Coronavirus Today: What’s an ‘acceptable’ number of deaths?
- Share via
Good evening. I’m Karen Kaplan, and it’s Tuesday, April 5. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Let’s face it: We’ll probably never see a time when the annual number of COVID-19 deaths in the U.S. falls to zero. That seems like a fact we can live with.
But how much higher than zero should that number be?
The answer matters, because it will determine how soon we can leave behind mask mandates, vaccination requirements, restrictions on large gatherings and other rules designed to hinder coronavirus spread.
The higher the number, the sooner we can transition into a post-pandemic world. The lower the number, the longer we’ll have to wait.
I’m sure you’re eager to get back to “normal.” We all are. But you might be a little uncomfortable with the idea that the price for doing so now instead of next month — or at summer’s end, or a year from now — will be someone’s life. Many someones.
Will it be the neighbor you see walking his dog every morning? Your co-worker’s mom? The person who cuts your hair?
Will it be your spouse? Will it be you?
This is the kind of morbid calculation public health professionals make as they weigh the costs and benefits of saving lives. They have a label for the ones that won’t make it: “acceptable deaths.”
For instance, 34.2 million American adults continue to smoke in spite of minimum age requirements to buy cigarettes, laws against smoking in public, and public health campaigns to help people quit. The nation’s 480,000 tobacco-related deaths each year are “acceptable” — neither the government nor the public is willing to spend more money or tolerate more intrusive regulations to bring the number down.
Likewise, more than 100,000 Americans die of diabetes each year, but attempts to reduce that number by putting limits on the sale and consumption of sugary drinks have met with fierce political resistance. Apparently, that amount of deaths is “acceptable” too.

Those who are willing to drop all pandemic safety measures tomorrow and simply live with the coronavirus are making an implicit decision that the current death rate is acceptable.
And just what is that death rate? Over the last week of March, COVID-19 claimed an average of 749 lives in the U.S. each day, my colleague Melissa Healy reports. That’s far fewer than the roughly 1,900 who die of heart disease and the 1,650 who die of cancer on a daily basis, but it’s more than five times the 147 lives lost to influenza and pneumonia combined.
(You see, LeBron? Kareem is right: COVID-19 is not the same as a cold or the flu.)
Officials at the Centers for Disease Control and Prevention and other federal agencies haven’t come up with an amount of acceptable deaths for COVID-19. They’re still deciding on the criteria they’ll use to determine when it will be safe to consider the pandemic over, at least in the U.S.
But other health experts have taken a stab at picking a number. They suggest an acceptable yearly death toll from all respiratory illnesses — including COVID-19 — is 60,225.
That works out to an average of 165 deaths per day nationwide. It’s about the same as an extremely severe flu season in the days before COVID-19.
“There was no magic to it at all,” said Michael Osterholm, the director of the University of Minnesota’s Center for Infectious Disease Research and Policy and one of 23 experts who wrote a report that included the number. “Our goal was to say that at these numbers and below, you’re much less likely to be stressing the healthcare system.”
That’s important because if the healthcare system is stressed, the quality of hospital care suffers and patients with all kinds of diseases — not just COVID-19 — will suffer.
By the numbers
California cases and deaths as of 4:30 p.m. on Tuesday:
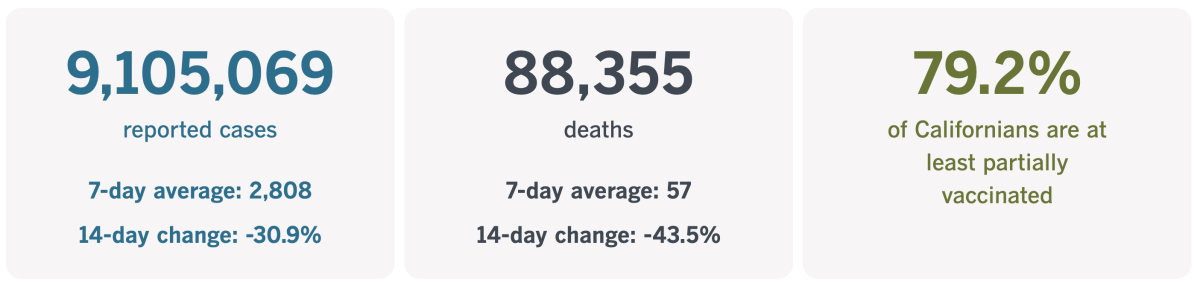
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Were all the rules worth it?
The United States is on the verge of notching its 1 millionth COVID-19 death. No other country is anywhere close. Brazil, which ranks second in total deaths, has recorded a little more than 660,000 pandemic fatalities.
The U.S. is faring better on a per-capita basis — our 299 deaths per 100,000 people over the course of the pandemic are lower than those of 18 other countries, according to Johns Hopkins University.
Still, the fact that the richest country in the world has suffered so many casualties might make you wonder if all our pandemic restrictions did us much good. Would things really have been much worse without the stay-at-home orders, travel bans, school shutdowns and other measures that turned our lives upside down?
In all likelihood, the answer is yes.
We can say this because there’s another way to approach this alternative-universe thought experiment: Would the U.S. have been better off if we’d acted more like Sweden?
The Scandinavian country took a decidedly different approach to confronting the coronavirus. For much of the pandemic, it eschewed lockdowns, paid little mind to social distancing, and kept restaurants, bars and schools open.
It was as if Sweden were conducting a giant experiment to test the validity of the Great Barrington Declaration, the much-criticized white paper that advocated the pursuit of herd immunity without waiting for vaccines to be developed first. This was supposed to be done by protecting the most vulnerable members of the community while allowing the virus to spread more or less freely among everyone else. (It’s kind of like hosting a chicken pox party on a national scale, except the disease in question is COVID-19, not varicella.)
It turns out that didn’t work so well, my colleague Michael Hiltzik writes. In fact, according to a new study in the journal Nature, it was a disaster.
“The Swedish response to this pandemic,” the researchers report, “was unique and characterized by a morally, ethically, and scientifically questionable laissez-faire approach.”

The Swedish government never stated publicly that herd immunity was its goal, but they did so in private emails obtained by investigative reporters.
The plan was to have children catch and spread the coronavirus, the study authors wrote in Nature. But when vulnerable people like senior citizens and those with chronic health problems became sick, care for them was denied.
In Stockholm, for instance, doctors were instructed not to give ICU rooms to people with preexisting health conditions because they were “unlikely to recover,” the researchers wrote. The triage rules also put seniors at a disadvantage.
That wasn’t the only hurdle they faced.
“Many elderly people were administered morphine instead of oxygen despite available supplies, effectively ending their lives,” the researchers wrote. “Potentially life-saving treatment was withheld without medical examination, and without informing the patient or his/her family or asking permission.”
You might be wondering how Sweden’s public health experts came up with this plan. The answer is, they didn’t. It was created by “a small, insular group of government officials who not only failed to consult with experts in public health, but ridiculed expert opinion,” Hiltzik writes.
When scientists learned things about the coronavirus that called the government’s strategy into question, they didn’t adapt. Instead, they ignored or downplayed whatever was inconvenient.
Despite doubling down on their herd immunity plan, Sweden fell short. By a lot.
“Projected ‘natural herd-immunity’ levels are still nowhere in sight,” the researchers wrote in Nature.
And it probably never will be, they added: Herd immunity “does not seem within reach without widespread vaccinations,” and it “may be unlikely” under any circumstances.
OK, so that part of the plan didn’t work. But did Sweden at least soften the pandemic’s economic blow by keeping the economy relatively open?
Not really. An analysis by the Organization for Economic Cooperation and Development found that while Sweden fared a little better than the European average, it was far behind its Scandinavian sister countries of Denmark, Norway and Finland. The pandemic “hit the economy hard,” the OECD analysis said.
Sweden’s cumulative COVID-19 death rate is also worse than those of its neighbors. Since February 2020, Sweden has recorded 179 deaths per 100,000 residents, according to the Johns Hopkins tracker. That compares with 100 deaths per 100,000 residents in Denmark, 47 in Norway and 59 in Finland.
Here’s another way to look at it, Hiltzik writes: If Sweden’s death rate were as low as Norway’s, the country would have had 4,429 COVID-19 deaths. In reality, it’s had more than 18,500.
Perhaps Sweden’s King Carl XVI Gustaf summed things up best: “I think we have failed.”
California’s vaccination progress
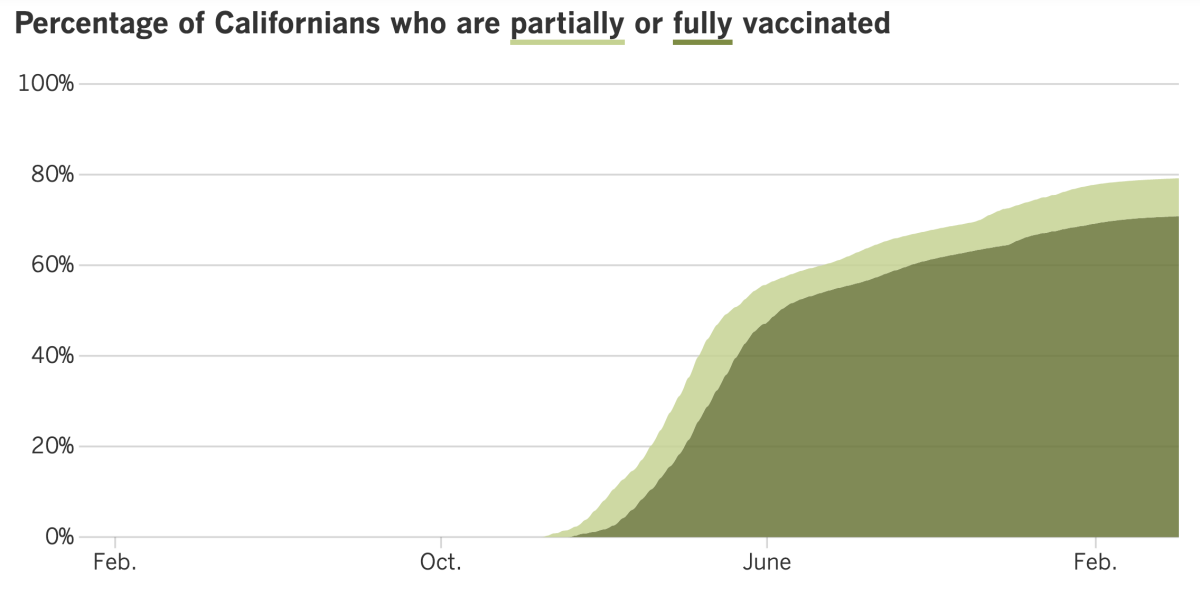
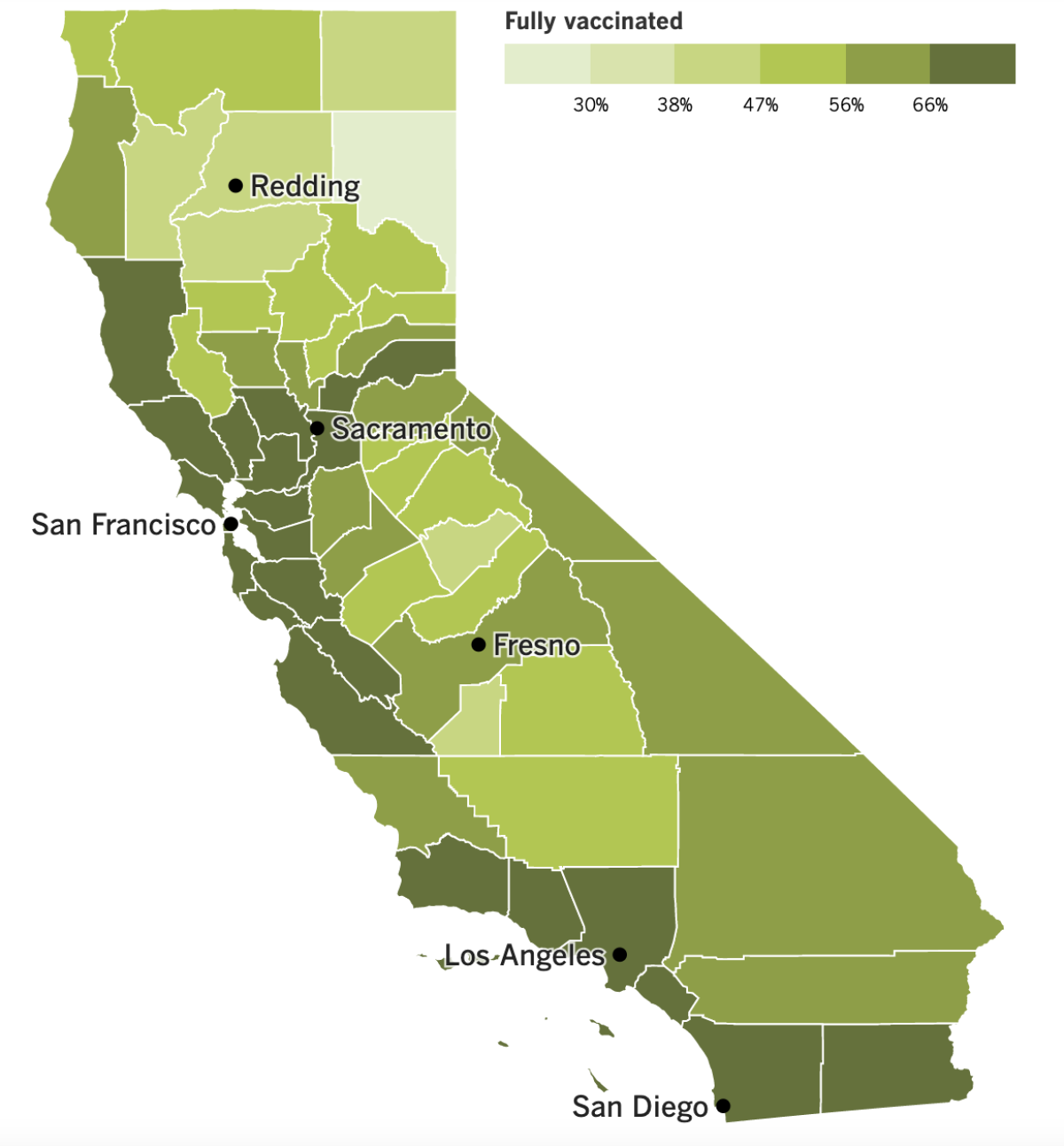
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
California has lost more than 88,000 people to COVID-19. And according to new data from the U.S. Census Bureau, the Golden State lost an additional 260,000 or so residents between July 1, 2020, and July 1, 2021, because they opted to move away.
The bulk of that population decline occurred in Los Angeles County, which is still home to more people than any other in the country. About 160,000 Angelenos packed up and left during that 12-month period, reducing the population by about 1.5%.
San Francisco lost about 54,000 residents, but since it’s smaller than L.A., that amounted to a 6.7% population decline — the second-highest loss in the nation. Only Manhattan (a.k.a. New York County) fared worse, losing 6.9% of its residents.
Most of the former Californians left the state by choice. With the pandemic enabling (if not requiring) many people to work remotely, relocating became a possibility that hadn’t been on the table before.
Meanwhile, California’s dramatic decline in coronavirus cases has plateaued as the BA.2 Omicron subvariant made itself more at home. But unlike in New York and Massachusetts, where a BA.2 wave may be in the offing, case numbers here are flat.
Health officials don’t know whether our relatively good fortune will hold, or whether we’ll inevitably follow in the footsteps of those East Coast states. (If we’re really unfortunate, we could wind up like Britain, where an estimated 4.9 million people became infected in the week ending March 26.) There’s hope that the state’s gigantic wave of cases this winter, especially in Southern California and the Central Valley, could ward off a BA.2 surge.
L.A. County Public Health Director Barbara Ferrer said the flattening of cases here was both a good and a not-as-good sign.
“At some point, we knew that it was likely we were going to stop declining because we know that there’s still transmission,” she said. “Personally, I wish we were at a lower level when we’re doing this plateauing, but we have seen a significant decrease, and that is the good news.”
Ferrer added that the best way to keep case numbers moving in the right direction is for people to get up to date on their vaccinations and continue with precautions such as wearing masks in indoor public settings.
Apparently, many Californians agree. In a survey conducted in mid-March by the Public Policy Institute of California, 57% of respondents said they were in favor of requiring proof of vaccination to enter restaurants, bars and gyms. On the flip side, 41% of respondents said they’d rather drop such requirements.
Support for vaccine verification was strongest in the San Francisco Bay Area (where 68% backed it) and in Los Angeles County (where 60% were in favor). A more tepid 55% of Central Valley residents said they endorsed the rule; elsewhere, opinion was pretty evenly split.
Here’s another measure of support: More than 100 employees of the video game studio Activision Blizzard participated in a virtual walkout Monday to protest the company’s lifting of vaccine requirements while urging workers to return to the office.
The Santa Monica-based studio said last week that it would no longer require employees to be fully vaccinated to come into the office. Companies such as Adidas, Starbucks, Intel and United Airlines made similar moves in recent months. Still, the announcement “came as a shock to everybody,” said Ada-Claire Cripps, a senior software engineer at Blizzard whose spouse is in an at-risk category for a serious case of COVID-19.
“I don’t want to have to go into a workplace where I don’t know who I can trust to not get me sick,” she said.
A spokesperson for Activision Blizzard said a majority of employees were operating under a voluntary return-to-office policy and denied that the company would force people to come back if they didn’t want to.
On to Washington, D.C., where administrators of the nation’s Medicare program announced that millions of its enrollees will finally be able to get free over-the-counter coronavirus tests at certain drugstores. The 59 million Americans who have Medicare’s Part B outpatient coverage will be eligible for up to eight at-home tests per month — enough to test themselves twice a week.
Private health insurers have been covering the cost of at-home tests since early January, as have Medicaid and Children’s Health Insurance Program plans. It took a few months to get around rules and regulations that prevented Medicare from following suit.
And there’s more good news: A bipartisan group of senators has agreed on a $10-billion package for continuing the nation’s fight against COVID-19 with vaccines, treatments and other steps. The compromise is more slimmed down than the $22.5-billion measure President Biden initially pushed for, but he was quick to support it.
Although the coronavirus has no respect for international borders — the Delta variant was first spotted in India, Omicron is thought to have emerged in South Africa, and the earliest specimen of the BA.2 subvariant uploaded to a global database came from the Philippines — the package contains none of the $5 billion Biden requested to help other countries fight the pandemic.
And finally, a 60-year-old man in Germany is under investigation for getting as many as 90 doses of COVID-19 vaccine. Police don’t think he’s a hypochondriac. Rather, he’s suspected of forging vaccination cards and selling them to people who want easy access to public venues such as theaters and swimming pools without having to get the shot.
The man was detained when he showed up at a vaccination center in Saxony two days in a row with several blank vaccination cards in his possession, police said.
The doses he received included multiple brands of vaccines. Time will tell what effect all those shots have on his health.
Your questions answered
Today’s question comes from readers who want to know: Should I get a second COVID-19 booster shot if I’m not immunocompromised?
If you’re at least 50 years old, you’ve probably been wondering about this since the CDC and the Food and Drug Administration made a second booster shot available to you last week. Unfortunately, they did so without first consulting their scientific advisory groups to hash out the pros and cons of a second booster. Nor did they actually recommend the shot; they merely made it available.
What makes the decision hard is not that a second booster doesn’t work. It’s that the first booster worked quite well.
A study from Israel examined data from healthcare workers of all ages. Some of them opted for a second booster shot, and some of them stopped after one. The doctors and nurses who got a second booster were 11% to 30% less likely to become infected during the Omicron wave, and they were 31% to 43% less likely to develop COVID-19 symptoms. (The lower figures were for people who got Moderna’s SpikeVax shot for their second booster, and the higher ones were for people who got Comirnaty, the Pfizer-BioNTech vaccine.) Regardless, those who got sick reported “negligible symptoms,” so the net benefit of the extra shot was tiny.
Another study in Israel focused on people 60 and up. The preliminary data suggest that the second booster reduced the risk of a coronavirus infection by as much as 64%, though the protection waned in a matter of weeks. The data also suggest that the second booster reduced the risk of a severe case of COVID-19 by 73%. That held up throughout the nine-week study period. But considering that severe COVID-19 was rare in both groups, people fared well whether they had one booster shot or two.
Melissa Healy spoke to several infectious-disease experts about the merits of a second shot. Dr. Paul Offit at Children’s Hospital of Philadelphia gave the most straightforward advice: Most people 50 and up don’t need a second booster shot, and it doesn’t make sense for them to get it.
But several others believed that however small the upside of a second booster, the downside was even smaller. That’s why Dr. Otto Yang, associate chief of infectious diseases at UCLA, said his default position is that “anyone that’s qualified should just go ahead and get it.”
Here’s another thing to consider: Mixing and matching your vaccine doses may “enhance” your body’s immune response, according to the National Institutes of Health. So if you’ve had three shots of Spikevax, you may want to get a second booster just to get some Comirnaty into your system, or vice versa.
We love that you take this newsletter to heart, but remember that we’re journalists, not doctors. If you’re still on the fence, talk to your physician about your individual situation to help you make up your mind.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

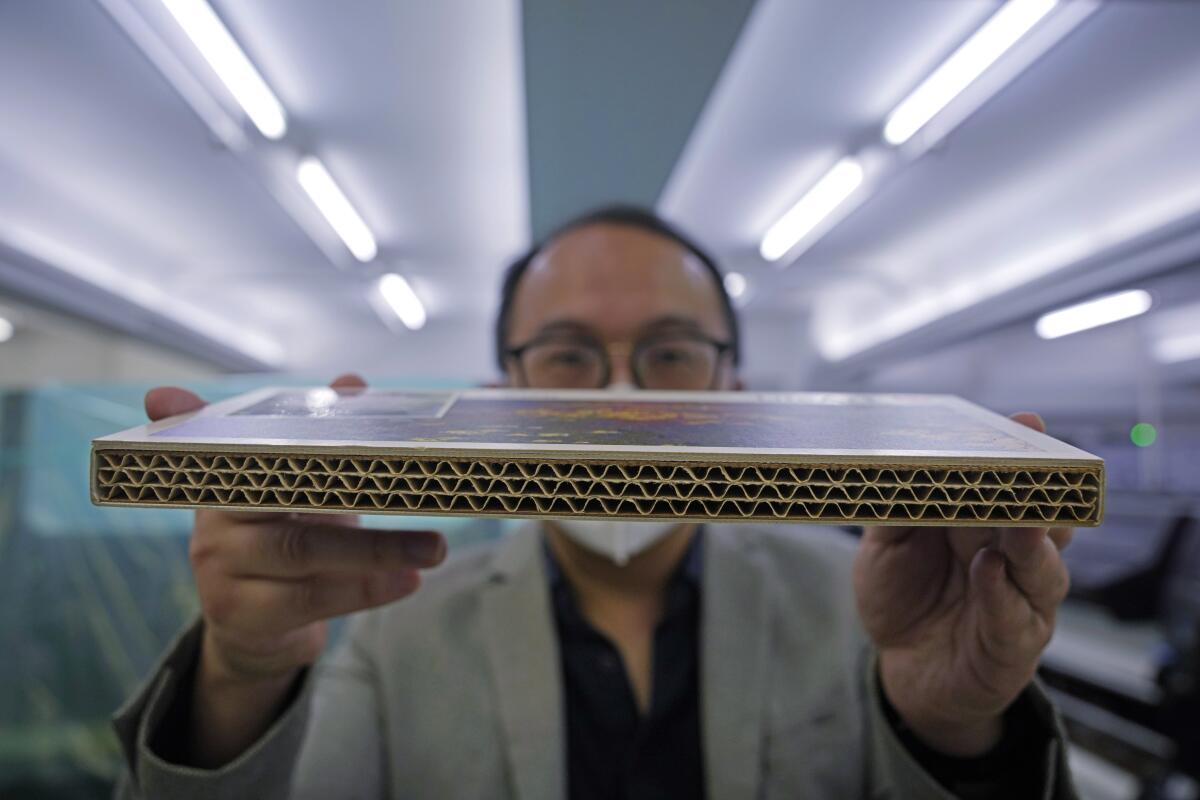
Amid Hong Kong’s devastating COVID-19 outbreak, the number of virus victims exceeds the number of coffins available to contain them. A company called LifeArt says it has a fix: coffins made out of cardboard.
Cardboard coffins — like the one seen above — have several advantages, the company says. They’re environmentally friendly because they’re made of recycled wood fiber and, when burned during cremation, emit far less less greenhouse gas than traditional coffins made of wood or wood substitutes. They’re also customizable, with exteriors that reflect a person’s religion, hobbies or favorite color.
The result is “a more pleasant farewell,” said Chief Executive Wilson Tong, the man holding a cardboard sample in the photo below.
He’s not the only one who thinks so. Albert Ko is a board director at a nonprofit called Forget Thee Not, which advises people about funerals. The group has purchased 300 cardboard coffins to give to people in need or donate to hospitals.
Some of Forget Thee Not’s elderly clients are intrigued by the new option, Ko said with satisfaction: “We hope to take this opportunity to contribute as well as promote eco-coffins.”
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




