Experimental COVID-19 vaccine could outsmart future coronavirus variants
- Share via
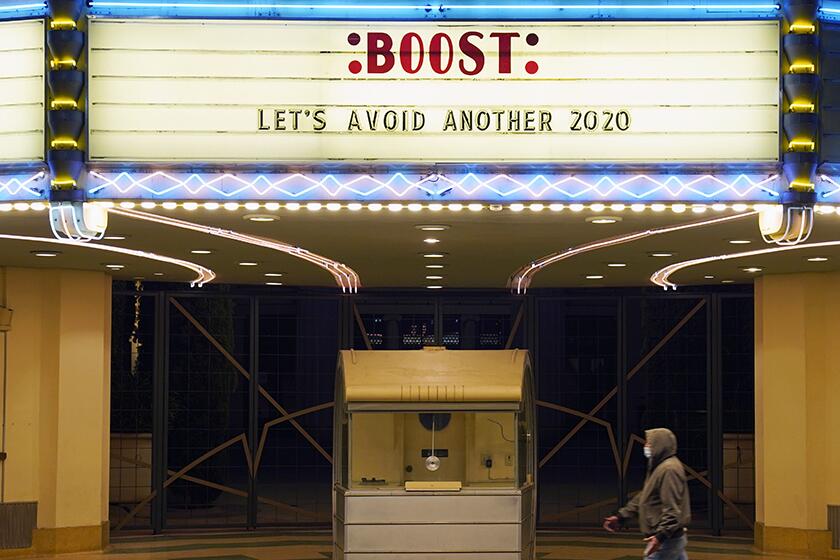
The new COVID-19 booster shots going into arms across the country are prized for their ability to recognize the distinctive spike protein shared by BA.4 and BA.5, the Omicron strains that currently account for nearly 90% of coronavirus specimens now circulating in the U.S.
But sooner or later, mutations in the spike protein will allow the virus to slip past the antibodies that are trained to recognize its predecessors. The boosters may still protect people from becoming seriously ill, but they’ll become less effective at preventing infections in the first place.
An experimental vaccine aims to solve that problem by priming the immune system to recognize both the spike protein and a second — and far more stable — viral protein.
When tested in small animals, this bivalent vaccine provided stronger protection than alternatives that targeted only one of the proteins. And, although the vaccine’s design was based on an early coronavirus strain from Wuhan, China, it remained effective against the Delta and Omicron variants.
The new shot will need to be tested in larger animals before it’s tried in people, and there’s no guarantee the results will be the same. Still, scientists said the approach could lead to a one-size-fits-all vaccine that provides more lasting protection against a virus with a proven record of spinning off new variants.
“We think of it as a one-time solution for all the COVID variants,” said Haitao Hu, an immunologist at the University of Texas Medical Branch and senior author of a study describing the vaccine in Wednesday’s edition of the journal Science Translational Medicine.
Other scientists who weren’t involved in the study agreed that if the vaccine works as well in humans as it did in mice and hamsters, it could help us stay a step ahead of the coronavirus.
“It’s a great idea,” said Dr. Paul Offit, a virologist and immunologist at the University of Pennsylvania who wasn’t involved in the study. “You could have argued that we should have done this at the beginning.”
Determining which version of the coronavirus should be used to make COVID-19 vaccines and boosters is an exercise in educated guesswork.
The current COVID-19 vaccines have saved an estimated 19.8 million lives around the world. Yet as the virus has evolved, their effectiveness in preventing infections has lessened, meaning more illness, more time away from work and school, and more people at risk of developing long COVID.
The situation has forced scientists to play catch-up with the variants, Hu said: “You’re always one stage behind.”
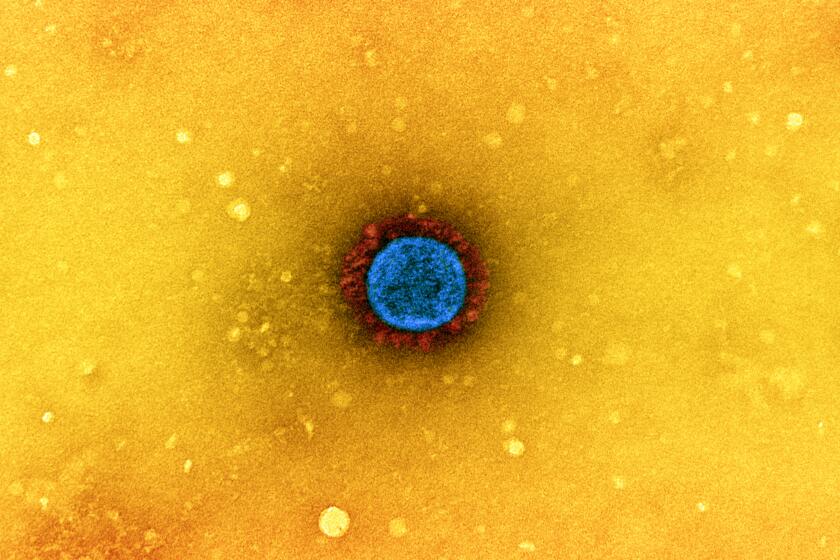
The spike protein on the SARS-CoV-2 virus is in some ways the pandemic’s double-edged sword. It’s the key target of all four COVID-19 vaccines currently available in the U.S. But it’s also the part of the virus most likely to take advantage of random mutations that allow it to dodge the immunity those vaccines are intended to provide.
There’s a reason why the spike protein, or “S” in virology shorthand, is so susceptible to evolutionary pressure: It’s the part of the virus that initiates an infection by entering a host cell. If the spike can’t do its job, the virus can’t survive.
Researchers at Caltech have developed a vaccine designed to neutralize multiple coronaviruses at the same time.
The second target of the experimental vaccine is the nucleocapsid protein, known as “N.” It’s situated in the virus’ core and has little reason to change. But once inside a host cell, it plays an essential role in allowing the coronavirus to make copies of itself.
Hu and his colleagues used the same mRNA technology as the Pfizer-BioNTech and Moderna vaccines to encode instructions for making harmless copies of both the S and N proteins. Once those copies are made, the immune system recognizes them as threats and learns to respond accordingly.
The researchers began their tests by injecting small groups of mice with vaccines that targeted only the N protein. The animals mounted an immune response, but only a modest one, Hu said.
Exposing cells to N did not trigger the production of neutralizing antibodies. The study authors expected this, as N isn’t involved in helping the virus barge its way into a host cell. The exposure did, however, induce a strong T-cell response, which helps clear the virus from the cell.
When the coronavirus attacks the body, the immune system steps up, trying to respond quickly and powerfully enough to stop the virus from running wild.
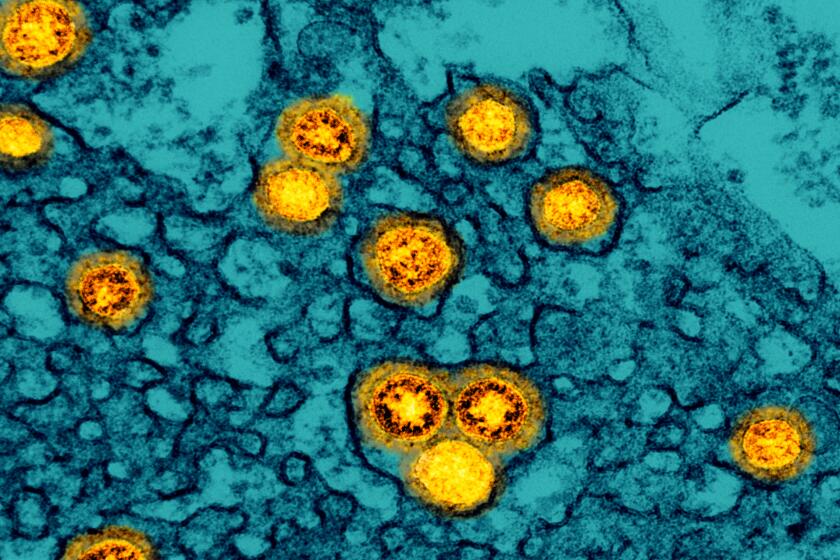
Next, the researchers injected animals with a bivalent vaccine that targeted S and N at the same time. The immune response was much stronger: No viral RNA was detected in the lungs of the eight mice that received the bivalent vaccine. By contrast, among eight mice immunized with a shot that targeted only S, seven had detectable amounts of viral RNA.
Additional tests were conducted in hamsters that were exposed to the Delta variant. The results were similar: The viral load was undetectable in animals that received the combination vaccine, and their lung pathology was clear. Compared with hamsters that got the S-only vaccine, they also had less virus in their upper respiratory tracts, which could make them less likely to spread the virus to others.
Hamsters exposed to the Omicron variant fared better with the bivalent vaccine as well. Four of five hamsters who received it had no detectable virus, compared with just one of five hamsters that were vaccinated with a shot that targeted only S. The animals that got the bivalent vaccine had no lung damage, while those that got the S-only vaccine developed lesions on their lungs. The bivalent vaccine also reduced viral loads in the hamsters’ upper respiratory tracts.
Conventional wisdom says Omicron is less likely to cause serious illness, but that might be due to better immunity and treatments, not the virus itself.
The Texas team isn’t the first to go after the spike and nucleocapsid proteins at the same time. ImmunityBio of Culver City has developed a COVID-19 vaccine with a similar structure that’s currently in clinical trials in South Africa.
The new study “confirmed that when you have S plus N, you’re able to have multivariant protection,” said Dr. Patrick Soon-Shiong, ImmunityBio’s executive chairman. (Soon-Shiong also owns the Los Angeles Times.)
The S protein “gives you a good antibodies, and N gives you amazing T cells,” he said. “It’s the interplay between the antibodies and the T cells — by having both, you get the best of both worlds.”
One thing the new study did not address is how long the benefits of the combination vaccine would last, said Stanley Perlman, a microbiologist and immunologist at the University of Iowa. The animals were tested two weeks after receiving their final dose, and the study authors acknowledged that longer experiments were needed to gauge the vaccine’s longevity.
Hu said his team’s next step is to study the vaccine in nonhuman primates. If all funding and approvals come through, that could be completed within six months, and if the results are good, human trials would be next, he said.