Don’t curb opioid prescriptions through telemedicine. They’re saving lives

- Share via
The explosion of telemedicine during the COVID-19 pandemic has been transformative for countless patients who might otherwise be unable to access care. But the Drug Enforcement Administration is preparing to roll back telemedicine options for many essential prescriptions. It would be a dangerous move, exacerbating already gaping disparities and imperiling the most vulnerable patients.
The proposed rule changes would require that patients be seen in person in order to receive prescriptions for certain controlled medications, including stimulants and opioids to treat attention disorders, pain and seizures. For other controlled medications, such as buprenorphine, which is used to treat opioid use disorder, the DEA would allow a 30-day supply to be provided via telemedicine, but a patient must then arrange an in-person visit to continue to receive medication.
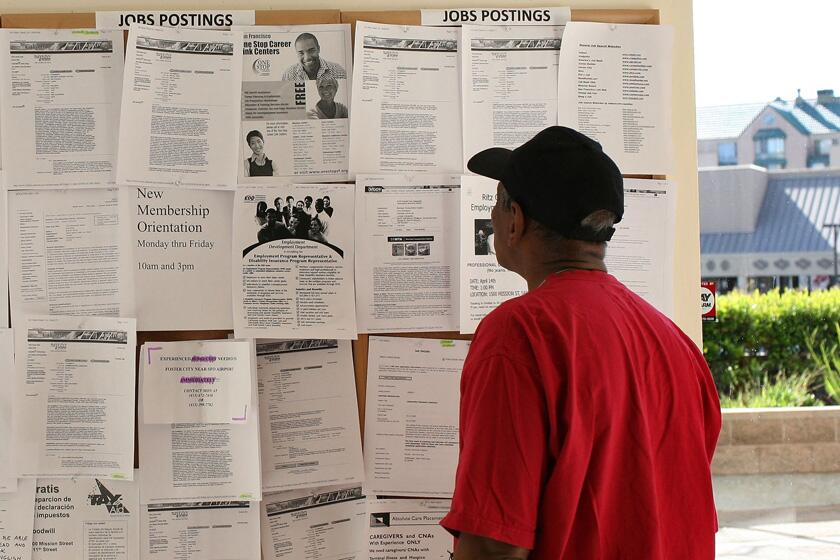
One key problem with these proposals is that they ignore the fractured reality of our healthcare system, where care deserts are rampant. Currently, nearly 100 million Americans live in areas with a shortage of health professionals, while 130 million face a dearth of behavioral care providers. In the cities with the best physician-to-patient ratios, the average wait time to arrange primary care is 26 days. In rural areas where many clinics and hospitals have shuttered, wait times are considerably longer.
Care deserts aren’t just geographic. Policies and law enforcement create barriers to access that burden some people more than others. An overzealous 2016 guideline from the Centers for Disease Control and Prevention, for example, created barriers to care for the 8 million Americans who use opioids to manage pain, as the agency has acknowledged. Half of primary care clinics will simply refuse to treat these patients.
Barriers to prescription access are deadly. Medication disruptions for patients on opioids triple the risk of overdose and suicide.
Federal policies have created barriers to addiction treatment as well, although recently ending the waiver that allowed buprenorphine to be prescribed as an outpatient treatment for opioid addiction will help. Still, as a result of such obstacles, fewer than 22% of the 2.1 million Americans with an opioid use disorder receive medication like buprenorphine that cuts their risk of death in half or more. Those who go off buprenorphine or complete only a four-week course tend to return to opioid misuse.
Drug-related mortality surpassed 107,000 last year driven by illicitly manufactured fentanyl. Interrupting treatment is counterproductive at an especially dangerous moment to incentivize people to turn to a tainted street market.
The proposed changes to current regulations are a “solution” in search of a problem. More than three years into the pandemic, we know that telemedicine has worked. Creating barriers to continued access to care is unconscionable. They will be compounded for people of color, women and people with disabilities.
Black and Latino patients already receive less pain medication, even cancer patients at the end of life. Women more often have pain dismissed, though studies show they experience more severe pain. So do transgender people who face heightened barriers to care. Black, American Indian and Alaska Native individuals also have the highest rates of overdose and the most limited access to lifesaving medications for opioid use disorder.
People with disabilities have poorer health outcomes and face obstacles to care such as transportation barriers. Some who are more susceptible to COVID-19 will soon have to decide whether to forgo medications or risk their safety by visiting a healthcare setting in person.
For these patients, telehealth extends a lifeline. And in rural areas, it offers vital access to needed care. For individuals with disabilities, the group most likely to have used telemedicine in 2022, it bridges access barriers. For those vulnerable to overdose, studies show that telemedicine prescribing during the COVID-19 public health emergency significantly increased access, improved retention in care, and reduced overdose and drug-related mortality.
The government has an interest in preventing drug diversion, but it should follow the evidence. Provisional data from the National Center on Health Statistics show no rise in prescription-related drug overdose deaths during the COVID emergency while telemedicine prescribing was the norm; on the contrary, telemedicine prescribing reduced overdose mortality.
And while physical exams are ideal in many situations, whether healthcare is delivered in person or through telehealth is a poor proxy for quality. The DEA’s proposal to flag all prescriptions issued by telemedicine implies that telemedicine care is inferior. It also renders prescriptions suspect at a time when major pharmacy chains have declined to fill telemedicine prescriptions and when people who need medications for ADHD already face supply scarcities and other limiting policies.
Who gets access to medication should not come down to geography, identity or wealth, nor should government proposals compound existing disadvantages. The DEA and the Biden administration have the authority to let telehealth prescribing continue as is. It’s only a matter of will.
Kate M. Nicholson is the executive director of the National Pain Advocacy Center, a nonprofit that advocates for the health and rights of people with pain. Leo Beletsky is a professor of law and health sciences at Northeastern University and faculty director of the Action Lab at the Center for Health Policy and Law.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.