Medical experts decline to endorse cognitive screening for older adults
- Share via
A leading group of medical experts is declining to endorse cognitive screening for older adults, fueling a debate that has simmered for years.
The U.S. Preventive Services Task Force said Tuesday it could neither recommend nor oppose screening because there was insufficient scientific evidence of the practice’s benefits and harms. The task force called for more research to address that gap.
The group’s work informs policies set by Medicare and private insurers. Its recommendations were published Tuesday in the Journal of the American Medical Assn., along with an accompanying scientific statement and two editorials.
The position statement comes amid mounting concern over a rising tide of older adults with Alzheimer’s disease and other forms of dementia. Nearly 6 million Americans have Alzheimer’s disease, and that population is expected to swell to nearly 14 million by 2050. Unfortunately, treatments remain elusive.
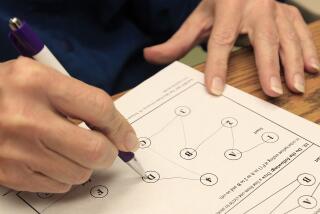
Cognitive screening involves administering short tests — usually lasting five minutes or less — to people without any symptoms of cognitive decline. Depending on the test, people may be asked to recall words, draw a clockface, spell a word backward or sort items into different categories, among other tasks. It’s an effort to bring to light problems with thinking and memory that otherwise might escape attention.
Proponents of screening say that testing seniors without any symptoms can help identify people with unrecognized difficulties and potentially lead to better care. It can also give them more time to plan for their future, medically and financially.
“This can start a discussion with your doctor: ‘You know, you’re having problems with your cognition, let’s follow this up,’” said Stephen Rao, an Alzheimer’s researcher with the Cleveland Clinic’s Lou Ruvo Center for Brain Health.
Opponents counter that the benefits of screening are unproven and the potential for harm is worrisome.
“Getting a positive result can make someone wary about their cognition and memory for the rest of their life,” said Benjamin Bensadon, an associate professor of geriatric medicine at the University of Florida College of Medicine.
The task force’s evaluation focused on universal screening for all adults age 65 and older without symptoms of cognitive decline. It found a lack of high-quality evidence that such screening would improve quality of life for older adults or ensure that they get better care, among other outcomes.
The task force’s stance is controversial, given how poorly the healthcare system serves seniors with memory and thinking problems. Physicians routinely overlook cognitive impairment and dementia in older patients, failing to recognize these conditions at least 50% of the time, according to several studies.
When the Alzheimer’s Assn. surveyed 1,954 seniors in December 2018, 82% said they thought it was important to have their thinking or memory checked. But only 16% said physicians regularly checked their cognition.
What’s more, Medicare policies appear to affirm the value of screening. Since 2011, Medicare has required that physicians assess a patient’s cognition during an annual wellness visit if the patient asks them to do so. But only 19% of seniors took advantage of this benefit in 2016, the most recent year for which data is available.
Dr. Ronald Petersen, director of the Mayo Clinic’s Alzheimer’s Disease Research Center, cautioned that doctors shouldn’t be discouraged from evaluating older patients’ memory and thinking.
“It would be a mistake if physicians didn’t pay more attention to cognition and consider screening on a case-by-case basis,” said Petersen, who co-wrote one of the JAMA editorials.
Similarly, seniors shouldn’t avoid addressing worrisome symptoms.
“If someone has concerns or a family member has concerns about their memory or cognitive abilities, they should certainly discuss that with their clinician,” said Dr. Douglas Owens, the task force’s chairman and a professor at Stanford University School of Medicine.
As the task force conducted its review, high hopes had rested on a study by researchers at Indiana University involving 1,723 older adults who were screened for cognitive impairment and 1,693 who were not.
After one year, seniors in the screening group were not more depressed or anxious than their counterparts who weren’t screened — important evidence that the assessment isn’t harmful. But the people who were screened did not have a better health-related quality of life. Nor did they experience lower rates of hospitalizations or emergency department visits. The findings were published in December in the Journal of the American Geriatrics Society.
“What seems clear is that screening in and of itself doesn’t yield benefits unless it’s accompanied by appropriate diagnostic follow-up and care,” said study leader Nicole Fowler, associate director of the Center for Aging Research at Indiana University’s Regenstrief Institute. Only one-third of the seniors who tested positive for cognitive impairment opted to undergo further evaluation.
And with shortages of geriatric psychiatrists, geriatricians, neuropsychologists and neurologists, there aren’t enough specialists to handle the demand that would arise if universal screening for cognitive impairment were implemented, warned Dr. Soo Borson, a researcher at the University of Washington who developed the Mini-Cog, a common screening test.
Screening should not be confused with diagnosis. The tests considered by the task force can only flag potential problems.
If results indicate reason for concern, a physician should ask knowledgeable family members or friends what’s going on with an older patient.
“Are they depressed? Having problems taking care of themselves? Asking the same question repeatedly?” said Dr. David Reuben, director of UCLA’s Alzheimer’s and Dementia Care program.
A comprehensive history and physical examination should follow to rule out potential reversible causes of cognitive difficulties, which are implicated in about 10% of cases. These include sleep apnea, depression, hearing or vision loss, vitamin B12 or folic acid deficiencies, alcohol abuse and side effects from anticholinergic drugs or other medications.
Once other causes are ruled out, neuropsychological tests can help establish a diagnosis.
“If I detect mild cognitive impairment, the first thing I’ll do is tell a patient I don’t have any drugs for that but I can help you compensate for deficits,” Reuben said. About 50% of patients with MCI develop dementia within five years of being diagnosed, but the other 50% don’t, he added.
If you’re a family member of an older adult who’s resisting getting tested, “reach out privately to your primary care physician and express your concerns,” said Dr. Timothy Holden, a geriatric medicine specialist at Washington University School of Medicine in St. Louis. “And let your doctor know if the person isn’t seeing these changes or is resistant to talk about it.”
This happens frequently because people with cognitive impairments are often unaware of their problems. “But there are ways that we, as physicians, can work around that,” Holden said. “If a physician handles the situation with sensitivity and takes things one step at a time, you can build trust and that can make things much easier.”
Judith Graham writes for Kaiser Health News, a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.