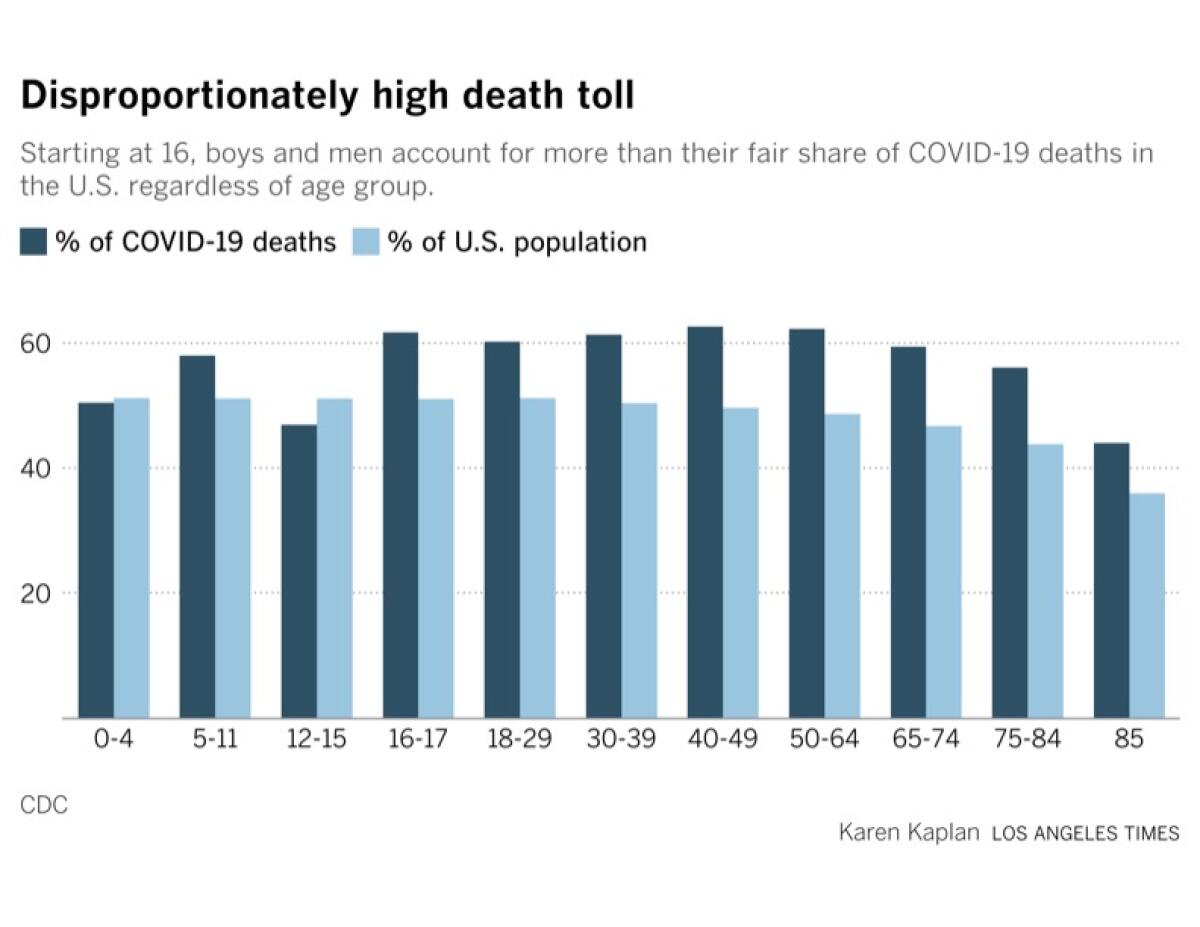
Today’s question comes from readers who want to know: Does COVID-19 still affect men more than women?
The answer depends on what you mean by “affect.”
According to the CDC, boys and men account for 46.5% of official coronavirus cases to date. That’s a little low considering that they make up 49.25% of the U.S. population. (Girls and women have experienced 53.5% of recorded cases, a figure that’s higher than their 50.75% share of the population.) However, among Americans 65 and older, men account for a little more than their fair share of cases.
The gender disparity is more pronounced when it comes to COVID-19 deaths — and that one doesn’t work in men’s favor.
Overall, 55.1% of the nation’s COVID-19 victims have been boys and men, the CDC says. That’s not only well above their share of the population, it’s significantly higher than the percentage of COVID-19 deaths involving women and girls (44.9%).
What’s more, it doesn’t take until age 65 for men to be affected more than women. COVID-19 deaths are disproportionately high for men starting at ages and 16 and 17 and remain that way right up through the 85+ cohort, as you can see in the chart below.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The deck in the photo above is attached to a villa on the outskirts of Tivat, a coastal town in Montenegro. The villa was rented by Richard Ayvazyan and Marietta Terabelian, a couple from the San Fernando Valley who took drastic steps to evade the law enforcement officers trying to send them to prison.
Ayvazyan and Terabelian were convicted last year of various crimes for their role in a family fraud ring that pocketed $18 million worth of pandemic relief loans for fake businesses. Rather than go to prison, the couple used forged Mexican passports to escape to the Balkans with their family pet. Their three teenage children were left behind in Tarzana.
“While I am writing this our tears are dripping on our breakfast table,” Ayvazyan wrote in a goodbye note. “Without saying too much, we both love you more than anything in this world.”
Did the couple’s daring escape succeed? Find out in this thrilling story by my colleague Michael Finnegan.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




