Choice of Transplant Recipients Poses Dilemma in Heart Cases
- Share via
It was a matter of timing.
Two weeks ago, when surgeons at UCI Medical Center transplanted the heart of a brain-dead El Toro Marine into a 26-year-old Huntington Beach musician, someone else could have used the same heart.
The other patient is a middle-age Orange County doctor. Seriously ill with congestive heart failure, he has been waiting for a new heart since Jan. 9 when doctors at Hoag Memorial Hospital entered his name in a computer registry of Southern California heart transplant candidates.
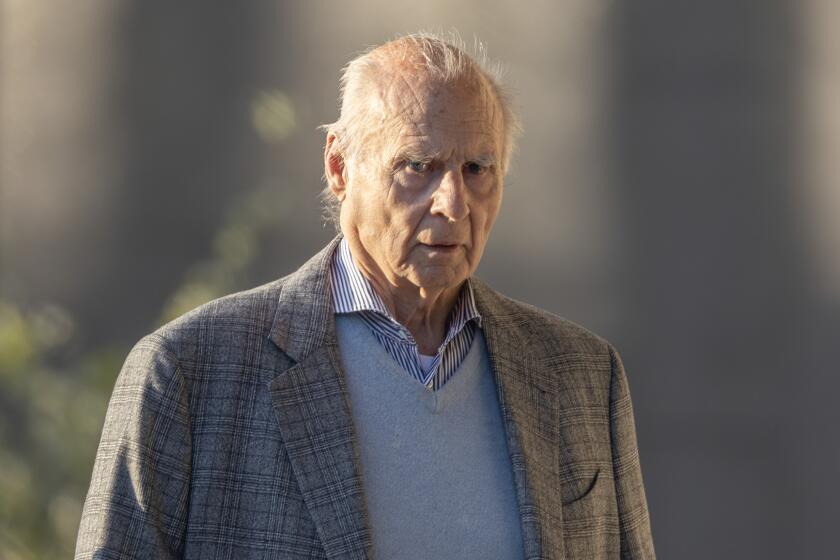
The dead Marine’s heart probably would have been “a good match” for Hoag’s patient, said cardiac surgeon Douglas Zusman. He estimated that it could have sustained a man weighing about 180 pounds--the size of their patient--and it was the right blood type--O. But when the dead Marine’s heart became available two weeks ago, Zusman’s patient was second on the Orange County transplant list.
Although the condition of Zusman’s patient had deteriorated--he had been able to live at home when he was first placed on the list but for the last month has been hospitalized--UCI Medical Center’s patient, musician Scott Headding, was also seriously ill with cardiomyopathy, a disease of the heart muscle.
And Headding had priority for the heart. His name had been placed on the official transplant list Jan. 7, just two days before that of Zusman’s patient. So Orange County’s first heart transplant was performed at UCI Medical Center, not at Hoag.
“I was disappointed for our patient,” Zusman said. “But their patient was first on the list . . . so nothing could have been changed.”
The interest in a dead Marine’s heart points up a serious problem for patients who need a heart transplant: There are many more people waiting for a new heart than donors who can provide a match.
Throughout the nation, 846 people--20 from Southern California-- are on waiting lists for a heart transplant, according to the federal and regional networks that allocate donor hearts.
Fully a third of those patients will probably die while waiting, said Bob Bowie, a spokesman for the United Network for Organ Sharing in Richmond, Va. “It’s kind of dismal. It’s a shame to keep reporting this. But we desperately need heart donors.”
National statistics were unavailable for 1987, but 108 heart transplants have been performed through March of 1988, Bowie said.
In the Los Angeles area, only seven were performed through March, compared to 14 in a similar period the previous year.
At the moment, Hoag’s heart transplant candidate is first on the Southern California list--ahead of another transplant candidate at Hoag, one waiting at UCI Medical Center and 18 other heart patients in Los Angeles area hospitals. Nervous about the transplant surgery, Hoag’s candidate has asked not to be identified until after the operation, his doctors have said. But they and the local organ transplant network officials describe his need for a new heart as “urgent.”
Even so, he could be bumped from first place anytime by someone who needs a heart-lung transplant or a patient whose blood type or body weight is a better match for the next available donor heart, noted Barbara Schulman, transplant coordinator for the Los Angeles agency that allocates donor organs, the Regional Organ Procurement Agency of Southern California.
“This is sort of a funny business,” said Dr. Richard Ott, the cardiac surgeon who heads UCI Medical Center’s transplant team. “You’re waiting around for an opportunity (for an available heart), but an opportunity means that someone has had a tragedy.”
There has always been a shortfall of donor hearts, transplant experts say, but for reasons that are not clear, the shortfall this year appears to be more severe than usual.
Bowie, spokesman for the Virginia network, said his organization has been hearing complaints recently from Southern California, Texas, Florida and Georgia that organ donations are down.
New seat belt laws may have reduced the supply of available hearts. Without seat belts, accident victims were likely to die from head injuries but their hearts were undamaged. Now, the victims of severe accidents may suffer abdominal and chest injuries caused by the belts that make their hearts unsuitable for transplantation, Bowie said.
Also, he said, there may be some “backlash” from a federal law that took effect last November requiring all hospitals to approach family members of a brain-dead patient and invite them to donate his organs.
“It would be easy to imagine a situation where a hospital staffer says, ‘Look, I’m required by law to ask if you will donate your son or daughter’s organs for transplant.’ If you ask the question negatively, the response will probably be: ‘I’m not going to donate.’ ”
Schulman, the Los Angeles-based transplant coordinator, agreed. For the last two years, California hospitals have been required to ask families about organ donation, but the request has to be made with sensitivity. “They may be asking prematurely, before the family has had an opportunity to absorb and understand brain death,” and so will be rejected, she said.
Schulman said her agency also maintains transplant coordinators at hospitals in Orange, Kern, Santa Barbara, Ventura and Riverside counties who are trained to ask grieving families about organ donation.
If family members agree, they receive a personal letter several days after the organ has been transplanted with the age, occupation and some medical background about the person who received it, Schulman said.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.