The COVID ‘emergency’ is ending. Here’s who will be hurt most

- Share via
In the State of the Union, President Biden stated that “we have broken COVID’s grip on us.” Indeed, COVID-19 deaths are down about 75% since last year’s speech. Consistent with that progress, the Biden administration announced in January that it will end the public health emergency (and national emergency) declarations on May 11.
Yet nearly 500 Americans are dying from COVID-19 per day. As many as 1 in 5 U.S. adults who contract the virus experience some effects of long COVID. And the toll of the disease has never been distributed equally.
Historians have long pointed out that pandemics tend to reveal social inequalities and often make them worse, as we have seen with COVID. Studies show that people in areas of social disadvantage have died from COVID at higher rates than those in affluent areas. After controlling for differences in age, people of color have contracted COVID at higher rates, and have died at higher rates, than white people.
It was these inequities that prompted the Biden administration, Congress and some states to adopt policies designed to even the playing field. These policies meant that most Americans could access COVID testing, treatment and vaccines for free or close to free. They also addressed access issues — getting people insured — by expanding Affordable Care Act subsidies for exchange policies, offering a temporary Medicaid coverage option for uninsured people in 15 states, and by not disenrolling anyone from Medicaid in all states during the public health emergency. Between February 2020 and March 2021, at least 13 million additional people enrolled (and stayed) in Medicaid. These policy changes didn’t solve health inequity, but they blunted the impact of COVID on vulnerable communities.
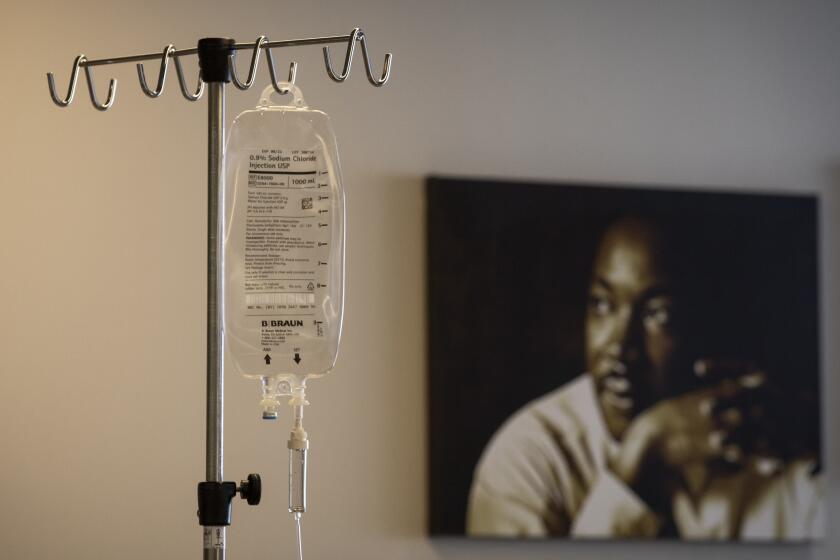
But with the end of the public health emergency, so too comes the end of many of these protections. Most uninsured people will no longer be able to access free COVID tests. Medicaid continuous coverage is ending. The federal uninsured fund has already lapsed.
The COVID-19 pandemic made our shortage of healthcare providers worse. There are solutions we can act on now.
A direct consequence will be that the uninsured and undocumented people, almost half of whom are uninsured, won’t be able to access care for COVID. This is a tragedy in its own right and is likely to expand racial health inequalities connected to COVID. It will also have broader impacts on the community and the economy as COVID will spread, workforce shortages will continue and burdens of long COVID will increase.
Perhaps the most consequential change ahead is the looming loss of Medicaid eligibility for millions of low-income Americans. As part of a spending bill signed into law in December, states will soon begin a redetermination process for deciding Medicaid eligibility. Disenrollments can begin as soon as April. As many as 18 million enrollees may lose coverage. The U.S. Department of Health and Human Services predicts that people of color are much more likely to lose coverage based on administrative hurdles alone, even if they remain eligible for Medicaid.
This massive coverage loss in a short period of time could have devastating consequences, further straining already-stretched hospitals, diminishing access to necessary screenings and care for chronic disease, as well as increasing emergency department use and medical debt for low-income Americans. Black and Hispanic people are twice as likely as white people to be enrolled in Medicaid and more likely to be directly impacted.
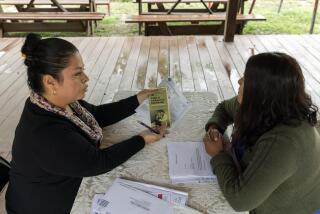
There are actions states should take now to prevent worsening COVID inequities. State governments can start by encouraging those who lose Medicaid coverage to get alternative coverage that will provide COVID benefits. Many will be eligible for free or reduced cost plans in the Affordable Care Act marketplace. Rhode Island is launching a program to automatically enroll those who lose Medicaid coverage during unwinding into a marketplace plan. Other states, like Maryland, plan to use navigators to contact those no longer eligible for Medicaid to help them enroll in a qualified health plan.
Too few doctors can afford to practice in the communities that rely on Medi-Cal, which are largely made up of people of color.
States could also look at other ways to ensure access to social safety net programs for low-income communities. For instance, in November, Colorado opened enrollment for a program called OmniSalud that assists undocumented residents and individuals with protections through the Deferred Action for Childhood Arrivals program to obtain affordable healthcare insurance through the state’s marketplace. By January, 10,000 Colorado residents had enrolled.
In many states, however, undocumented immigrants and some people who cannot afford a policy have limited options to obtain coverage, particularly in the 11 states that have not expanded Medicaid. As such, states and localities must also continue to look for ways to provide free COVID testing and treatment to uninsured populations.
Finally, good public health requires more than access to healthcare. States can work to enact social policies that are likely to reduce COVID-related inequalities, such as paid sick leave laws, universal basic income requirements and supplemental nutrition assistance programs.
The Biden administration’s decision to end the public health emergency is in some sense understandable. States of emergency cannot persist indefinitely. Even the World Health Organization recently signaled that it may be preparing to end its declaration of the COVID pandemic as a “public health emergency of international concern.” But moving out of the declared emergency doesn’t mean we should forget that the burden of COVID is borne disproportionately by vulnerable communities. Policies to prevent worsening COVID-driven inequities can — and should — be enacted now.
Wendy Netter Epstein is a professor of law and associate dean of research at DePaul University College of Law. @ProfWEpstein. Daniel Goldberg is an associate professor in the Center for Bioethics and Humanities at the University of Colorado Anschutz Medical Campus. @prof_goldberg
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.