Everyone in California seems to be sick with respiratory illness. Here’s why

- Share via
Does it seem like a lot of people you know are sick?
You’re not alone. Respiratory illness season is in full swing in California and across much of the nation.
In Los Angeles County, about 23% of people participating in a weekly text-message-based survey reported having a cough or shortness of breath for the week that ended Dec. 10, higher than the total reported during a late summer peak in respiratory illnesses, when 21% said they had those symptoms. Early summer brought a lull, with only 10% of survey respondents saying they had a cough or shortness of breath.
Meanwhile, coronavirus levels in wastewater in L.A. County are at their highest since summer.
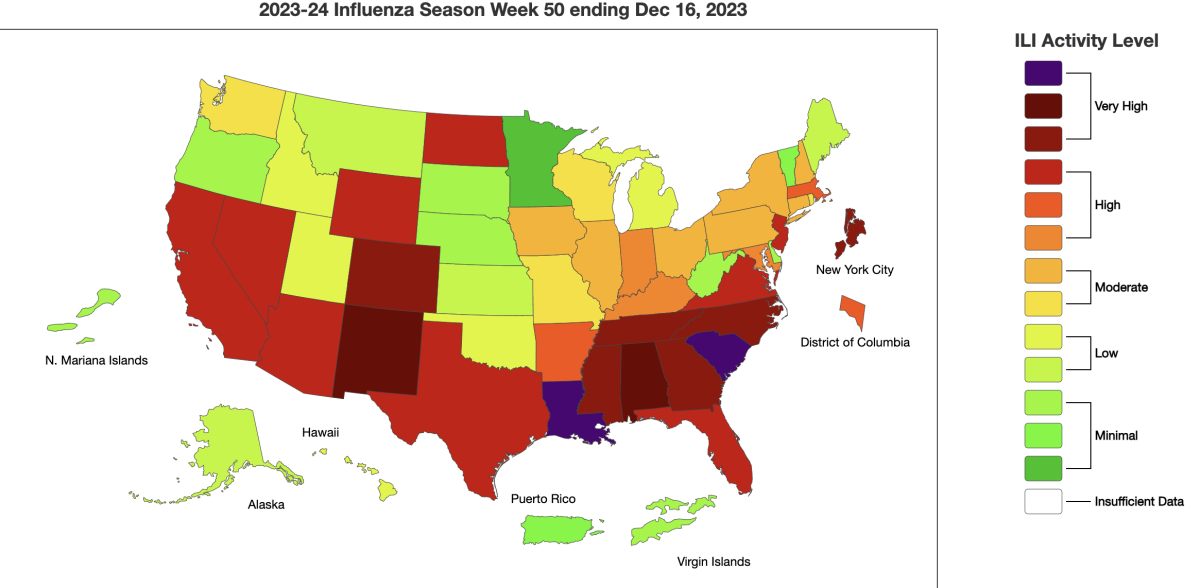
Statewide, the level of flu-like illness — which includes non-flu viruses such as the coronavirus — is considered high, according to the U.S. Centers for Disease Control and Prevention.
Nationally, COVID-19 remains the primary cause of new respiratory hospitalizations and deaths, resulting in about 1,000 fatalities a week.
Despite the chorus of coughs, the trend in terms of levels of virus in sewage and hospitalizations is milder than last year at this time. And the health infrastructure in Los Angeles and Orange counties, as well as the San Francisco Bay Area, are holding up well, with no sign yet of a major increase of patients needing intensive care.
With COVID-19, “it’s continuing to go up, but it’s not as dramatic as, certainly, even two winters ago or even last winter, yet. So time will tell if the numbers that we see continue to go up,” said Dr. Nancy Gin, regional medical director of quality and clinical analysis for Kaiser Permanente Southern California. “It’s not causing intensive care units to be full of COVID-related illness, which is good.”
Still, Gin and other doctors say there is reason to be on guard; they’re urging people to get their COVID-19 and flu vaccinations and asking sick people to say home and healthy people to avoid ill people. The latest ascendant coronavirus variant, JN.1, is particularly contagious and is spreading more widely. And with COVID-19 and flu still rising, and respiratory syncytial virus plateauing at a high level, it’s unclear how bad this year’s respiratory season will get.
“We have all these respiratory viruses afoot, with RSV that hasn’t really started to go down,” said Dr. Peter Chin-Hong, a UC San Francisco infectious-disease expert. “With flu, it’s just rising now. And then with COVID ... that’s increasing, for sure.”
And some parts of California are being hit harder than others. Fresno County’s Department of Public Health says its hospitals are seeing a sharp rise in respiratory illnesses and reporting “severely impacted conditions ... due to a historic number of admitted patients and people accessing the emergency department with non-urgent medical problems.”
The Sacramento area and the Eastern Sierra are at the “medium” level of coronavirus-positive hospital admissions, according to the CDC, while the rest of California’s counties are in the “low” level.
Coronavirus transmission is once again spiking in California entering the winter holiday season — and the new JN.1 subvariant may be partly to blame.
COVID-19
Coronavirus levels in Los Angeles County’s sewage were at 39% of last winter’s peak — the region’s last major spike — according to data for the week ending Dec. 9, the most recent available.
The rate at which coronavirus tests are coming back positive also continues to rise. About 11% of specimens tested at sentinel surveillance labs in L.A. County were positive for the week that ended Dec. 16, up from 10% the week prior.
In the San Francisco Bay Area, coronavirus levels in the largest sewershed in Santa Clara County have reached their highest point since last winter’s peak, at 72%, according to the local public health department.
At UC San Francisco’s hospitals, coronavirus-positive hospitalizations have been increasing and remain high, but are lower than this time last year, Chin-Hong said. As of Wednesday, there were 27 coronavirus-positive patients at those hospitals; by contrast, in mid-December, there were fewer than 20.
Across California, new weekly coronavirus-positive hospital admissions are at their highest levels since last winter. For the week ending Dec. 16, there were 2,924 new coronavirus-positive hospital admissions, up nearly 50% from a month earlier, according to data posted by the CDC.
This season has not — at this point — eclipsed last year’s COVID-19 levels in terms of the number of weekly hospitalizations. And doctors in Los Angeles County say they’re not seeing COVID-19 patients inundating intensive care units, although urgent care clinics are quite busy.
COVID-19 and flu are rising across California, sparking new warnings from health officials to take precautions as the wider winter holiday season looms.
Flu
Flu cases also continue to rise in California. According to the state Department of Public Health, there were 1,007 new flu hospital admissions for the week that ended Dec. 9, up 20% over the prior week.
The latest flu hospitalization level is about one-third the peak of last winter’s.
In Los Angeles County, about 18% of specimens tested at sentinel surveillance labs came back positive for the flu, compared with 14% from the previous week.
California’s respiratory virus season is ramping up, prompting officials to renew their calls for residents to get vaccinated in hopes of reducing pressure on hospitals.
RSV and other viruses
RSV can cause severe illness and death in babies and older people. It has plateaued at a relatively high rate in L.A. County. For the week that ended Dec. 16, about 12.3% of specimens tested at surveillance labs came back positive for RSV, about the same as the prior week’s reading of 12.5%.
The positive test rate for RSV in in the county has been mostly between 12% and 13% since early November, with a one-week peak that reached 15%. That represents a particularly active RSV season.
Since the 2017–18 season, there have been just two other seasons in which the positive rate has been higher: last year’s terrible season, which plateaued at a peak rate of about 20%, and the 2018–19 season, which leveled off at a maximum of about 15%.
There are other viruses also causing illness, including rhinoviruses and enteroviruses. Most people who get these viruses develop a common cold. In Los Angeles County, 15% of surveillance-lab-tested specimens are coming back positive for rhinoviruses or enteroviruses.
Emergency rooms
In Los Angeles County, for the week that ended Dec. 17, about 5% of emergency room visits were classified as related to the coronavirus, just enough to warrant a medium level of concern.
That’s not as bad as it was last year at this time, when roughly 13% of emergency room visits were classified as related to the coronavirus.
What you can do
Doctors believe more people became infected with respiratory viruses over the Christmas holiday.
Wearing a mask can help sick people avoid spreading viruses to others and lower the risk of healthy people getting sick.
Many people who test positive for the coronavirus or the flu are eligible for antiviral drugs, such as Paxlovid for COVID-19 and Tamiflu for the flu. The medications can reduce the severity of illness.
A program funded by the National Institutes of Health, featured at test2treat.org, gives adults who test positive for COVID-19 or flu free access to telehealth care and treatment. Those who aren’t positive can still enroll to get free tests shipped to them if they are adults and uninsured or underinsured; on Medicare, Medicaid or Medi-Cal; or in the healthcare system of the Department of Veterans Affairs or the Indian Health Service.
Californians who don’t have insurance or have a hard time getting anti-COVID-19 medication can get a free COVID-19 telehealth appointment and medication by calling (833) 686-5051 or going to sesamecare.com/covidca to request an appointment. L.A. County residents can do the same by contacting the county’s Public Health Call Center at (833) 540-0473, which is open seven days a week from 8 a.m. to 8 p.m. but closed on New Year’s Day.
Doctors are also urging people to get a fresh vaccination for COVID-19 and flu this winter. Generally speaking, if you haven’t gotten a new vaccination for either virus since September, it’s time for a new one.
RSV immunizations are also available for babies, those who are pregnant and people who are 60 or older.
People who test positive for the coronavirus should isolate for at least five days after the onset of symptoms or their first positive test, whichever comes first. The day a person starts having symptoms or had their first positive test is considered Day Zero, and the earliest a patient can exit isolation is by the end of Day 5.
Infected people can end isolation after Day 5 if they have been free of fever for 24 hours without using fever-reducing medications and if they don’t have any other symptoms, or if their symptoms are mild and improving, according to the L.A. County Department of Public Health.
The agency strongly recommends people get a negative rapid test result before ending isolation between Days 6 and 10. Isolation can generally end after Day 10 without needing a negative test result, unless you still have a fever.
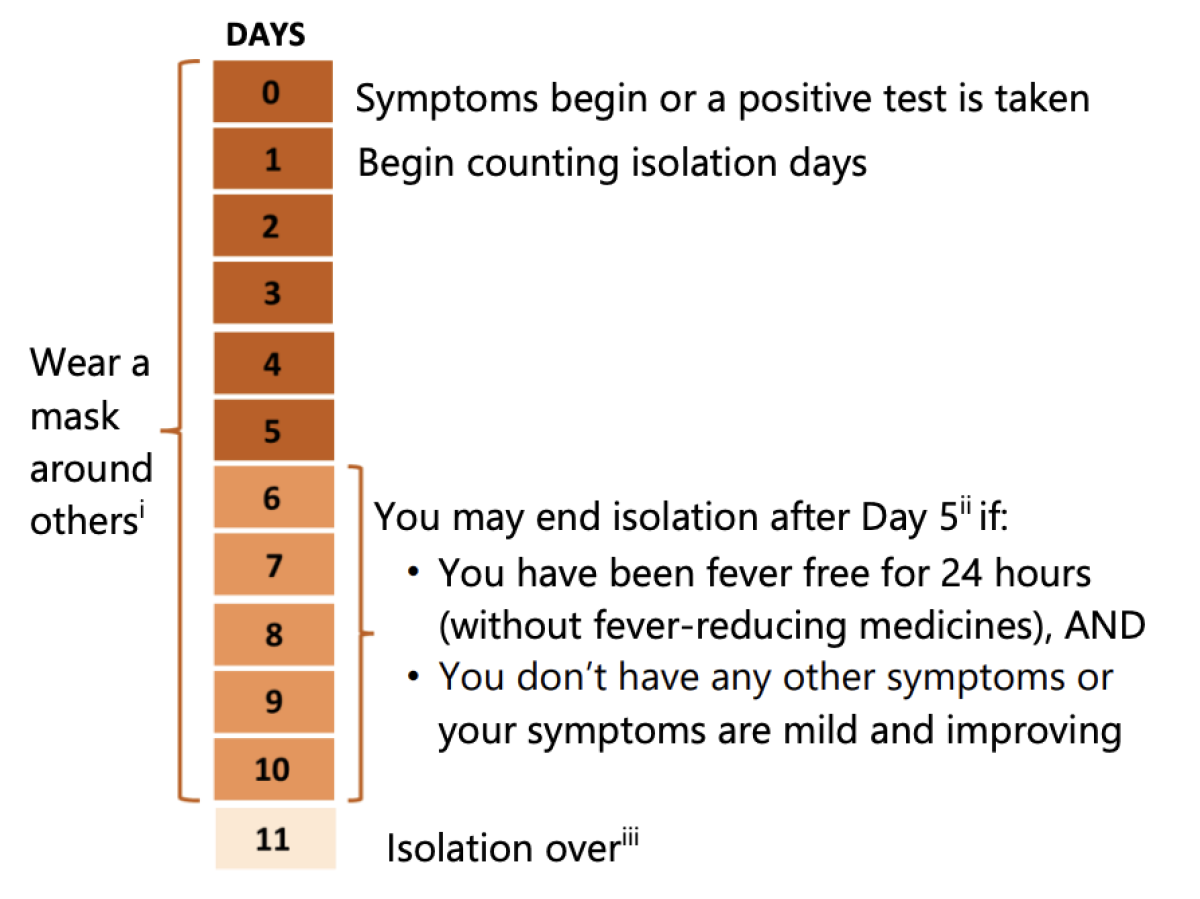
Infected people are encouraged to wear a mask around others for 10 full days after the onset of symptoms or their first positive test result. But the agency says people who meet the criteria to end isolation after Day 5 can stop wearing a mask too if they have two consecutive negative test results taken at least one day apart.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.

















