Coronavirus Today: Why exactly are cases surging?
- Share via
Good evening. I’m Amina Khan, and it’s Thursday, Nov. 19. Here’s what’s happening with the coronavirus in California and beyond.
As officials in Los Angeles fight to get the coronavirus outbreak under control, they’re struggling to understand why so many people are becoming infected.
The county is worse off now than it has ever been during the COVID-19 pandemic, with more than 348,500 coronavirus infections confirmed to date and more than 7,300 deaths, according to Times data.
In early October, L.A. County recorded its lowest number of cases since the spring, after months of restrictions that prohibited Angelenos from exercising inside gyms, watching movies in theaters and dining indoors at restaurants.
Here’s the thing: All of those same restrictions are still in place.
So what changed?
It’s not the virus. The rules are essentially the same. Folks who were interviewed after testing positive for the virus haven’t revealed any major shifts in behavior compared with a month ago, such as dining out more often or making more trips to the store, said Dr. Jeffrey Gunzenhauser, L.A. County’s chief medical officer.
The answer is out there, but health officials can’t find it because they’re facing challenges in contact tracing.
Contact tracing is basically exactly what it sounds like. Officials interview an infected person to find out whom they’ve been in contact with, then test those people and trace their contacts, and so on. If done right, it can nip an outbreak in the bud. It also allows investigators to track the train of transmission back toward its source.
It’s a tried-and-true method, but since so many people are currently infected, it’s nearly impossible to pinpoint exactly how someone contracted the virus.
“Contact tracing just can’t keep up with it,” said Kevin Malotte, a Cal State Long Beach professor emeritus of epidemiology. “You have to make kind of educated guesses as to what you think is going on.”
In L.A. County, officials say they don’t know where a majority of infected people contracted the virus. A similar trend holds nationally.
Another stumbling block in the process: Some infected people refuse to talk to contact tracers. Only about 63% of people contacted by the county public health department complete the interview. Officials have started offering $20 gift cards to people who agree to participate.
Without a fuller picture from contact tracing, it’s hard to understand Los Angeles’ turn for the worse. Still, several trends explain part of the jump, if not all of it.
It’s possible that the coronavirus somehow became more prevalent in the community in the last several weeks, perhaps because of the slight uptick in gatherings or because colder weather prompted people to spend more time indoors, Gunzenhauser said. Other experts suggested that the earlier sunsets have sent more people indoors, or that visitors from parts of the country where COVID-19 is surging have brought the virus with them.
As more people fall sick, every interaction becomes more dangerous.
“All it takes is a slight change in some behavior or practice, and the virus is going to take advantage of that,” Gunzenhauser said. “Interactions that at the end of August would not have led to an infection now are, because we have quite a few more people infected.”
By the numbers
California cases and deaths as of 4:05 p.m. PST Thursday:
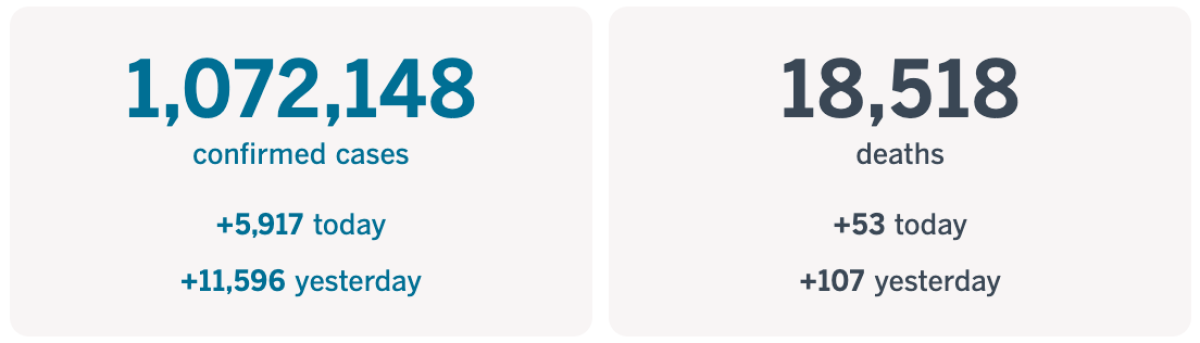
Track the latest numbers and how they break down in California with our graphics.
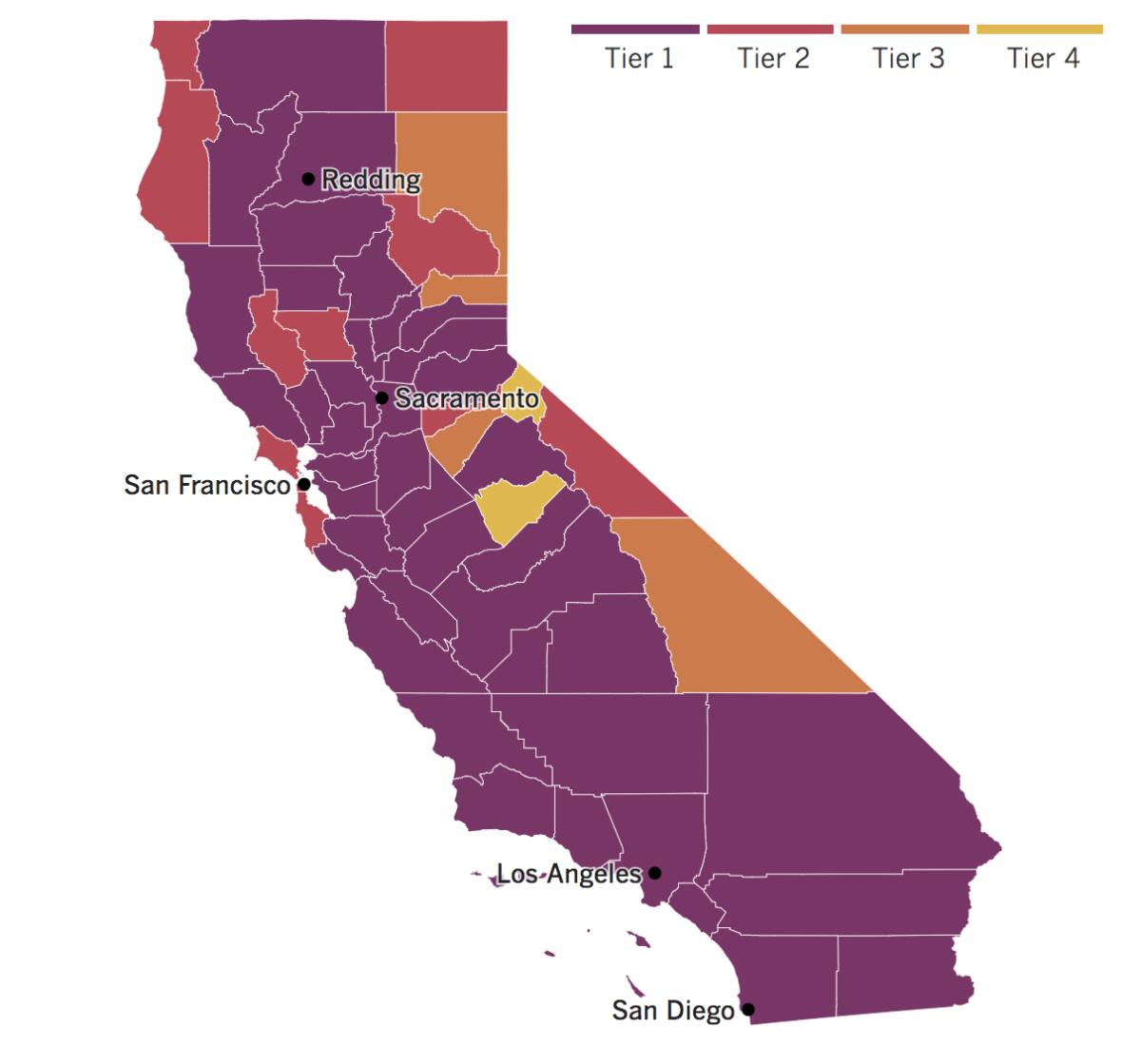
See the current status of California’s reopening, county by county, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Across California
Gov. Gavin Newsom has upped the ante in California’s fight against the coronavirus with a curfew for most of the state. The mandatory overnight stay-at-home order goes into effect on Saturday and will last through Dec. 21, though it could be extended beyond that.
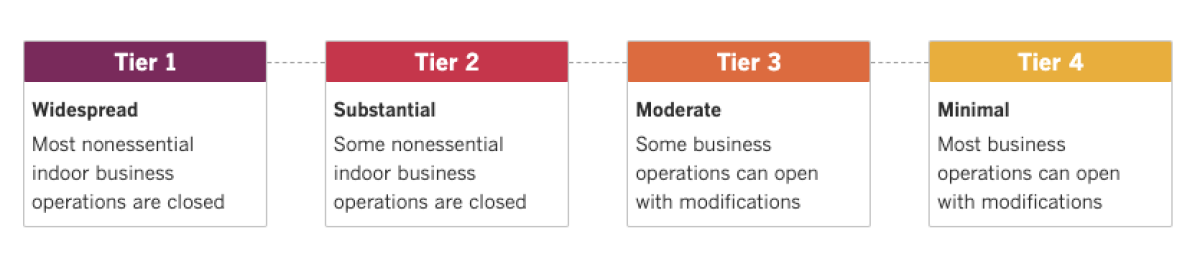
The order, issued by the state’s public health department, will prohibit most nonessential activity outside the home from 10 p.m. to 5 a.m. in counties in the strictest, or purple, tier in the state’s four-tier reopening road map. About 94% of Californians, or 37 million people, live in counties in the purple tier.
“The virus is spreading at a pace we haven’t seen since the start of this pandemic, and the next several days and weeks will be critical to stop the surge. We are sounding the alarm,” Newsom said in a statement released Thursday afternoon. “It is crucial that we act to decrease transmission and slow hospitalizations before the death count surges. We’ve done it before, and we must do it again.”
There’s clear reason for officials to be alarmed: California has reported more than 10,000 new daily cases four times in the past week. That’s something the state had never before experienced — even during the summer, its deadliest time of the pandemic.
“We are asking Californians to change their personal behaviors to stop the surge,” said Dr. Erica Pan, the state’s acting public health officer. “Letting our guard down could put thousands of lives in danger and cripple our healthcare system,” she said.
In another sign that things are getting worse, Los Angeles County reported more than 5,000 new coronavirus cases Thursday — the most the county has seen on any single day since the start of the pandemic. While the case count is concerning enough, officials say the bigger worry is that a surge in new infections tends to lead to a hike in hospitalizations.
County health officials warn that hospitals and their intensive care units are at risk of being overwhelmed if cases keep rising. The number of people hospitalized with COVID-19 in the county has shot up by more than 70% over the past month, from 722 on Oct. 17 to 1,238 on Tuesday.
Unless things change quickly, “demand for ICUs will outstrip the supply of beds, and hospitals will have to take drastic action to be able to meet the needs of those who require an ICU level of care,” said Dr. Christina Ghaly, the county’s director of health services.
This could have consequences far beyond COVID-19 patients, said Barbara Ferrer, L.A. County’s public health director.
“For all of you out there that may be in a car accident or you may have a heart attack or you may, unfortunately, have a stroke or have a serious asthma attack, when the hospital system is overwhelmed, care for everyone gets seriously compromised,” she said. “So we owe it to each other, we owe it to our healthcare workers most importantly, to not keep transmitting this infection.”
In response to the surge, the San Bernardino school system said it will not reopen its campuses for the rest of the school year. The school district, with about 47,000 students, may be the first in the state to make that hard call.
In an online announcement, the district said the action was taken “after carefully weighing local COVID-19 figures that show the virus is spreading at alarming rates and families living in its attendance boundaries are especially at risk.” The infection rate within the school district’s boundaries is among the highest in the county.
About 9 in 10 students are from low-income families that have often had a harder time supervising and supporting children with the challenges of all-online school. Families in low-income areas also have been among the last to receive the necessary tech gear for distance learning.
The district’s decision highlights the disparity between school systems serving more affluent communities with lower virus transmission rates, and those serving low-income neighborhoods that tend to have higher coronavirus rates, my colleague Howard Blume writes.
Resources
— For general safety, wash your hands for at least 20 seconds (here’s a super-fun how-to video). Stop touching your face, and keep your phone clean. Practice social distancing, maintaining a six-foot radius of personal space in public. And wear a mask if you leave home. Here’s how to do it right.
— Watch for symptoms including fever, cough, shortness of breath, chills, repeated shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. If you’re worried you might be infected, call your doctor or urgent care clinic before going there.
— Need a COVID-19 test? Here’s how to receive a free test if you’re in L.A. County. And here’s a map of testing sites across California.
— Here’s how to care for someone with COVID-19, from monitoring their symptoms to preventing the virus’ spread.
— If your job has been affected by the pandemic, here’s how to file for unemployment.
— Here are some free resources for restaurant workers and entertainment industry professionals having trouble making ends meet.
— Advice for helping kids navigate pandemic life includes being honest about uncertainties, acknowledging their feelings and sticking to a routine. Here’s guidance from the CDC.
— In need of mental health services? Here are resources for coping during the crisis from the CDC and the L.A. County Department of Mental Health. L.A. County residents can also call (800) 854-7771 or text “LA” to 741741.
— For domestic violence victims, the pandemic can pose a “worst-case scenario,” advocates say. If you or someone you know is experiencing such abuse, call the National Domestic Violence Hotline at 1-800-799-SAFE (7233) or L.A. County’s hotline at 1-800-978-3600. Here are more ways to get help.
Around the nation and the world
Long lines for coronavirus testing are getting longer around the U.S. as families hope to gather safely for Thanksgiving in the midst of a major surge in cases.
Thousands have lined up outside Dodger Stadium for drive-through testing. Across New York, people have waited for three hours or more in lines spanning multiple city blocks.
The delays are growing as Americans prepare for winter weather, flu season and holiday travel — a dangerous mix that experts say will further fuel an outbreak that has already resulted in more than 11.5 million cases and more than 250,000 deaths.
Continuing shortages in key lab supplies may create more bottlenecks that will be worsened by the pre-holiday rush.
There is a glass-half-full point here: The fact that shortage problems are only now emerging more than a month into the latest surge is a credit to the country’s increased testing capacity. More than 1.5 million people are being tested each day, on average, more than double the number in July.
But experts say the U.S. is still far short of what’s needed to control the spread of the virus. Many have called for anywhere between 4 million and 15 million daily tests in order to halt its spread.
Another COVID-19 vaccine may soon be joining the fray. Oxford University scientists expect results from late-stage trials on their vaccine candidate to be available by Christmas, said a key researcher, who added that the shot appears to be well tolerated and produces a strong immune response in older patients.
“The reason that we’re so delighted is that we’re seeing the immune responses look exactly the same, even in those who are over 70 years of age,” said Dr. Andrew Pollard, an expert in pediatric infection and immunity at Oxford.
The vaccine is being developed with drug maker AstraZeneca. Two other vaccine candidates from Pfizer and Moderna appear to be around 95% effective, according to preliminary results reported this week.
In Denmark, Prime Minister Mette Frederiksen has replaced the minister of agriculture, Mogens Jensen, who resigned after the government ordered that all mink be culled amid fears of coronavirus transmission.
The kill order came after it was found that a mutated version of the virus in Danish minks can be transmitted to people — though there is no evidence so far that it is more dangerous or more resistant to vaccines. Authorities say 11 people were sickened by this version of the virus earlier this month.
The problem was that the government lacked a legal basis for killing healthy animals. That oversight caused it to rush to build consensus for a new law that now has the backing of a majority in the Danish parliament.
Your questions answered
Today’s question comes from a reader who wants to know: Should we mask up when we come into contact with people who have recovered from COVID-19?
This reader was curious about British Prime Minister Boris Johnson’s decision to quarantine after learning that he had come into contact with someone infected with the virus. Johnson has already recovered from a case of COVID-19 — so shouldn’t he have some immune protection?
The short answer is: You should definitely still wear a mask, says Dr. Stuart Ray, an infectious disease specialist at the Johns Hopkins University School of Medicine.
First off, two things to know: Scientists think about half of coronavirus transmission happens through asymptomatic spread, by people who show no signs of the disease. Second: People who have already survived COVID-19 can potentially be reinfected with the virus if they’re exposed to a different strain from the one that first made them sick.
Those cases are relatively rare, Ray said. However, that may be because these cases are potentially underreported.
“The challenge is that to report a reinfection is a very high bar,” Ray explained.
The initial infection has to be tested and positively identified. The virus sample needs to be genetically sequenced. Once they’re experiencing symptoms again, the patient has to test positive a second time, and a new sample needs to be sequenced to determine whether the virus is the same as the first (and thus possibly due to an old, persistent infection) or if it’s different (and thus due to reinfection with a new strain of the virus).
“They have to be shown to be different,” Ray said.
So yes, if you are near someone who has previously survived COVID-19, you can’t assume they are immune to reinfection, and you both should definitely wear masks. Conversely, since they could potentially have a second infection, you should both wear masks.
Bottom line: Wear masks, everybody. There’s no free pass to unmask.
Our reporters covering the coronavirus outbreak want to hear from you. Email us your questions, and we’ll do our best to answer them. You can find more answers in our Frequently Asked Questions roundup and in our reopening tracker.
For the most up-to-date coronavirus coverage from The Times over the weekend, visit our homepage and our Health section, sign up for our breaking news alerts, and follow us on Twitter and on Instagram.
Updates
2:08 p.m. Jan. 20, 2021: In the “Your Questions Answered” portion of this newsletter, we may have implied that a person who recovered from COVID-19 could be sickened again only if they’re exposed to a different coronavirus strain. While that can happen, people can also be reinfected by the exact same strain — though because of testing limitations, it’s impossible to say how often this takes place. Want to learn more? Check out the reader question in this edition of Coronavirus Today.




