Coronavirus Today: America’s pandemic priorities
- Share via
Good evening. I’m Karen Kaplan, and it’s Tuesday, July 19. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Coronavirus cases are on the upswing yet again, and infections are so widespread that nearly 90% of Californians now live in a county with a high COVID-19 community level. Scientists using animals to model the progression of the outbreak estimate that it’ll take until at least 2024 for the disease to become endemic.
Against this backdrop, it’s easy to feel like we’re not making much progress with getting the pandemic under control. Maybe that’s because Americans don’t even agree on what the problem is.
A report out this month from the Pew Research Center shows that Democrats and Republicans have very different views about what the country should prioritize when it comes to the pandemic.
For Democrats (and independents who lean Democratic), the main thing that deserves more attention is “protecting public health.” In a nationally representative survey, 46% — nearly half — say health issues haven’t gotten the attention they deserve, while 7% say they’ve received too much.
Republicans (and independents who lean Republican) don’t agree. Just 20% of these folks feel that protecting public health should be a higher priority than it currently is, while 40% say it’s already gotten more attention than it deserves.
Stop and think about that for a minute — 46% of Americans on the blue side of the political spectrum think the country isn’t paying enough attention to protecting public health, while 40% of Americans on the red side think we’re paying too much.
Similarly, 52% of Democrats (and independents who lean Democratic) say “limiting health risks for vulnerable populations” should be a higher priority for the country and 6% of them say it should be a lower priority. Among Republicans (and independents who lean Republican), 31% say more should be done to make life safer for those who are vulnerable and 20% say the country is doing too much.

So what do the more conservative among us think we should be focusing on instead? More than two-thirds of them — 69% — say Americans need to up their game when it comes to “respecting individuals’ choices.” Only 28% of their more liberal counterparts agree.
In the liberal camp, 33% feel the country pays too much deference to individual choice. That view is shared by just 11% of the conservatives.
By a margin of 62% to 34%, Republicans (and Republican leaners) are also more likely than Democrats (and Democratic leaners) to say the country should place a higher priority on “supporting business and economic activity.” At the same time, 10% of Republicans and 15% of Democrats say business and economic concerns receive too much emphasis.
It’s not only the problems we see differently — it’s the solutions too.
For instance, 75% of Democrats (and Democratic-leaning independents) say COVID-19 vaccines have been either “very” or “extremely effective” in reducing coronavirus spread. Only 32% of Republicans (and Republican-leaning independents) agree. Given these views, it’s no wonder there’s such a huge partisan gap in vaccination status.
Or consider face masks. In the poll, 71% of Democrats (and Democratic leaners) say wearing masks around others while indoors is an effective way to reduce coronavirus spread. That view is shared by just 21% of Republicans (and Republican leaners). If you’re of the opinion that masks aren’t helpful but you’re confronted with a government rule that forces you to wear one anyway, it’s no wonder you’d think the country hasn’t done enough to prioritize respect for individual choices.
The poll was conducted May 2-8 among a nationally representative group of more than 10,000 Americans. The margin of error for responses comparing people based on their political views was plus or minus 2.2 percentage points.
“The overall findings reflect two competing critiques of the nation’s response,” the authors of the Pew report wrote. “One, widely expressed among Republicans, is that the country has not focused enough on business concerns and respecting individual choices. The other, more widely held by Democrats, centers concern around efforts to protect public health and limit health risks for vulnerable populations.”
At least there’s one thing Americans across the political spectrum agree on: “Neither Republicans nor Democrats think the country has hit the mark in its response to the outbreak.”
By the numbers
California cases and deaths as of 4:55 p.m. on Tuesday:
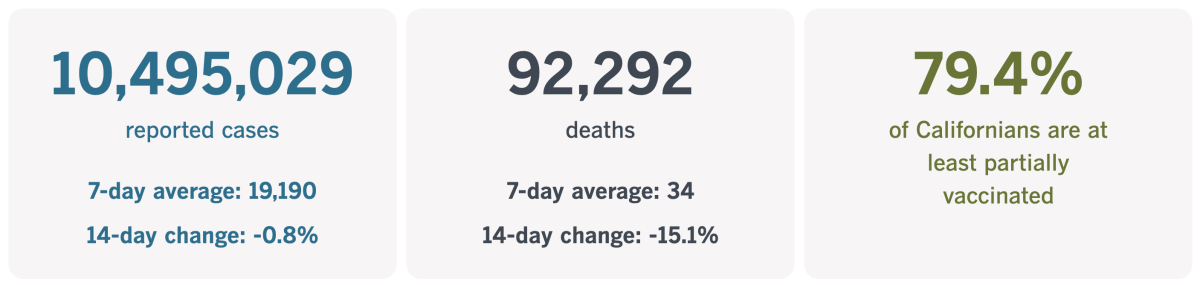
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
A number you can’t count on
Imagine you’re standing on the sidewalk when a car whizzes past. You can tell it’s going fast — too fast. But if you had to estimate its speed, could you say whether it was going 65 miles per hour? 80? 100?
This is the predicament of those who sincerely care about the number of coronavirus infections in their community. They can tell that the number is high — and growing. But they’re hard-pressed to pinpoint it with any certainty.
The case-counting problem has been with us throughout the pandemic. In early 2020, health experts quickly realized that the coronavirus had been circulating more aggressively than they’d initially believed. Once the official case count took off, the health establishment recognized that infections were going uncounted because we lacked the tools to identify them.
When coronavirus testing sites were finally up and running and people queued up by the hundreds to have their nostrils swabbed, the case counts omitted the significant number of people with asymptomatic infections who didn’t know they should be in those lines. As far as researchers can tell, roughly 40% of infections produce no COVID-19 symptoms, leading to the phenomenon of silent spreaders.
And when the long lines were made obsolete by rapid home testing kits, it was widely acknowledged that plenty of positive results never made their way into the official statistics. (Indeed, some local health departments have no way for people to report their home test results, even if it occurred to them to try.)
Health agencies — from the Los Angeles County Department of Public Health to the Centers for Disease Control and Prevention to the World Health Organization — continue to update their coronavirus case counts. Officials may have less confidence in the totals, but at least they can see whether the numbers are rising more or less rapidly than in the past.
“We don’t have to count every case to understand what’s happening in our communities,” Michael T. Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told my colleague Emily Alpert Reyes. “What’s important is to understand the general trend of how cases are changing.”
Right now, the general trend is that the virus “is widespread in our communities everywhere,” Osterholm said. “The bottom line is, extensive transmission is going on.”

Modeling studies by researchers at the University of Washington’s Institute for Health Metrics and Evaluation estimate the official counts include only 14% of actual infections.
The lowball counts leave the public with the false impression that daily activities are a lot safer than they really are.
“People now may be doing things that they don’t realize are going to put them at high risk of getting infected” and infecting others, said Dr. Abraar Karan, a fellow in the Division of Infectious Diseases and Geographic Medicine at Stanford University.
Here in L.A., officials rely on more than just test results to gauge coronavirus activity. Data from hospitals and wastewater monitoring systems help fill in the gaps.
“We feel confident that we have a decent grasp on the level of spread across the county,” said L.A. County Public Health Director Barbara Ferrer.
That’s not exactly as confidence-inspiring as some people would like it to be.
Without reliable data, it’s difficult for health officials to justify the need for mask mandates, vaccine verification programs and other safety rules. The public might be more receptive to measures like these if the people in charge could point to hard metrics and say, “Look, we’ve gone from Point A to Point B — and we’ve crossed a line that is very important,” said Mark Rothstein, a public health and bioethics expert.
“You want your public health systems to develop responses that are based on these sorts of metrics,” added Dr. David Dowdy, an infectious-diseases epidemiologist at the Johns Hopkins Bloomberg School of Public Health. “As these metrics become less reliable ... you’re left with going back to what it was before, which is just kind of a general sense of where things are headed.”
California’s vaccination progress
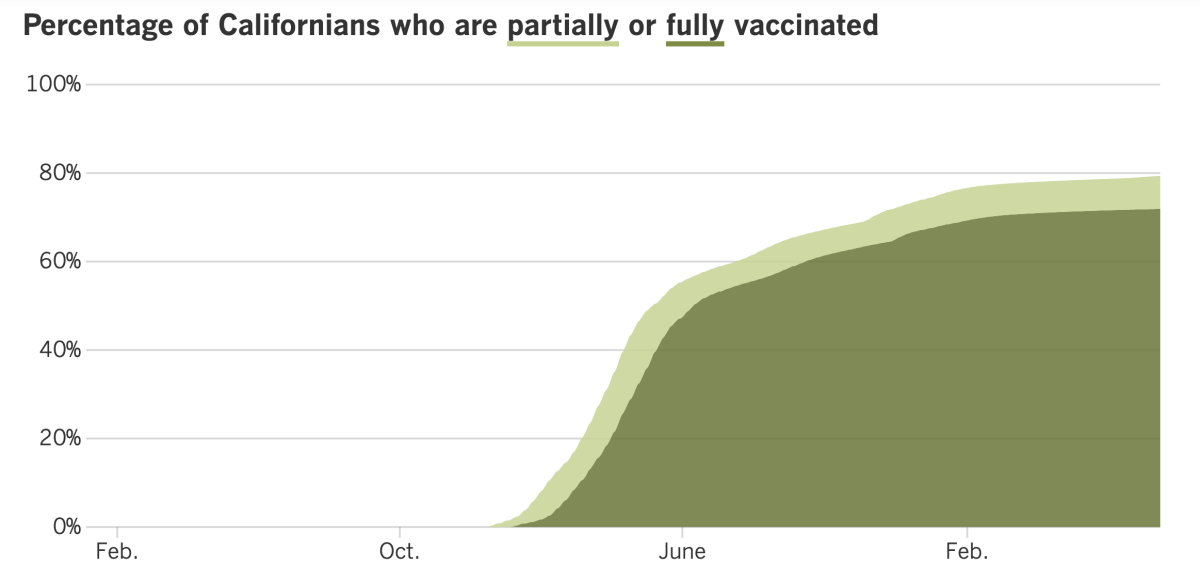
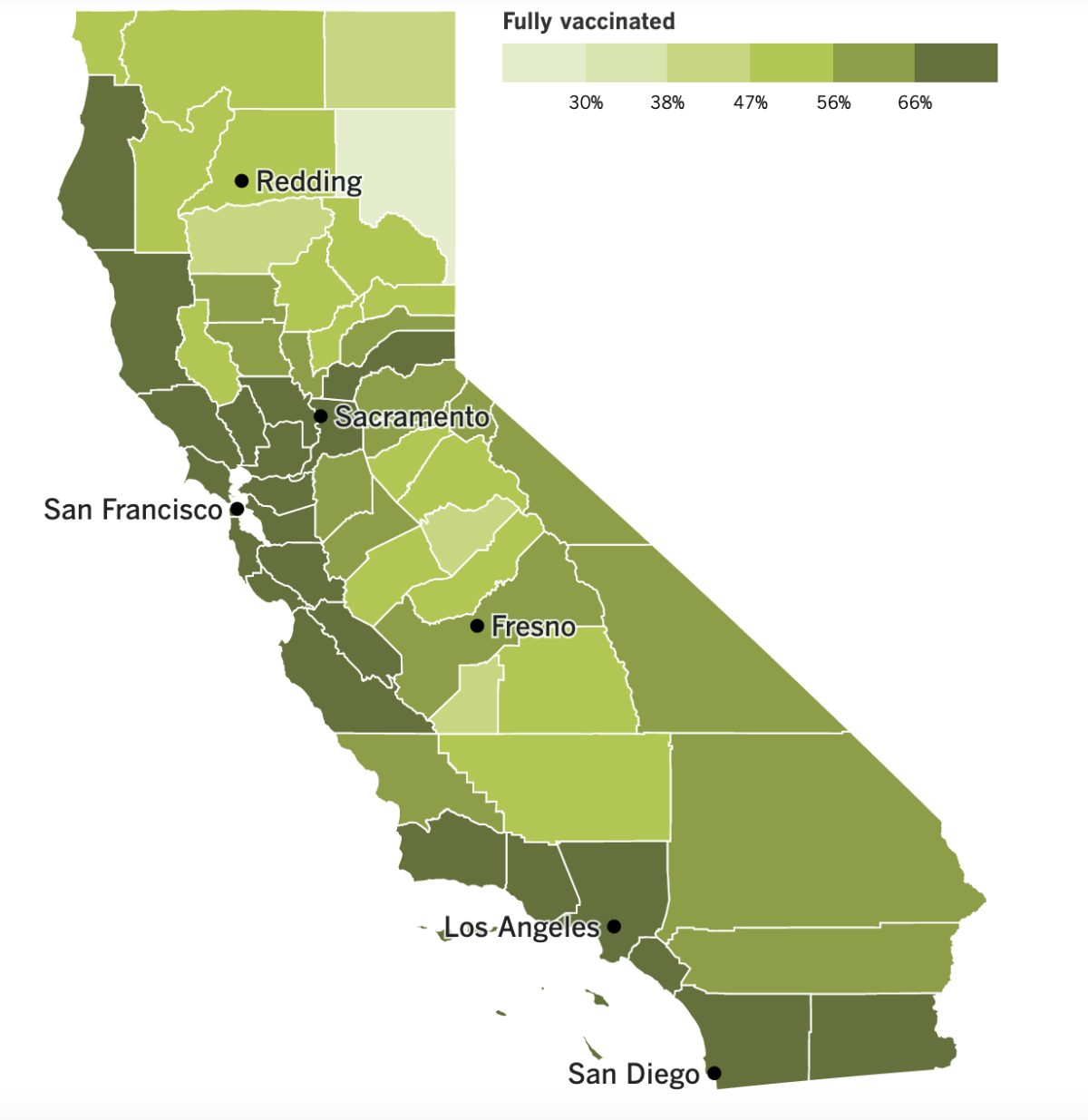
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
It’s hard to escape the feeling that things are moving in the wrong direction.
The latest version of the CDC’s map shows 42 of California’s 58 counties colored orange, indicating they have high COVID-19 community levels. As of Thursday, those counties included Los Angeles, Orange, San Diego, Imperial and Santa Barbara. Considering that Ventura earned a “high” designation the previous week, almost all of Southern California is now in the highest tier of coronavirus risk. The only exceptions are Riverside and San Bernardino counties.
The list of orange-colored counties also includes all of the San Francisco Bay Area, most of the Central Valley, and every coastal county except Santa Cruz and Humboldt.
When you add it all up, 87% of Californians reside in a place with a high COVID-19 community level. A week ago, 41% of Californians lived in a county in the “high” category.
L.A. County, the most populous in the country, is now averaging about 6,900 coronavirus cases per day. Not only is that 27% higher than it was a week ago, but it’s also nearly double the peak case rate from last summer’s Delta surge. Those numbers translate to a rate of 476 cases per 100,000 residents per week. (Anything over 100 cases per 100,000 residents per week is considered high.)
You may be thinking that most of those cases are mild — and that’s true — but COVID-19 deaths are climbing too. Over the last month, the L.A. County’s weekly death toll has increased from 50 to between 88 and 100.
Statewide, infections are up 16% week to week, and deaths are up to about 255 per week. The people who keep tabs on coronavirus levels in wastewater say that, in some parts of the state, the virus is more widespread now than it was during the winter’s original Omicron surge.
Although there are dire signals coming from pretty much all parts of the state, Los Angeles is the only county with plans to reinstate a mask mandate. The clock began ticking last week when the county’s hospitalization numbers downgraded its COVID-19 community level from “medium” to “high.” If it stays in the “high” category, a new mask mandate will go into effect on July 29.
That mandate will require everyone age 2 and older to wear a mask in indoor venues such as stores, restaurants, bars, gyms, museums, schools and shared offices. They wouldn’t be required when people are actively eating or drinking, or when people are outside.
Business groups are already asking Ferrer to reconsider her plan. In a letter to the county health chief, they wrote that requiring masks “puts employees in the increasingly challenging position of enforcing a mandate that many customers no longer wish to — or are unwilling to — comply with.”
Another concern is that customers who don’t want to wear masks will simply take their business to a neighboring county where masks aren’t required.
Those in the anti-mandate camp got some support from Dr. Brad Spellberg, the chief medical officer for Los Angeles County-USC Medical Center. About 90% of patients with coronavirus infections there were admitted for other reasons, he said in an internal town hall meeting that was posted online.
“Virtually none of them go to the ICU — and when they do go to the ICU, it is not for pneumonia. They are not intubated,” he said, citing other issues such as electrolyte abnormalities.
“It is just not the same pandemic as it was, despite all the media hype to the contrary,” Spellberg added. “A lot of people have bad colds, is what we’re seeing.”
Epidemiologist Dr. Paul Holtom seconded that view. Although the rise in hospitalizations is the trigger for the mask mandate, he said “there’s no reason, from a hospitalization-due-to-COVID perspective, to be worried at this point.”
L.A. County Department of Health Services, which has oversight of County-USC, disputed that view. The pandemic “remains a very serious public health threat that we must continue to fight with every tool available,” the department said in a statement.
Indeed, outbreaks at L.A. County workplaces have nearly quadrupled since early May. Affected businesses include airports, aerospace firms, Hollywood film and television production, and food processing companies. County health officials advised employers to expand options for remote work to reduce crowding on the job.
Increased uptake of COVID-19 vaccines may help too, and a new shot from Novavax could move some American adults from the unvaxxed to the vaxxed column. The CDC’s vaccine advisory group met Tuesday and voted unanimously to recommend it. Dr. Rochelle Walensky, the CDC director, did just that.
The newfangled vaccines from Pfizer-BioNTech, Moderna and Johnson & Johnson deliver genetic instructions to cells so they will make harmless copies of the coronavirus’ spike protein. Millions of Americans have rejected that new technology, and the CDC advisors expect those skeptics to be more comfortable with the Novavax shot, which employs a familiar technology used in vaccines for shingles, hepatitis B and other diseases.
“I’m really positive about this vaccine,” said Dr. Pablo Sanchez of Ohio State University, a member of the CDC advisory group.
The federal government has already purchased 3.2 million doses. Like the Pfizer vaccine, the one from Novavax requires two doses given three weeks apart. In clinical trials, the shots were safe and about 90% effective at preventing COVID-19 symptoms.
Speaking of vaccines, about 25 million kids around the world have missed out on routine childhood immunizations as a result of the pandemic, according to a new report from the World Health Organization and UNICEF. In some cases, vaccinations were missed because the pandemic interrupted regular health services; in others, misinformation about COVID-19 shots turned people off of vaccines altogether.
“This is a red alert for child health,” said Catherine Russell, UNICEF’s executive director. “We are witnessing the largest sustained drop in childhood immunization in a generation,” and its consequences will be measured in lives lost.
Another report from the WHO said coronavirus cases across Europe had tripled in the past six weeks and now accounted for nearly half of all infections globally. The rise in cases has caused hospitalization rates to double, though intensive care admissions have remained low.
And finally, we won’t have Dr. Anthony Fauci to kick around much longer. The nation’s top infectious diseases expert said Monday that he plans to retire before President Biden’s current term ends in January 2025.
The 81-year-old Fauci has been running the National Institute of Allergy and Infectious Diseases since 1984. He spent decades fighting disease like HIV/AIDS, respiratory infections, Ebola and Zika before becoming a household name during the COVID-19 pandemic.
Fauci said his decision wasn’t motivated by politics.
“It has nothing to do with pressures, nothing to do with all of the other nonsense that you hear about, all the barbs, the slings and the arrows,” he said. “That has no influence on me.”
Your questions answered
Today’s question comes from readers who want to know: What is Centaurus?
It’s a constellation in the southern sky, but that’s not the answer you’re looking for. The one that’s relevant to a coronavirus newsletter is either:
a) The nickname of the new Omicron subvariant BA.2.75.
b) Nothing you need to worry about right now.
c) All of the above.
The correct answer is c.
WHO’s names for variants of concern and variants of interest are based on Greek letters. That’s your first clue that Centaurus isn’t an official moniker. Your second is this tweet from July 1, in which an avid coronavirus commenter announced, “I have just named BA.2.75 variant after a galaxy. Its new name is Centaurus strain. Get used to it.”
BA.2.75 got attention for spreading rapidly in India and has turned up in roughly 10 countries. About a dozen infections involving the subvariant have been identified in the U.S. by Helix, which supplies sequencing data to the CDC. At least two of those cases were in California, including one in Los Angeles County.
In an analysis of variants detected in the U.S. over the past 15 days, 0.03% were BA.2.75. That’s lower than the unheralded BA.2.74 (at 0.06%) and BA.2.76 (at 0.08%). And none of those are anywhere near high enough to rate a mention on the CDC’s COVID Data Tracker.
BA.2.75 has several mutations on its spike protein that scientists find concerning. Researchers who are sharing their preliminary test results online report that the subvariant is probably more adept at evading the immune protection of vaccines and past infections than BA.2.12.1 but less adept than BA.4 and BA.5 (which share the same spike protein).
But “it’s still really early on for us to draw too many conclusions,” said Matthew Binnicker, director of clinical virology at the Mayo Clinic in Rochester, Minn.
One thing we can say for sure: The coronavirus isn’t fading away, so it’s necessary to remain vigilant against all subvariants.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The unusual watercraft in the photo above is a dragon boat. The racing of dragon boats is an ancient Chinese sport — possibly the oldest team sport there is.
This boat, painted with green scales, is being rowed by members of the D.C. Dragon Boat Club in our nation’s capital. The woman with the blue shirt, white visor and ponytail is Kimbriell Kelly, the paper’s Washington Bureau chief. She’d been a competitive dragon boat paddler for several years before giving it up to focus on her career.
Running a bureau of 30 journalists would be draining under any circumstances, but keeping up with an unrelenting news cycle in the midst of a pandemic was a sure recipe for burnout. Kelly’s aunt suggested she recharge by getting back on the water. Two months latter, Kelly was ready to give it a try.
“Like so many of us during the pandemic, I didn’t have a work problem. I had a life problem,” she wrote. “The solution would be dragon boats. And they would send me on an improbable quest.”
That quest was to earn a seat in the boat when the club competed against teams from Hungary, South Korea, Singapore, Thailand, India, Britain and Canada in the Club Crew World Championships later this month. Read her story to find out whether she succeeded.

Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




