Coronavirus infection rate in L.A. County is falling. But it’s still in the danger zone

- Share via
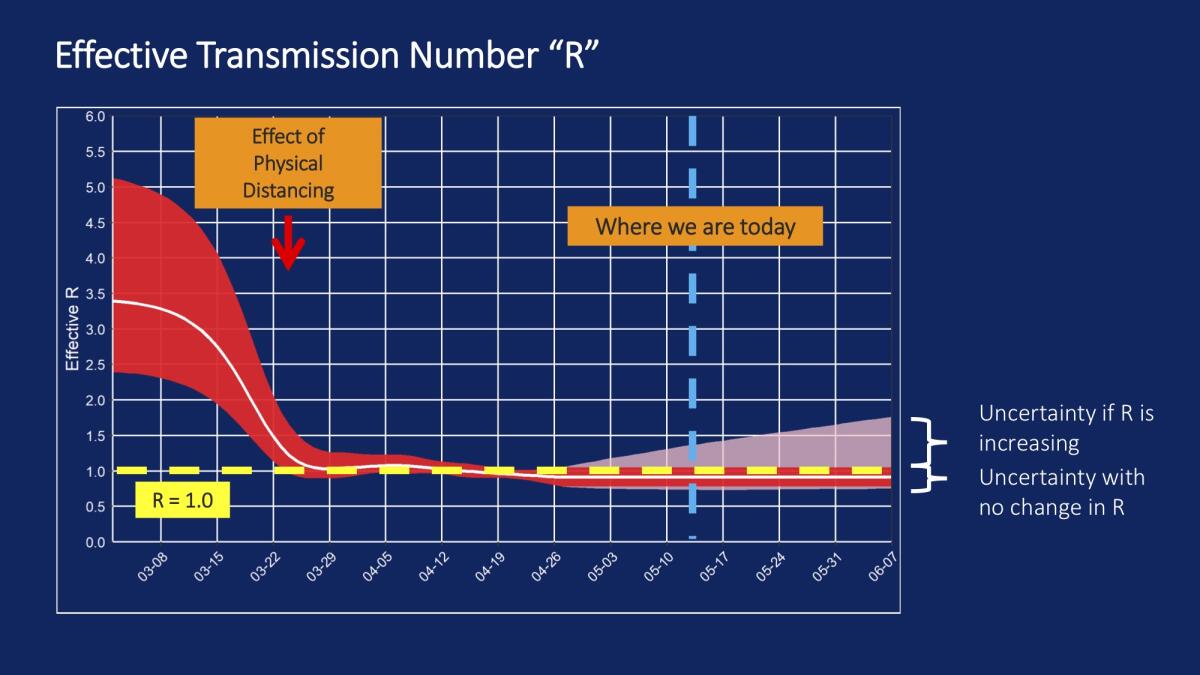
As Los Angeles County found itself in a coronavirus crisis in March, it became clear the highly infectious disease was surging out of control, with every one person testing positive for the virus infecting an average of 3½ other people.
Last week, L.A. County officials released data showing remarkable progress: The infection rate has fallen. Instead of every patient infecting an average of more than three other people, every infected person in L.A. County now infects just one other person.
Among L.A. County public health experts, this number is called “R,” which stands for the Effective Transmission Number of the disease. This number can change when the public takes steps to change behaviors, such as adhering to a stay-at-home order.
The fact that the disease was spreading from one infected person to more than three others represented “a high rate of spread, much faster than what is seen, for example, with seasonal influenza,” Dr. Christina Ghaly, director of health services for L.A. County, said Thursday.
Officials believe the drop is tied to stay-at-home orders imposed in late March.
“This represents tremendous progress, and we should all be very proud. It is also what allows us to start easing health officer orders and the restrictions that we’ve all been living with for the past several weeks. Safer at Home bought us time,” Ghaly said.
“It allowed our healthcare system to become more prepared. It allowed time for testing to be ramped up. It allowed time to prepare to do more contact tracing efforts, and it showed the power of what we can all do to protect ourselves and one another,” Ghaly said.
But the fact that the Effective Transmission Number hasn’t fallen below 1 also poses a challenge. It explains why the coronavirus has stubbornly persisted at a plateau in California. If every person who gets infected on average infects one other person, then the disease levels will remain constant.
L.A. County’s rate is the same as is now reported in Silicon Valley, home to Northern California’s most populous county, Santa Clara County, an early hot spot of the statewide outbreak.
Health officers in the Bay Area on Monday said they have seen a number of positive signs since the last loosening of stay-at-home orders executed on May 4, which allowed all construction and certain businesses that primarily do work outdoors, such as gardening and landscaping, to resume.
“We make one change, watch the indicators, and when we haven’t seen that uptick, then we take the next step and then we watch again,” said Dr. Sara Cody, Santa Clara County’s health officer.
Santa Clara County was the initial epicenter of the health crisis in California. Now its cases amount to 3% of the state’s total and its deaths 4%. In early April, 9% of people tested in the county were positive for the virus, Cody said. Now the rate is 1% to 1.5%, “a very significant improvement,” Cody said.
Dr. Grant Colfax, San Francisco’s health officer, also said his city was seeing progress.
As long as San Franciscans continue to social distance, practice good hygiene and wear masks, reopening businesses could continue.
“So far the game is going relatively well,” Colfax said Monday. “But we are only in the second inning of a long game.”
He said the virus will remain a threat in San Francisco for at least the next 18 months.
Los Angeles remains the center of coronavirus in California, with more than 1,800 deaths.
Ghaly said Los Angeles County will need to closely monitor the rate of disease spread. If the Effective Transmission Number starts to tick upward, it’s possible that L.A. County will need to reimpose stronger stay-at-home measures. That would be expected if people aren’t careful in staying away from others or stop avoiding social gatherings or wearing masks.
If the Effective Transmission Number rises substantially, it’s possible the county could again be threatened with having so many critically ill patients, it exceeds the number of intensive care unit beds.
Officials are starting to see a decline in the number of coronavirus patients in the ICU.
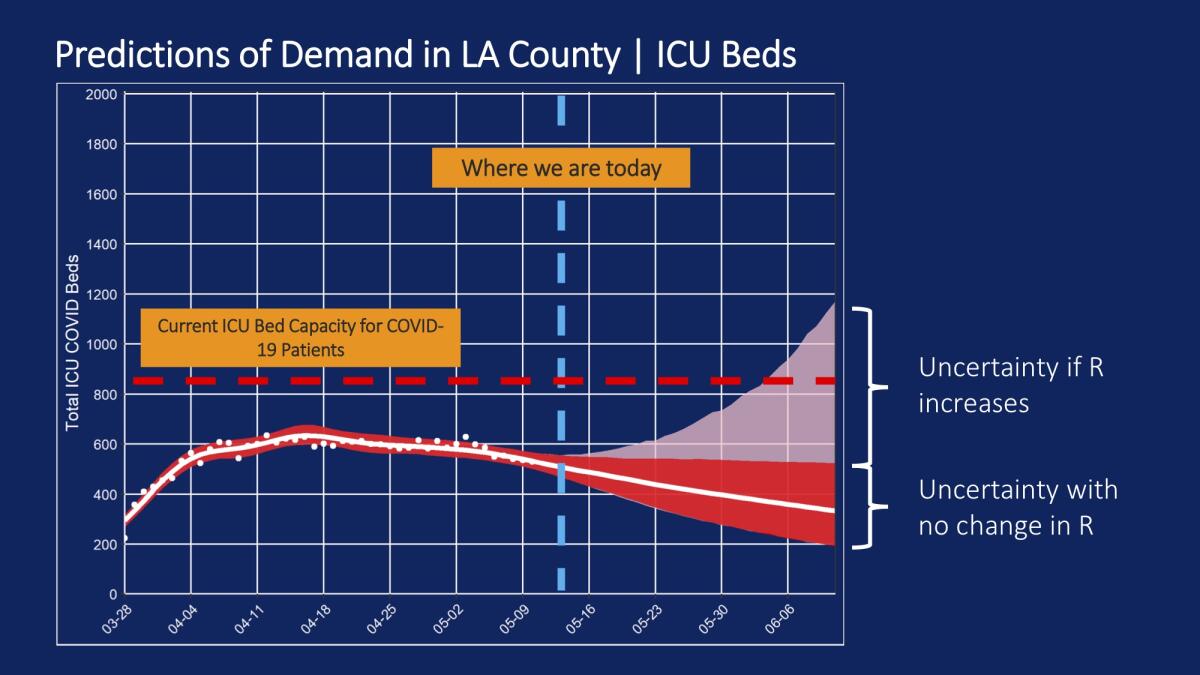
There is an added potential problem: It can take two to four weeks before hospitals start seeing a surge in patients after they’ve been infected, so it can take some time before officials realize what’s going on.
Ghaly said L.A. County residents can’t simply get back to life as they once knew it right now “because so many of us across the county are still susceptible to COVID-19,” she said. If people did go back to old habits, she said, “then we will experience a rapid increase in cases and that will require drastic action that none of us want to revisit.”
“The better question is what we can do to get back to work and get back to our lives in ways that still protect our families and our community,” Ghaly said. “Both are important for our overall health and well-being, and for the vibrancy of our community. And both are very possible.”
The strategy, Ghaly said, includes:
- Accepting that masks will need to be used in public
- Practicing physical separation when outside the home
- Continuing to wash hands and cleaning frequently touched surfaces
- Being cautious around older people or those with underlying health conditions
- Respecting new rules in venues that commonly have placed people close to one another, such as restaurant dining rooms, when they reopen
- Following isolation and quarantine rules when sick or exposed to a sick person
- Increased testing for at-risk populations
Federal officials have said they expect it will take 12 to 18 months at the earliest to see a vaccine. And they’ve warned about a surge of cases that may come in the fall.
“We are not going to get back to the normal, the way it was,” Ghaly said. “But we can and will get to a place that allows everyone to earn a living, to take care of themselves and their family, to find enjoyment in their lives. And then that allows us to be healthy at the same time.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.















