Coronavirus Today: More good news on the vaccine front
- Share via
Good evening. I’m Amina Khan, and it’s Monday, Nov.16. Here’s what’s happening with the coronavirus in California and beyond.
Folks, let’s start off your week of coronavirus news on a good note: Initial data on the COVID-19 vaccine developed by Moderna shows that it appears to be 94.5% effective in a major clinical trial. That announcement follows similar news last week from drug giant Pfizer, which said its experimental vaccine looks to be 90% effective. Both companies are on track to seek authorization for emergency use in the United States within a matter of weeks.
“That should give us all hope that actually a vaccine is going to be able to stop this pandemic and hopefully get us back to our lives,” said Moderna president Dr. Stephen Hoge. The fact that two companies are seeing similarly successful results so far is a “really important milestone,” he added.
Indeed, it will take more than one company to meet the demand for COVID-19 vaccines. Coronavirus cases passed 11 million in the U.S. over the weekend, with 1 million of them logged in just the last week. More than 247,000 people have died in the U.S., more than in any other single country.
Even if the Food and Drug Administration allows emergency use of both candidate vaccines, supplies will be limited through the end of the year at least. Moderna expects to have 20 million doses for the U.S. market by Dec. 31, while Pfizer and its German partner BioNTech expect to have about 50 million doses for customers around the world by the same time. Both vaccines require that people get two shots several weeks apart.
As long as demand outstrips supply, any COVID-19 vaccine will have to be rationed. While it’s still unclear exactly who will be first in line, Health and Human Services Secretary Alex Azar said the hope was to prioritize adults over 65 (who face the highest risk of serious illness and death) as well as healthcare workers (who face prolonged exposure to the virus).
Dr. Anthony Fauci, the nation’s top infectious disease expert, said it could take until spring or summer for there to be enough supply to allow anyone who wanted a shot to get one.
A few things to keep in mind: The results announced to date are preliminary. The protection rate for either or both vaccine candidates may change as more infections are detected in the study population.
Another big unknown: exactly how long the protection afforded by the vaccines will last.
The side effects of Moderna’s vaccine include fatigue, muscle aches and injection-site pain after the vaccine’s second dose. Hoge said these occurred at rates that were higher than with flu shots but on par with other vaccines, such as the one for shingles. (In case you missed it, our columnist Sandy Banks wrote about a local cancer survivor and his daughter who participated in the Pfizer trial. Though they don’t know whether they got the vaccine or a placebo, they reported symptoms also ranging from aches to chills and exhaustion — a cost they both said was well worth the endeavor.)
Note that both shots are based on a brand-new technology. These so-called mRNA vaccines aren’t made with the coronavirus itself, which means there’s no chance anyone could become infected from the shots. Instead, the vaccine contains a piece of genetic code that trains the immune system to recognize the virus’ telltale spike protein.
By the numbers
California cases and deaths as of 5:03 p.m. PST Monday:
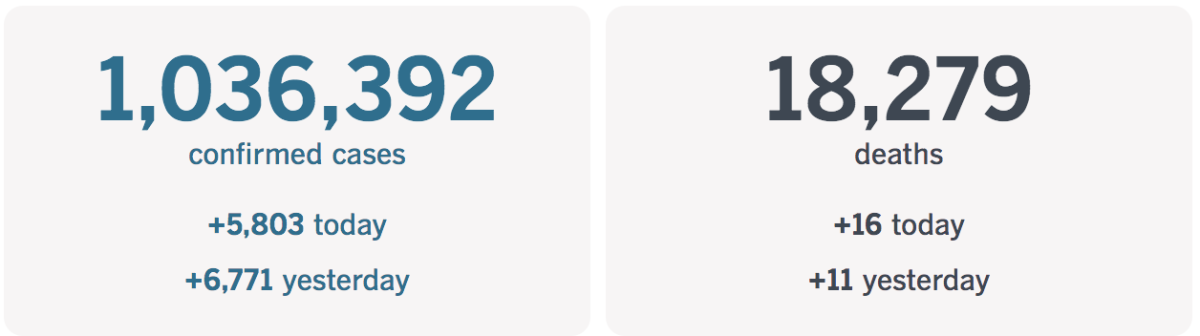
Track the latest numbers and how they break down in California with our graphics.
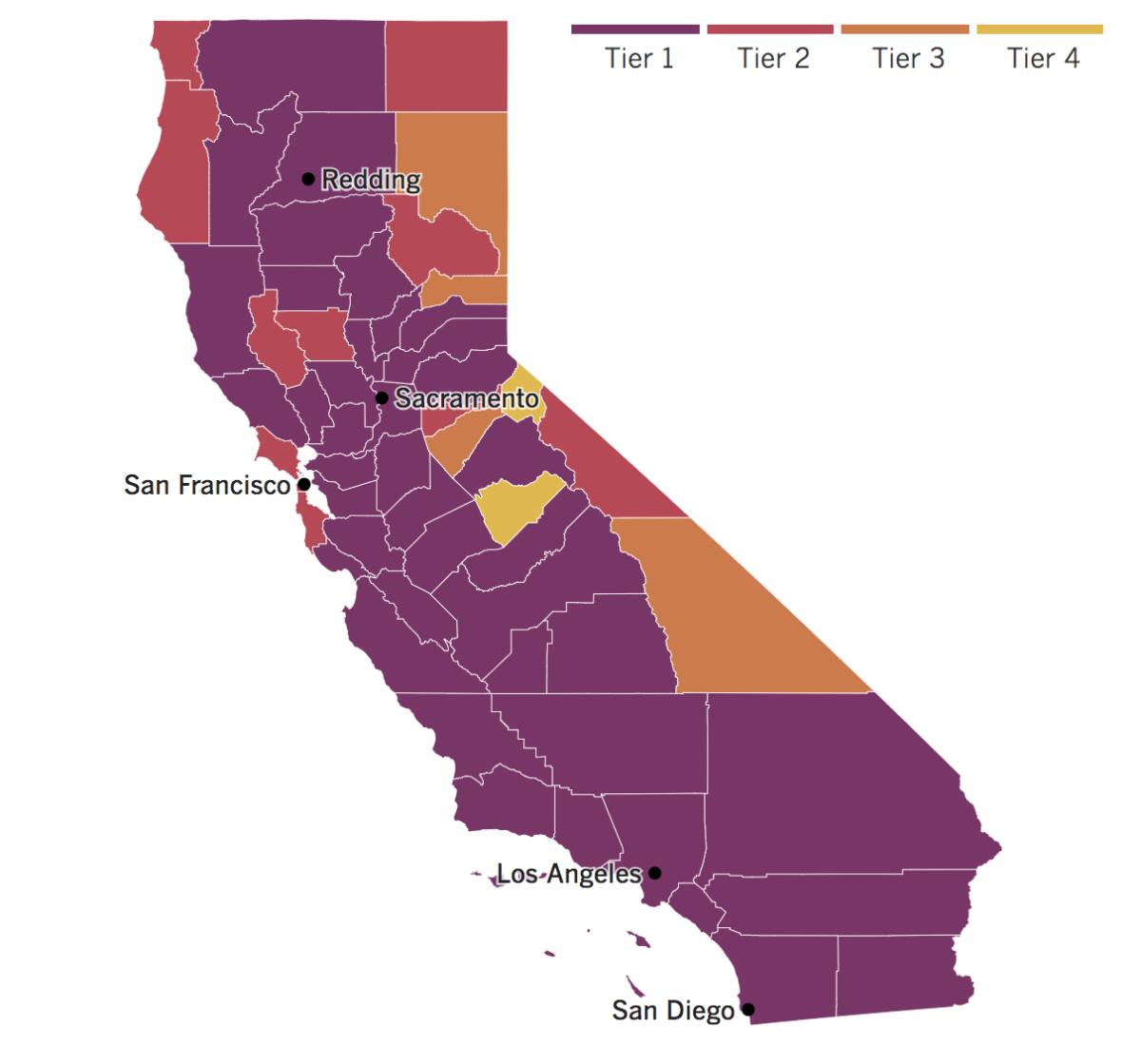
See the current status of California’s reopening, county by county, with our tracker.

Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Across California
California has had a bumpy ride as the state battles a surge in coronavirus cases. Now officials say they’re pulling the equivalent of an emergency brake, announcing that almost all of the state will be placed into the more restrictive tiers of the state’s reopening roadmap.
Once the changes go into effect on Tuesday, roughly 94% of Californians will live in counties in the strictest purple category of the four-tier roadmap. This means that many businesses will have to suspend or severely limit their indoor operations.
There’s a good reason for pulling so much of California into the purple tier, Gov. Gavin Newsom said Monday: It’s facing the steepest rise in COVID-19 cases it has seen. Over the seven-day period ending Sunday, the state averaged 7,985 new cases per day, up nearly 90% from just two weeks ago, according to The Times’ coronavirus tracker.
“We are seeing community spread broadly now throughout the state of California,” Newsom said.
Los Angeles, San Bernardino, Riverside, San Diego and Imperial counties are already in the purple tier. The new additions include Orange, Ventura, Santa Barbara, Kern and San Luis Obispo.
Santa Clara, Alameda, Contra Costa, Napa and Solano joined the Bay Area’s purple contingent, as well as all eight counties in the San Joaquin Valley.
San Francisco, once touted as a major success story in California, is now suffering from a “major surge” of the coronavirus. It will move from the least-restrictive yellow tier for reopening to the state’s second-most restrictive red tier.
San Francisco Mayor London Breed and Public Health Director Dr. Grant Colfax pleaded with residents to avoid travel and gathering outside their households on Thanksgiving. “What we are asking people to do is sacrifice,” Breed said.
Los Angeles County reported more than 3,000 new infections both Saturday and Sunday. Indeed, the 3,780 new cases on Saturday marked the highest one-day total since mid-July.
“When cases are increasing at this pace, it is really important for us to act quickly,” said acting state health officer Dr. Erica Pan. “Every day makes a difference, and time is of the essence.”
More than 1 million Californians have been diagnosed with the coronavirus during the pandemic, and more than 18,200 have died. And things could soon get worse as cooler temperature push people together indoors and the holidays tempt resident to gather with members of other households.
Gov. Newsom issued an advisory recommending that residents avoid unnecessary travel, including for Thanksgiving, and urging those who do head out of state to voluntarily self-quarantine for 14 days when they return. Essential travel is defined as “for work and study, critical infrastructure support, economic services and supply chains, health, immediate medical care and safety and security.”
Carving turkey and trimming trees didn’t make it onto the “essential” list.
If the virus’ rampage continues unabated, it’s unclear what other measures state officials might have to take to get the outbreak under control. Some L.A. County officials have discussed potentially limiting businesses hours or instituting some type of curfew.
“I think it makes sense to do everything we can to encourage people not to be out and about, not to be mingling with others,” said county Public Health Director Barbara Ferrer. “And if we can’t make those choices ourselves, you’re forced to sort of look at, structurally, how do you make it harder for people to intermingle, particularly in activities where we know there’s going to be spread.”
Meanwhile, Gov. Gavin Newsom issued a mea culpa Monday for visiting a Napa Valley restaurant with people from other households. His behavior contradicted the spirit of the same safety guidelines and precautions to which he has asked other Californians to adhere, he said.
“I want to apologize to you because I need to preach and practice, not just preach and not practice,” he said. “We’re all human. We all fall short sometimes.”
The governor acknowledged that the decision to dine with others may lead to a loss of his moral authority. The governor has been criticized recently not just for this faux pas but also for sending his children back to in-person classes at a private school in Sacramento County while millions of other California schoolkids and their families struggle with distance learning.
San Diego Mayor Kevin Faulconer, Newsom’s most prominent GOP critic, condemned the governor in a tweet last week.
“His kids can learn in person. But yours can’t,” Faulconer wrote. “He can celebrate birthday parties. But you can’t. He can dine on a $350 meal at one of California’s fanciest restaurants during the worst recession in generations. But you definitely can’t. Can you believe this? I can’t.”
Resources
— For general safety, wash your hands for at least 20 seconds (here’s a super-fun how-to video). Stop touching your face, and keep your phone clean. Practice social distancing, maintaining a six-foot radius of personal space in public. And wear a mask if you leave home. Here’s how to do it right.
— Watch for symptoms including fever, cough, shortness of breath, chills, repeated shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. If you’re worried you might be infected, call your doctor or urgent care clinic before going there.
— Need a COVID-19 test? Here’s how to receive a free test if you’re in L.A. County. And here’s a map of testing sites across California.
— Here’s how to care for someone with COVID-19, from monitoring their symptoms to preventing the virus’ spread.
— If your job has been affected by the pandemic, here’s how to file for unemployment.
— Here are some free resources for restaurant workers and entertainment industry professionals having trouble making ends meet.
— Advice for helping kids navigate pandemic life includes being honest about uncertainties, acknowledging their feelings and sticking to a routine. Here’s guidance from the CDC.
— In need of mental health services? Here are resources for coping during the crisis from the CDC and the L.A. County Department of Mental Health. L.A. County residents can also call (800) 854-7771 or text “LA” to 741741.
— For domestic violence victims, the pandemic can pose a “worst-case scenario,” advocates say. If you or someone you know is experiencing such abuse, call the National Domestic Violence Hotline at 1-800-799-SAFE (7233) or L.A. County’s hotline at 1-800-978-3600. Here are more ways to get help.
Around the nation and the world
Even as public health experts warn that a dire new chapter in the COVID-19 pandemic is nigh, President-elect Joe Biden’s team remains cut off from the government experts managing the pandemic as President Trump balks at conceding defeat.
Officials say a smooth transition between the incoming and outgoing administrations will be essential as they prepare to distribute a COVID-19 vaccine starting early next year.
“There are people at [the Department of Health and Human Services] making plans to implement that vaccine,” said Biden’s incoming chief of staff, Ron Klain. “Our experts need to talk to those people as soon as possible, so nothing drops in this change of power we’re going to have on Jan. 20.”
Among those key experts is Dr. Anthony Fauci, the nation’s top infectious disease expert. Asked whether it was important to begin working with the incoming administration as soon as possible, Fauci responded: “Yes, of course. … That is obvious.”
Trump, meanwhile, traveled Sunday to his Virginia golf property and reiterated false claims of widespread of election fraud on Twitter.
North Dakota nurses trying to save COVID-19 patients without becoming sick themselves now have another worry: catching the virus from their infected but asymptomatic colleagues.
Gov. Doug Burgum has allowed the state’s embattled hospitals to use infected but asymptomatic workers to treat COVID-19 patients. The move reflects the scarcity of medical workers in a state that has been regularly breaking its records for both cases and deaths.
Burgum said his decision could help the state’s short-staffed hospitals deal with the surge, and the move has been praised by some hospital administrators. But many nurses say the governor is saddling them with yet another burden while failing to impose common safeguards that, while less politically palatable in the conservative state, would help prevent the virus from spreading.
One of those nurses is Adam Johnston. He works in an emergency room and has watched people die on every shift. He‘s been able to find solace during brief breaks with fellow nurses. Now, even those moments of relief are a threat to his health.
“It’s going to make you question every time you want to sit down and grab a five-minute snack with one of your co-workers,” said Johnston, who is the president of the state’s Emergency Nurses Assn. “You’re always going to think, ‘Am I six feet away from them? Am I safe? Am I not?’”
The World Health Organization, tasked with coordinating the international response to the COVID-19 pandemic, has logged 65 coronavirus cases among staff based at its headquarters — in spite of its public assertions that there has been no transmission at the site, according to an internal email.
The news comes as cases surge in Europe, including in Switzerland and particularly in Geneva, the WHO’s home base. According to the email, about half of the infections were in people who had been working from home, but 32 were detected in staffers who had been working at the main office. This suggests the United Nations health agency’s strict hygiene, screening and other prevention measures were not enough to protect it from the pandemic’s reach.
Your questions answered
Today’s question comes from a reader who wants to know: How many infectious people are missed by our current methods of screening, such as temperature checks and health questionnaires?
This question comes from a Colorado man who points out that many symptoms on a COVID-19 questionnaire are the kinds of symptoms he has daily, being of “Medicare age.”
We just published a story on some research that helps answer this question. A study of Marine Corps recruits found that temperature and symptom checks, like those used at schools and in doctors’ offices, are not great at spotting coronavirus infections and preventing outbreaks.
The New England Journal of Medicine study involved 1,848 Marine recruits, 90% of them men, who were told to self-isolate for two weeks at home. This was followed by supervised military quarantine for two more weeks at a closed college campus where the recruits had a single roommate, wore masks, kept at least six feet apart and held most of their training outdoors. And of course, they had daily fever and symptom checks.
Recruits were tested when they arrived for the military quarantine, and tested again seven and 14 days later. Sixteen (about 1%) of the recruits tested positive on arrival, though only one of them had any symptoms. An additional 35 recruits (about 2%) of the recruits tested positive during the two-week military quarantine, though only four of them had symptoms.
Genetic testing showed that there were six separate clusters of cases among the recruits.
That’s in spite of the fact that these quarantine measures — and the adherence to them — were far more strict than at a typical college campus, said Dr. Stuart Sealfon of the Icahn School of Medicine at Mount Sinai in New York, one of the study’s leaders.
The findings have implications for colleges, prisons, meatpacking plants and other places that rely on this kind of screening.
The case shows that “young, healthy persons can contribute to community spread of infection, often silently,” Dr. Nelson Michael of the Walter Reed Army Institute of Research wrote in a commentary that accompanied the paper.
Michael said the results suggest that current quarantine periods might have to be longer than two weeks. “An extended quarantine may prevent further transmission once recruits enter a prolonged training period on base, where physical distancing is far more difficult to reconcile with the need to train combat infantry,” he wrote.
So, returning to the reader’s question, it seems your hunch is correct: Our screening methods do miss a lot of infections and aren’t great at preventing outbreaks.
Our reporters covering the coronavirus outbreak want to hear from you. Email us your questions, and we’ll do our best to answer them. You can find more answers in our Frequently Asked Questions roundup and in our reopening tracker.
For the most up-to-date coronavirus coverage from The Times over the weekend, visit our homepage and our Health section, sign up for our breaking news alerts, and follow us on Twitter and on Instagram.




