Potent New Weapon : Scientists say a new class of drugs called protease inhibitors could ‘fundamentally change the landscape’ of treating AIDS. : SCIENCE FILE: An exploration of issues and trends affecting science, medicine and the environment.
- Share via
WASHINGTON — Protease inhibitors--the powerful new generation of antiviral AIDS drugs about to enter the marketplace--have been studied in the laboratory for at least seven years. But nobody knew how potent they were in humans until a little more than a year ago.
During a scientific meeting in Orlando, Fla., in the fall of 1994, AIDS researchers heard startling data about the drugs’ impact on the small number of patients who had taken them: All the subjects showed an astonishing drop in the amount of virus detectable in their blood.
In fact, during the patients’ first few weeks on the drugs, the decline of virus in their blood plasma was 100-fold. Moreover, the drop was 10 times greater than what had been seen using the most commonly prescribed AIDS drugs, AZT, DDI and DDC.
The news couldn’t have come at a better time.
After years of frustration and gloom at the plodding pace of therapeutic advances, “we realized that this potent new class of drugs could fundamentally change the landscape of treating this disease,” said Dr. Robert T. Schooley, head of infectious diseases at the University of Colorado Health Sciences Center.
“Now we have a much better feeling for the direction we need to be going,” added Schooley, who chairs the executive committee of the federal government’s AIDS Clinical Trials Group.
In recent years, most researchers have come to believe that the best approach to attacking the underlying viral condition is to use a combination of drugs, each one designed to hit the virus at a different stage of its life cycle, with the ultimate hope of suppressing the virus in a way that will prolong life indefinitely.
Most AIDS specialists agree that such an outcome is not yet on the horizon. However, the U.S. Food and Drug Administration’s approval last week of the first protease inhibitor (Invirase, or saquinavir, made by Hoffmann-La Roche Inc. of Nutley, N.J.) has moved that scenario much closer.
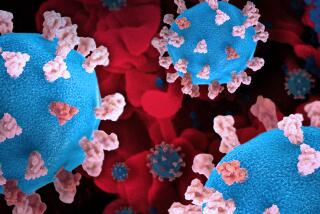
To appreciate the strategy involved, it is important to understand the nature of the virus itself.
The human immunodeficiency virus is a retrovirus, meaning that unlike most viruses, its genetic material is made of RNA, rather than DNA. DNA, deoxyribonucleic acid, is the master genetic blueprint of the cell stored in the nucleus. RNA, ribonucleic acid, normally serves as the working blueprint of the cell, transferring genetic information from the nucleus to the cytoplasm, where cellular components are synthesized.
*
To infect a human cell--and use its machinery to replicate--HIV must convert its RNA into DNA. To do so, it uses an enzyme called reverse transcriptase early in its replication process.
Since the late 1980s, clinicians have relied on a family of drugs known as nucleoside analogues--AZT, DDI, DDC, D4T and the recently approved 3TC--to attack the virus at this early phase and inhibit the work of reverse transcriptase.
But the benefits have proved temporary.
Like many microorganisms, HIV eventually outsmarts the drugs, forming mutations that escape their effects. These new strains continue to infect CD4 immune system cells and reproduce. In other words, the virus develops a resistance to the drugs, rendering them ineffective.
Protease inhibitors, on the other hand, hit the virus at a later stage, after it has begun reproducing within the infected cells.
This is how the inhibitors work:
To finish making copies of itself, the virus must produce two large proteins, known as pro-proteins, in the form of two long strands. The strands include all the elements needed to build pieces of new infectious virus. But to do so, each strand must be broken into smaller sections, each with its own function. If they stay attached, none of these components can work.
Protease, an enzyme made by the virus, does the cutting. It chops the proteins into the right-size pieces to complete replication.
A protease inhibitor “tricks” the enzyme, blocking it from doing its cutting.
The drug “acts like the part of the protein that’s supposed to get cut,” said Dr. Miklos P. Salgo, Roche’s director of clinical virology. “The protease inhibitor fits into the protease enzyme, on top of the pro-protein, so the enzyme is locked up and can’t go to the pro-protein” to do the cutting job.
*
Because the two proteins do not get chopped up into their active sections, “they can’t form the different parts of the virus that they’re supposed to in order to finish the replication,” he said.
The result produces new virus--but new virus that is not infectious and essentially harmless.
This could mean that many fewer CD4 cells become infected (and subsequently destroyed) and that the immune system remains intact longer--perhaps indefinitely.
The problem with protease inhibitors, as with almost all drugs, is resistance.
When taken alone--that is, not in combination with other drugs--resistance to protease inhibitors does, in fact, develop.
Scientists hope, however, that using a protease inhibitor in combination with another type of drug can blunt HIV’s ability to thwart these and other drugs.
“Mutants [resistant strains] will develop to the drug, but the idea of combination therapy is that whatever mutant develops to one drug will be killed by the other drugs,” said Dr. Anthony S. Fauci, director of the federal government’s National Institute of Allergy and Infectious Diseases.
Salgo cautioned that “we have not yet found the combination that will last forever.” But “we’re hoping as we get more powerful combinations and learn to use them more appropriately--which probably means when patients are healthier--we may be able to suppress the virus,” he said. “And with less virus in the body, you’re less likely to have a mutation that results in resistance.”
The other good news about protease inhibitors is that they are far less toxic than nucleoside analogues.
The chemical structure of the analogues is similar to the body’s own genetic building blocks; thus there is some crossover of the drugs into the DNA of other cells, which can cause potentially serious side effects. Side effects from the various nucleoside analogues have included low red blood cell count, neuropathy (pain and tingling in extremities) and inflammation of the pancreas.
But the protease enzyme “is a very unique enzyme seen only in the virus,” Salgo said. “So the inhibitors won’t go after anything else.”
There are at least six protease inhibitors in various stages of development, and researchers predict that even stronger forms of these drugs soon will show up soon in the pipeline.
Their experience in humans remains limited, however, and it is still unclear how beneficial they will be.
Nevertheless, “if one extrapolates from clinical trials that have been done, we can expect these drugs to have a very important impact on the disease,” Schooley said.
(BEGIN TEXT OF INFOBOX / INFOGRAPHIC)
How Protease Inhibitors Work
Although both the new protease inhibitors and existing AIDS drugs, such as AZT and DDC, interfere with the replication of the AIDS virus, their activities are complimentary because they target different stages of the viral life cycle. AZT and similar drugs interfere with the replication of viral RNA, preventing the introduction of the virus’ genetic blueprint into the cell. Protease inhibitors prevent the production of new viruses even after viral genes have taken over the cell’s metabolic machinery.
1. In making new virus particles, the cellular machinery does not produce each viral protein separately. Instead, it manufactures two large molecule, called pro-proteins, which contain all of the viral proteins linked together, somewhat like beads on a chain.
2. An enzyme called protease then cuts extraneous material out of the pro-proteins, thereby freezing the viral proteins for inclusion in the viral particles. Protease inhibitors bind tightly to this enzyme, preventing it from cutting up the pro-proteins.
3. As a result, the virus articles produced contain nonfunctioning pro-protein rather than the individual proteins necessary to infect other cells. Although they look like viruses, these altered particles are essentially harmless.