My small medical practice was struggling. And then the coronavirus pandemic hit
- Share via
For more than 20 years, I’ve run an allergy-asthma practice in Upland, and every year it has gotten tougher to keep small independent medical practices like mine afloat.
Well-meaning regulations to protect patients are designed with large health systems in mind, but they are heavy burdens on small doctors’ offices. Financial reimbursements from insurance companies have been decreasing, relative to inflation. Without the leverage to negotiate rates, small practices are at the mercy of these payers.
And then the coronavirus pandemic hit.
A month ago, our office followed guidelines to cancel non-urgent procedures and institute social distancing within our offices. This means far fewer patients, but we need to stay open — it’s allergy season and patients still depend on us.
Some need to maintain their allergy-shot schedules. Others fear an asthma attack could land them in the hospital and expose them to the coronavirus. We’re here to keep them out of the ER — and to reduce the burden on our hospitals.
Unable to secure face masks to protect our office staff, we turned to telemedicine. But about the same time, I developed an illness that had many signs of COVID-19 — fever, headaches, body aches, shortness of breath. On my sick bed, I studied webinars and articles on the latest medical recommendations for dealing with COVID-19.
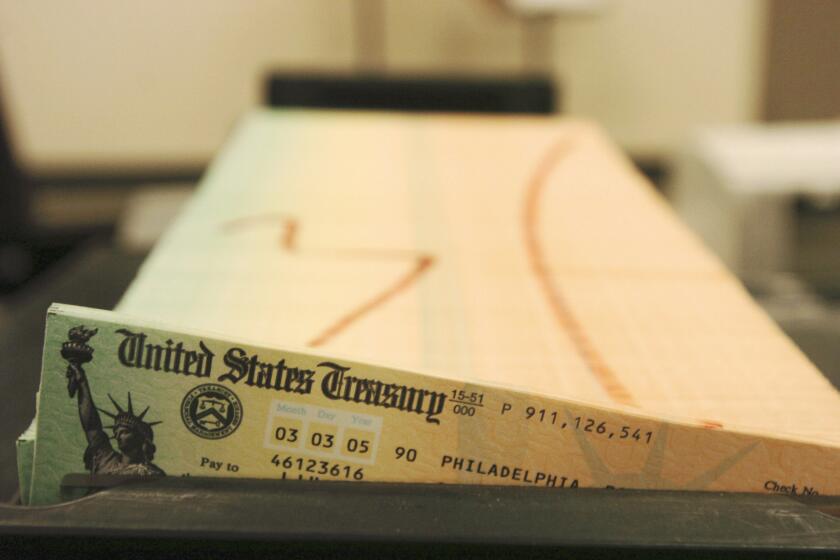
I also watched teleconferences on programs to help small businesses. I applied for the Paycheck Protection Program, designed to help small businesses keep workers on the payroll during the economic shutdown caused by the pandemic. The program ran through $310 billion before it could help my business. I’m waiting to hear if I get funded in round two.
It appears most of the loans went to the well-connected; mom-and-pop businesses had no chance. I tried to reassure my staff they would get paid because we had enough funding to last a month and, besides, loans would bridge the gap. Now that month has gone by, and our office generated almost no revenue in that time.
A recent California Medical Assn. survey reveals that 95% of physician practices are worried about their financial health, and 75% experienced a revenue decline of 50% or greater due to the COVID-19 public health emergency.
One thing I’m thankful for: I have recovered from my illness. But without the full-time patient load and non-urgent procedures, my practice will have a tougher time.
This pandemic might be the tipping point for solo practitioners. Large medical systems do have some advantages, like multiple specialists in one location and easier coordination of care. Yet some people prefer seeing their neighborhood doctor, where everybody knows their name. Half of my employees have been with the office for at least a decade.
If you think helping small medical offices survive is important, please let your state legislators and congressional representatives know.
We’re facing a choice: Are we going to allow this type of personal care to disappear?
Dr. Sunil Saini is an allergy and asthma specialist in Upland and a volunteer associate clinical professor at UC Irvine.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.