Post-Roe vs. Wade, more patients rely on prenatal testing as states toughen abortion laws

- Share via
WASHINGTON — Since Roe vs. Wade was overturned, many healthcare providers say an increasing number of patients are deciding the fate of their pregnancies on whatever information they can gather before state abortion bans kick in.
But early ultrasounds show far less about the condition of a fetus than later ones. And genetic screenings may be inaccurate.
When you find out your fetus has a serious problem, “you’re in crisis mode,” said Sabrina Fletcher, a doula, or pregnancy advisor. “You’re not thinking about legal repercussions and [state] cutoff dates, and yet we’re forced to.”
About half of states ban abortion or restrict it after a certain point in pregnancy.
This leaves millions of women in roughly 14 states with no option to get follow-up diagnostic tests in time to feasibly have an abortion there if they wanted, a paper published last March in the journal Obstetrics and Gynecology found. Even more states have abortion cutoffs too early for mid-pregnancy ultrasounds.
“More people are trying to find these things out earlier to try to fit within the confines of laws that, in my mind, don’t have a place in medical practice,” said Dr. Clayton Alfonso, an OB-GYN at Duke University in North Carolina.
When done at the right time, doctors said, prenatal testing can identify problems and help parents decide whether to have an abortion or continue a pregnancy and prepare for a baby’s complex needs after delivery.
One of the most common tests is the 20-week ultrasound. It checks on the fetal heart, brain, spine, limbs and other parts of the body, looking for signs of congenital problems. It can detect abnormalities and signs of chromosomal problems such as Down syndrome. Follow-up testing may be needed to make a diagnosis.
Earlier ultrasounds, in the first trimester for example, are not standard practice because it is too soon to see many of the fetus’ limbs and organs in detail, the American College of Obstetricians and Gynecologists says.
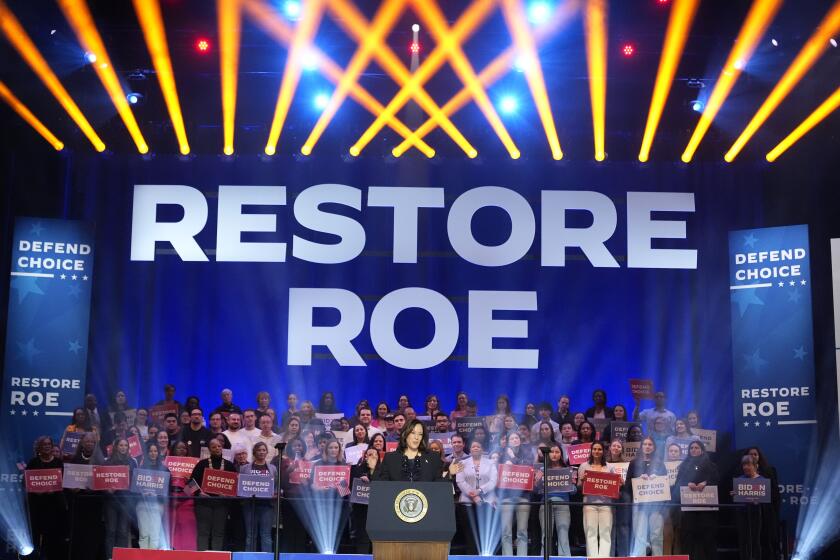
Vice President Kamala Harris traveled to California as part of her abortion rights tour for the 50th anniversary of the Roe vs. Wade ruling.
It’s impossible to spot problems like serious heart defects much before mid-pregnancy because the fetus is so small, said Dr. Cara Heuser, who practices maternal-fetal medicine in Utah. Nonetheless, she said, more patients are having ultrasounds at 10 to 13 weeks to get access to abortion if they choose.
Experts say there are no statistics on how many people opt for early ultrasounds or make choices based on them. But some healthcare providers say they’ve noticed an uptick in requests for the scans, including Missouri genetic counselor Chelsea Wagner. She counsels patients from around the nation through telehealth.
But she said doctors can’t provide patients with “an ‘everything looks good’ or a clean bill of health off of an ultrasound at 10 weeks.”
Doctors also can’t make a firm diagnosis from a genetic screening, which is done at 10 weeks gestation or later. These screenings are designed to detect abnormalities in fetal DNA by looking at small, free-floating fragments circulating in a pregnant woman’s blood.
They screen for chromosomal disorders such as trisomy 13 and 18, which often end in miscarriage or stillbirth, Down syndrome and extra or missing copies of sex chromosomes.
The accuracy of these tests varies by disorder, but none is considered diagnostic.
Natera, one of only a handful of U.S. companies that make such genetic tests, said in an email that prenatal test results are reported as either “high risk” or “low risk” and that patients should seek confirmatory testing if they get a “high risk” result.
Some may be pretty accurate, doctors said, but false positives are possible. In 2022, the Food and Drug Administration issued a warning about the screenings, reminding patients and doctors that results need further confirmation.
The agency is poised to release a new regulatory framework in April that would require prenatal screenings, and thousands of other lab tests, to undergo FDA review.
In states with tough abortion laws, healthcare providers said, there’s more urgency because of the timing of diagnostic tests.
CVS, or chorionic villus sampling, is offered at 10 to 13 weeks gestation. Initial results take a few days and more detailed ones around two weeks. Amniocentesis is typically done at 15 to 20 weeks, with similar timing for results.
If a state has a 12-week abortion ban, for instance, “some people may have to act on a screening,” Alfonso said.
Wagner said she’s had to counsel patients who couldn’t afford to travel out of state for an abortion if they had to wait for diagnostic testing. “They are forced to use the information they have to make choices they never thought they’d have to make,” she said.
Some states restrict abortion so early that women would not have the chance to get any prenatal testing done before the cutoff.
That was the case for 26-year-old Hannah in Tennessee, which has a strict abortion ban. An ultrasound in late November, at about 18 weeks, revealed she had amniotic band sequence, when very thin pieces of the amniotic membrane get attached to the fetus. In Hannah’s case, the bands were attached to many of her baby’s body parts and ripped open multiple areas of his body.
After calling clinics in Ohio and Illinois to terminate the pregnancy, she finally found one 4½ hours away in Illinois and had the procedure in early December at 19 weeks gestation. Results from the amniocentesis — which was done to look for the cause of the problem — came back the day after her abortion, and other results after that.
Hannah, who didn’t want her last name used for fear of backlash, said it’s “awful” to have to think about state timelines, and to travel long distances when dealing with something like this. But she’s grateful she had enough information to feel confident in her decision.
“I know some women are not that lucky,” Hannah said. She named her son Waylen.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.