Op-Ed: Rules for gay blood donors are based on outdated fear, not science
- Share via
In my senior year I helped organize a blood drive in my high school gymnasium. I felt newly mature as I signed the consent form; the idea that my transient discomfort potentially could help save a life inspired me, and I committed to making blood donation a habit. When I received my American Red Cross Donor Card weeks later indicating that I was “O-negative” – a universal donor – I became all the more motivated.
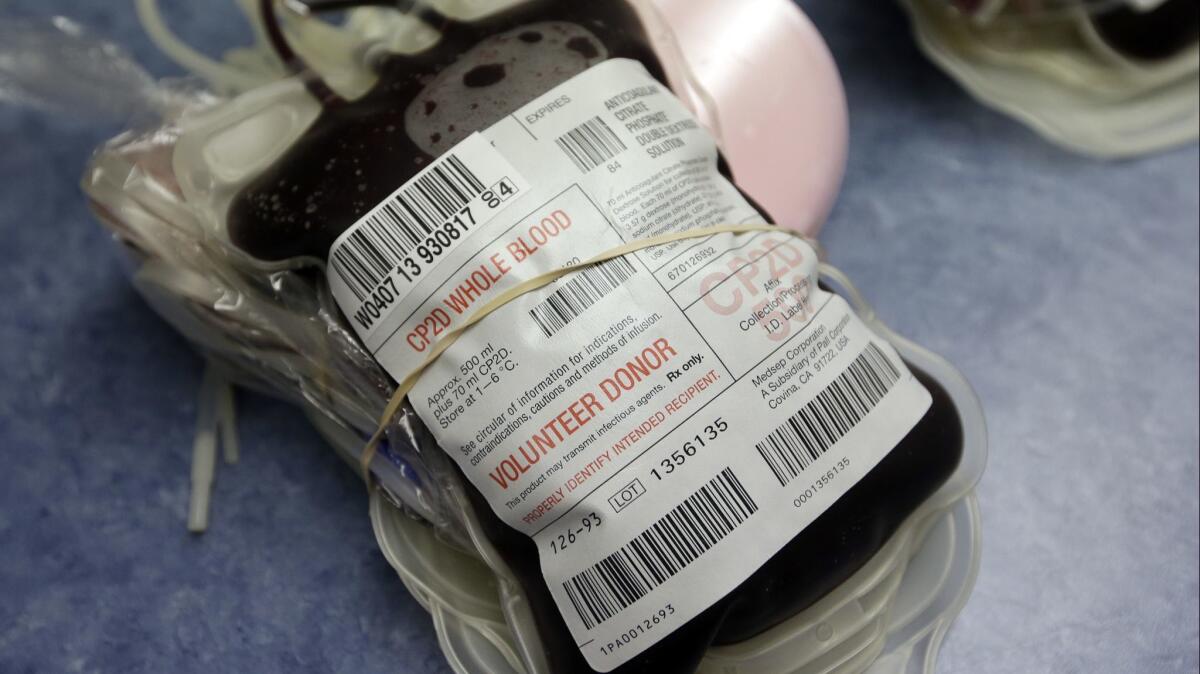
I’m now, years later, a physician who sees patients benefit from transfusions every day, from children with sickle cell disease to adults with leukemia. My husband sees blood products being put to work even more dramatically on his shifts in the emergency department, as they’re rapidly infused into trauma patients. When there’s no time for matching blood types, it’s O-negative blood like mine that is pumped into these patients’ veins.
The hospitals where I work regularly broadcast requests for donors via email. “Immediate Need for Type O-Negative Whole Blood Donors,” they implore. About 7% of the U.S. population has O-negative blood, and they can only receive blood from other O-negatives. Consequently, O-negative donors must provide enough supply to completely meet that population’s demand in addition to those whose blood types are uncertain at the time of transfusion. Critical shortages are commonplace.
But I cannot respond to these calls.
Many people, including fellow doctors, don’t realize that the Food and Drug Administration bans all gay men from giving blood products unless they have been sexually abstinent for the previous 12 months. (A previous lifetime ban on blood donations from gay men was repealed in 2015.) Unfortunately, these guidelines are derived from a legacy of fear rather than scientific fact. In the early days of the AIDS epidemic, thousands of people contracted HIV from transfusions. But back then HIV tests were less sensitive and couldn’t begin to detect the virus until 6 to 12 weeks after infection.
A straight man with an active chlamydia or herpes infection is not prohibited from donating blood.
Today’s blood screening technology detects HIV within nine to 14 days of exposure with near-perfect sensitivity. Advances in research on HIV transmission also have provided highly reliable methods for determining if someone is at risk of recent infection based on their behaviors, not sexual orientation. A patient’s chance of getting HIV from a blood transfusion in the United States today is 1 in 1.5 million.
In light of these advances, there is little reason to retain a system in which needed donors are excluded based on sexual orientation while heterosexuals with multiple concurrent partners are given the green light. Under the current system, for instance, a straight man with an active chlamydia or herpes infection is not prohibited from donating blood, even though such infections suggest recent high-risk sexual contact. In a country where nearly a fourth of new HIV diagnoses are coming from heterosexual transmission, this double standard makes no sense unless the fundamental goal is discrimination, not safety.
Not all countries do what we do. Gay men can donate blood in Argentina, Italy, Spain, Poland and even Russia, among others. Rather than screening out potential donors based on sexual orientation, countries like Italy engage in individual sexual risk assessment and evaluation (so-called “assess and test”). Using this evidence-driven approach, Italy has seen no increase in transfusion-based transmission of HIV. France, which, like us, has a one-year deferral policy for sexually active gay men, is currently being taken before the European Court of Human Rights for discrimination. If successful, the case could have implications across Europe.
I am hardly the only one pointing out that the FDA needs to update its blood donor rules. The American Medical Association has proposed that the FDA “ensure blood donation bans or deferrals are applied to donors according to their individual level of risk and are not based on sexual orientation alone.” The American Association of Blood Banks, America’s Blood Centers and the American Red Cross have all similarly advocated for science-based approaches to blood safety. Studies estimate that if the FDA policy was revised, an additional 219,200 pints of lifesaving blood could safely be donated each year.
The science is solid. The current FDA policy, on the other hand, is just discriminatory, casting a shadow on an otherwise venerable practice.
Dr. C. Nicholas Cuneo is resident physician in the Harvard combined program in internal medicine and pediatrics at Brigham and Women’s Hospital and Boston Children’s Hospital.
Enter the Fray: First takes on the news of the minute from L.A. Times Opinion »
Follow the Opinion section on Twitter @latimesopinion and Facebook
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.