Families of prisoners hospitalized with COVID-19 say they’re not notified until too late

- Share via
By the time Santos Ruiz heard from the prison doctor last July, his father had been at St. Francis Memorial Hospital in San Francisco for two weeks and on a ventilator.
“We don’t think he’s going to make it,” he recalled her saying.
This was the first time Ruiz had heard that his father, a 61-year-old inmate at San Quentin State Prison, even had the virus.
“It wasn’t right,” Ruiz said. “They waited to a point where a person can’t talk, a person can’t communicate with his family that loved him.”
As the pandemic has ravaged California prisons, some families say that officials have failed to inform them when their loved ones have been hospitalized with the virus — receiving a call only when it might already be too late to say their goodbyes, act as surrogate decision-makers or provide critical emotional support.
State law requires the California Department of Corrections and Rehabilitation to use “all reasonable means” to notify an inmate’s designated contacts in the case of a death, serious illness or serious injury.
The law does not say when exactly the prison must alert families — the CDCR’s operations manual says “as soon as possible” — or what’s deemed a serious illness.
In a statement, prison system officials said they have worked with hospitals to facilitate video calls between incarcerated patients and families, noting that they “understand the desire for friends and family … to stay informed of their loved one’s healthcare status, particularly during the COVID-19 pandemic.”
When asked to address claims that families are not notified promptly of hospitalizations and that coronavirus-related hospitalizations should be indicative of a serious illness, the CDCR and the California Correctional Health Care Services agency pointed to state notification policy and said they could not comment on specific cases because of medical privacy laws.
“I know it’s hard to understand, but not hearing from the institution, is a good thing,” a prison official wrote in an email to Jennifer Chacon of Corona, who said her husband, an inmate at Kern Valley State Prison, battled the coronavirus at an outside hospital for weeks without her knowing.
Prison advocates, who have long argued that a hospitalization should trigger an emergency notification, say the issue has come up often during the pandemic. They point to how COVID-19 has killed more than half a million people nationwide. Across California, 211 prisoners have died.
“There’s a fundamental human dignity to allow someone to communicate with their loved ones when they know they’re dying,” said Michael Bien, a leading Bay Area attorney for prison mental health issues.
Health experts also say that contact with loved ones might help patients. Dr. Marwa Kilani, director of palliative care at Providence Holy Cross Medical Center in Mission Hills, said doctors should not just give patients medication and “hope for the best.”
“To hear a loved one’s voice, to hear that they’re pulling for you, cheering for you, giving you that positive energy — who knows, it could have delayed you from being on a ventilator,” she said.

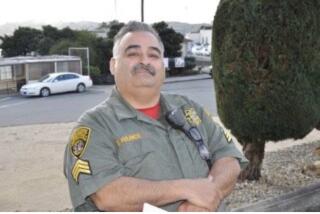
Daniel Ruiz, a father of six from Sacramento, was sentenced in January 2020 to four years in prison for possession of a controlled substance for sale and possession of a firearm by an ex-felon.
On June 22, a few days after testing positive for the virus, Ruiz was admitted to an outside hospital with worsening shortness of breath, according to medical records reviewed by The Times.
A week later, Ruiz consented to be placed on a ventilator, according to medical records.
The day after he was intubated, the hospital called San Quentin physician Shannon Garrigan, identified in records as Ruiz’s surrogate decision-maker. A staff member wrote that they spoke with her, given that Ruiz was “critically ill with multi-organ failure,” to request permission to contact his family.
Garrigan gave approval, but the staffer seemed to question whether personnel needed authorization from hospital administrators, records show. On July 2, a prison doctor provided consent for Ruiz to have a catheter inserted for dialysis.
When Ruiz’s family was informed of his condition July 6, two weeks after he was admitted, they wanted to be there for him.
Relatives gathered for videoconferences with Ruiz. The first time, he was heavily sedated, his son Santos Ruiz said. The second time, his eyes were open and he’d move his neck slightly.
“We wanted to let him know we were there,” said Patricia Caviness, 37, a niece who said Daniel Ruiz had been a father figure since her own dad had died when she was 3. “Everyone was telling him, ‘Daniel, fight, fight.’”
But on the morning of July 11, Santos and his brother Fernando drove from Sacramento to San Francisco to say goodbye to their father, who would be disconnected from the ventilator.
With his family watching remotely, Santos Ruiz passed along messages from relatives, hoping that his dad could still hear. He recited the Lord’s Prayer.
The brothers were driving back home when they learned their father had died.
The California Department of Corrections and Rehabilitation and Dignity Health, the hospital’s parent organization, declined to comment on Ruiz’s case, citing patient privacy laws. The CDCR would not comment on whether any policies prevent hospitals from contacting families of incarcerated patients.
Julia Sherwin, an attorney for the family, said it was “appalling” that a prison medical surrogate authorized procedures such as kidney dialysis and held that Ruiz’s medical records don’t indicate that he agreed to a prison surrogate decision-maker.
“After he agreed to go on the ventilator,” she said, “all medical decisions after that point should have been made by his family,” which has filed a claim against the prison system.
Dr. Leah Rorvig, director of health education at Amend, an organization at UC San Francisco that focuses on health issues affecting inmates, said having a prison medical professional act as an inmate’s surrogate decision-maker is “highly, highly unusual.”
Federal law entitles incarcerated patients to adequate medical care, which Rorvig said means contacting a patient’s family 24 to 48 hours after they are admitted to a hospital and allowing the patient to appoint surrogate decision-makers.
“It’s horrifying, it’s below the standard care,” she said of Ruiz’s family’s claim that they weren’t called for two weeks.
Some families learn from other inmates that their loved ones have been hospitalized.

Sandra Calac of Canoga Park said that on Dec. 31, a prisoner called her to say that her husband was having breathing issues.
Gary Calac, 65, was sentenced in 1996 to life with the possibility of parole for robbery and burglary. Before the pandemic, his wife would drive to Richard J. Donovan Correctional Facility in San Diego County regularly to visit him.
On New Year’s Day, another prisoner told her that Calac had been hospitalized.
She said a prison doctor called her Jan. 7, five days after she left a message for officials, and told her Calac had suffered a blood clot in his lungs.
“She says, ‘He’s probably going to be in the hospital longer,’” Sandra Calac said. “She made it sound like he’s OK.”
Two days later, she said, she received a call: Her husband had died of complications from COVID-19.
“The prison should have notified me, but it was his friends that called me and told me he was in the hospital,” she said. “I couldn’t believe he had gone so fast.”
Sharp HealthCare, parent organization of the hospital where Gary Calac died, would not comment on patient cases but said that it works with prison authorities to see if it can comply with an incarcerated patient’s request to notify an outside contact.
According to the CDCR, testing positive for the coronavirus does not meet criteria to notify families. Though the department says inmates in medical isolation are provided access to phones and mail, advocates say calls are sometimes more limited there.
“When they haven’t heard from them for two weeks,” said Vanessa Nelson-Sloane, director of Life Support Alliance, which advocates on behalf of inmates serving life sentences, “family members are left wondering, ‘Are they alive, is he dead?’”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.