While crowds are out shopping, at L.A.’s hospitals, ‘It feels like we’re drowning’
- Share via
Dr. Adupa Rao will be at work on Christmas Day, and the day after that, and the day after that, because as much as he’d like to be home with his family, the current monstrous wave of COVID-19 patients won’t allow him time off.
“It feels like we’re drowning here,” said Rao, a pulmonologist and critical care specialist at Keck Hospital of USC.
And there’s a fear that if the post-Christmas increase in cases is anything like the post-Thanksgiving bump, the worst may be yet to come.
“I look around at my colleagues’ faces and there’s a hollowness in their eyes, a fatigue,” said Rao. “There’s a resounding feeling of, ‘What’s next, and how do I brace myself for what’s next?’”
I think we owe Rao and his medical colleagues an apology. Better yet, we owe them more responsible behavior. At the worst moment in the most horrific pandemic in a hundred years, too many of us aren’t playing it safe. In recent days, airport traffic has spiked and shopping malls are bustling, even as the L.A. County death toll hit 9,000.
Rao and four other frontline healthcare workers appear in a public service video released this week by Keck, Cedars Sinai, Dignity Health, Providence and UCLA Health. In it, they talk about the onslaught of new cases, which has exhausted frontline staff, and ask people to play it safe during the holiday stretch between now and New Year’s weekend.

Doctors, nurses and frontline staff from Southern California talk about the challenges they face due to COVID-19 and how the public can help slow the spread of the virus this holiday season.
“We have more COVID patients than what we’ve ever seen,” says UCLA emergency room doctor Medell Briggs-Malonson. “Please do us a favor. Take care of yourself, take care of each other, so that you can take care of us, and help to save lives.”
I first spoke to Rao and two of his colleagues in July, when the man in the White House was refusing to wear a mask and legions of people were flouting common-sense advice from public health experts on how to slow the spread of the virus. At the time, Rao and the others described to me in graphic terms the suffering of critically ill COVID-19 patients who were unable to see loved ones in their final moments because of forced isolation.
This week, I circled back to Rao, Dr. Sunita Puri, and emergency room nurse Manny Khodadadi for an update on what’s happening on the front lines as the percentage of available critical care beds dropped to zero and Los Angeles County health officials and hospital staffs scrambled to accommodate roughly 700 new patients daily, a nearly fivefold increase since October.
“Every day, I get texts and phone calls to do an overtime or go in and help cover on lunches and other breaks,” said Khodadadi. He told me he struggles to find the right balance, wanting to help out by logging extra shifts, but without working so many hours that he’s not fully alert when patients roll into USC Verdugo Hills Hospital.
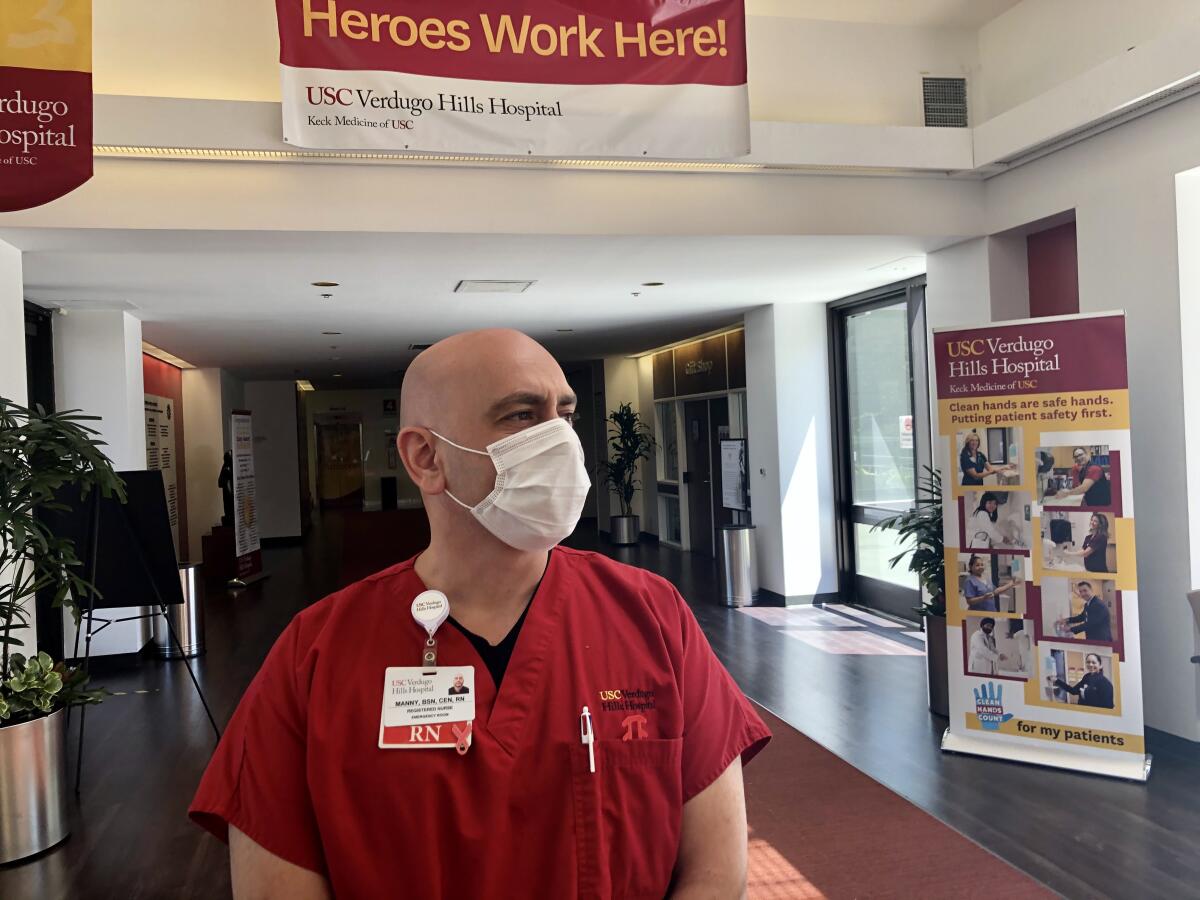
Khodadadi said that in the current surge, patients have told him they attended Thanksgiving celebrations or other gatherings and soon began getting cold and flulike symptoms.
“I try to stay neutral,” Khodadadi said. “I don’t want to judge people, because I have to take care of them.”
But negligent behavior puts a lot of people at risk, including frontline workers and their families. Khodadadi’s wife Jennifer, a property manager and former history teacher, told me it’s upsetting to watch rallies of unmasked people or read about those who resist safety protocols. That’s not just because her husband is an ER nurse and her brother is an ER doctor in Texas, she said, but because the youngest of her three children is immunocompromised.
“We’re very protective of our daughters,” Jennifer said, and Manny has always been extremely particular about changing, showering and washing his scrubs after work. “But as far as the public, we can’t control anyone else.”
Puri, a palliative care specialist at Keck, said the current crush of patients is “emotionally much more intense” for medical staff, because it didn’t have to be this bad.
“We feel like what we’ve seen this year should have been warning enough for people to be a little more careful with things like traveling, wearing masks, all the important preventive things … and sadly we haven’t seen that,” said Puri. “There’s this tremendous suffering that could have been prevented if we had banded together as a country.”
At Keck Hospital, Puri said, the overwhelming number of patients in COVID critical care are Latino, “and I think that says a lot about the inequalities faced by this group.”
It says, in part, that many of them are essential workers exposed to high risk on the job, and that many live in multigenerational households and can’t easily isolate when sick. And the pandemic has been particularly brutal for low-income people who don’t have easy year-round access to quality healthcare and are more likely to have health problems such as diabetes and hypertension.
The U.S. death toll is now at roughly 325,000, and L.A. County is averaging about 85 daily COVID-19 deaths in recent days. The loss is so great that we’re at risk of being desensitized by such statistics unless we’ve lost a loved one or we’re in the trenches.
“When you’re in the thick of it, and seeing people dying in front of you, that means more than looking at the death rate on a piece of paper,” said Rao.
Rao said he has no doubt this surge is directly related to Thanksgiving travel and gatherings, given the incubation period and the spread of the disease by those who were exposed. He said the challenge of caring for the crush of patients is all the greater because so many “nurses and physicians are getting infected” and have been forced to miss work.
And he’s anticipating yet another surge that runs through January and into February because of Christmas and New Year gatherings.
“That’s all weighing on our minds and it’s extremely frustrating and defeating to know that we have people who can step up and try to prevent this by wearing a mask and staying isolated as much as possible, and people won’t do it. They can’t do it or they won’t do it, whatever it is. The bottom line is that it’s not getting done,” said Rao.
Human nature being what it is, we know that many virus-fatigued people are going to get together with families and friends. And if they insist, they owe it to each other and everyone else to be as smart about it as possible, to respect science and medicine, to meet outdoors and maintain distance.
In fact, until the vaccines are available to the general public, that’s still the best way to limit the spread and get to where businesses can reopen.
Rao is taking no such chances, though, other than reporting for duty. He said that during this holiday season he’d love to see his parents (his father is also a physician), who live just a half-mile from him. But it’s not worth the risk.
“I know we’re not a great society when it comes to delayed gratification; we want instant gratification,” Rao said. “But people have to decide whether they want to see their loved ones for one more holiday season, or they want to see them for many more, into the future.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.














