Coronavirus Today: Pandemic resolutions for the new year (and beyond)
- Share via
Good evening. I’m Karen Kaplan, and it’s Tuesday, Dec. 20. We’ll be taking a holiday break for the next two weeks so this will be the last edition until Jan. 10. I hope you stay COVID-free as you celebrate with friends and family! In the meantime, here’s the latest on what’s happening with the coronavirus in California and beyond.
With December drawing to a close, it’s time to start thinking about New Year’s resolutions. Thanks to our pandemic-era work-from-home culture, I’ve finally knocked two long-standing items — prepare more meals from scratch and spend more time reading — off my list. (I’m still working on getting eight hours of sleep per night.)
The people who are already thinking about the next pandemic have some resolutions too. Their goal is to get the world in better shape to meet the next global health crisis when it inevitably arises.
These folks are working under the auspices of the World Health Organization, which explains their klunky name: the Intergovernmental Negotiating Body, or INB for short. You can think of it as a pandemic version of the United Nations’ Intergovernmental Panel on Climate Change, or IPCC.
The INB represents 194 member states, and getting everyone to agree on a plan won’t be easy. So far, the members have agreed to produce a first draft of a legally binding agreement sometime next year. They gathered in Geneva this month and will meet again in February. If they stick to their schedule, their final accord will be ready to be presented to the World Health Assembly, the WHO’s decision-making body, in May 2024.
Though there’s still a very long way to go, it’s clear from INB’s “conceptional zero draft” (a first draft of its first draft) that the experts are thinking big. Members are examining the cultural, educational, economic, political, legal and environmental issues that influence the public’s health and its ability to respond to — if not prevent — an outbreak of pandemic proportions.
They’re also embracing the One Health approach, which acknowledges that our health depends on the health of other animals and the environment we share. The SARS-CoV-2 coronavirus is believed to have originated in bats, then likely infected other animals before jumping to humans at a market in Wuhan, China. Influenza, which has caused four pandemics in the last century, comes from birds. The more carefully we tread in the world, the lower the risk that a dangerous pathogen will cross the species barrier.
The conceptual zero draft lays out core principles that negotiators would like to see reflected in the final agreement, including the notions that “all lives have equal value” and that the “enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being.”
It also recaps some of the failures of the world’s COVID-19 response, including the inability to ensure that all countries received vaccines, personal protective equipment, medical supplies, oxygen, coronavirus tests and other essential items in a timely manner.
Then it gets to the most consequential part — its goals. In its current form, it reads more like a wish list than an enforceable treaty. Still, knowing what the INB would like to see happen ought to shed some light on what the final agreement will contain.

The draft calls on countries to shore up their health systems so that, even in a pandemic, the public can maintain access to routine care without having to worry that their doctors — or urgent care clinics or hospitals — are swamped with sick patients. What’s more, the document urges countries to implement universal health coverage to boost their citizens’ baseline health and make it easier to help them deal with the aftermath of an outbreak.
Public health infrastructure should be strengthened too, so there can be enough people to track an outbreak and develop the tools and systems necessary to contain it. That includes distributing vaccines (once they become available), managing diagnostic laboratories and gathering specimens for genetic analysis, among myriad other tasks.
Both of those things will require a skilled workforce. To that end, countries should recruit capable people from all corners of society and make sure good talent isn’t being wasted due to gender, racial or ethnic discrimination, the draft says. In addition, countries should jointly support a “global public health emergency workforce” whose members can be dispatched to hot-spot areas as needed.
Hot spots will need stuff as well as people. That means nations will have to work together to create supply chain networks capable of getting resources anywhere in the world as rapidly as possible. They’ll also need affordable access to intellectual property, such as recipes for making lifesaving medicines and vaccines. Private companies should be encouraged to share their know-how and waive their licensing fees during an emergency, the draft says.
Crucially, the countries that ultimately sign this agreement should commit to increasing “science, public health and pandemic literacy,” according to the conceptual zero draft. That will mean studying the ways misinformation and disinformation spread and scouring social media to flag falsehoods that gain traction. Then someone will need to come up with a way to convince people what’s fake news and what’s real. (Amen to that!)
This is not an exhaustive list of what the INB members think it will take to up our game in a future pandemic. Even if it were, it’s not as though making these things happen will be easy.
Likewise, I can almost guarantee that 2023 will not be the year that (finally) sees me getting more than six hours of sleep a night. But I’d really like want it to be. And if that New Year’s resolution remains unfulfilled 12 months from now, it’ll be on my list for 2024. If I don’t even try to make it happen, it never will.
By the numbers
California cases and deaths as of 4:15 p.m. Tuesday:
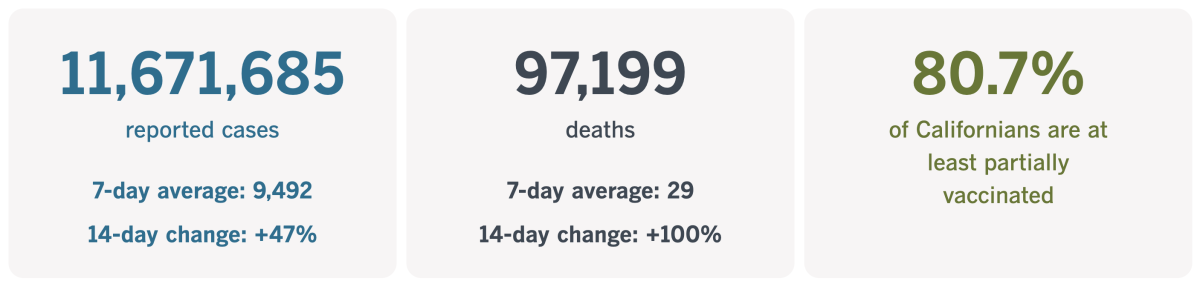
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
How the pandemic helped workers with disabilities
From our Pandemic Silver Linings Department comes a story about a group of marginalized people who are finally getting a chance to shine now that remote work for some has become the new normal.
I’m talking about people like Russel Rawlings of Sacramento, who has cerebral palsy. Before the coronavirus came along, he used to go into his office at a nonprofit independent living center five days a week. The 2-mile commute in his powered wheelchair required him to wake up at 5 a.m. in order to be at his desk by 8 a.m.
Now Rawlings has a new job that he can do from home full time. Being an education organizer for a nonprofit that assists domestic workers is a huge step up because it doesn’t require a difficult commute. (Another bonus: The work is more fulfilling.)
“I never thought I would be able to do community organization remotely,” said Rawlings, who struggled to find any job just a few years ago.
He’s hardly the only one. The Bureau of Labor Statistics says more than 7.3 million people with disabilities were in the labor force last month, an increase of nearly 25% since the start of the pandemic.
The unemployment rate for these workers now stands at 5.8% — nearly twice the rate for workers as a whole, but less than half what it was two years ago. In fact, the current jobless rate for workers with disabilities is the lowest it’s been since the government began tracking it in 2008, my colleague Don Lee reports.
The country’s embrace of telework is “a total game changer,” said Mason Ameri, who studies disability employment trends at Rutgers Business School.

In theory, the Americans with Disabilities Act of 1990 was supposed to make life easier for these workers. The law says employers must be willing to make a “reasonable accommodation” to an employee with a disability.
Deciding what counts as “reasonable” is often tricky, but the pandemic has provided abundant evidence that a wide array of jobs can be performed perfectly well from home — a fact that makes it difficult for an employer to call such an arrangement unreasonable.
“Before the pandemic, a lot of employers were saying, ‘Hey, remote work for managers, uh-uh — it’s just not doable,’” said Fiona Ong, an employment attorney who serves as the general counsel to the Maryland Chamber of Commerce. But “if somebody has been doing remote management, and doing it successfully, to then say it’s not reasonable is kind of a dangerous thing to say.”
Now that the economy is flirting with recession and layoffs are on the rise, remote workers are feeling vulnerable, especially if their employers are insisting on more face time in the office. Those trends could stall — or even reverse — the recent gains made by people with disabilities.
Melissa Merrell isn’t dwelling on that prospect. She has a genetic disorder that affects her vision and hearing, but her disability has been much easier to manage since the pandemic lockdown offered her the chance to work at home.
“Oh, God, my dream came true,” she said.
Telework eliminated her 90-minute commute to her job at the Travis Assn. for the Blind in Austin, Texas. It also allowed her to stop sharing an office with three other people and work in a quieter environment. Both developments have made her far more productive than she was in the pre-pandemic days.
Merrell is channeling some of her extra time and energy into accounting classes at a community college. She can envision her future self in a job with more responsibility than she has now, perhaps working as a comptroller, she said, or even a chief financial officer.
California’s vaccination progress
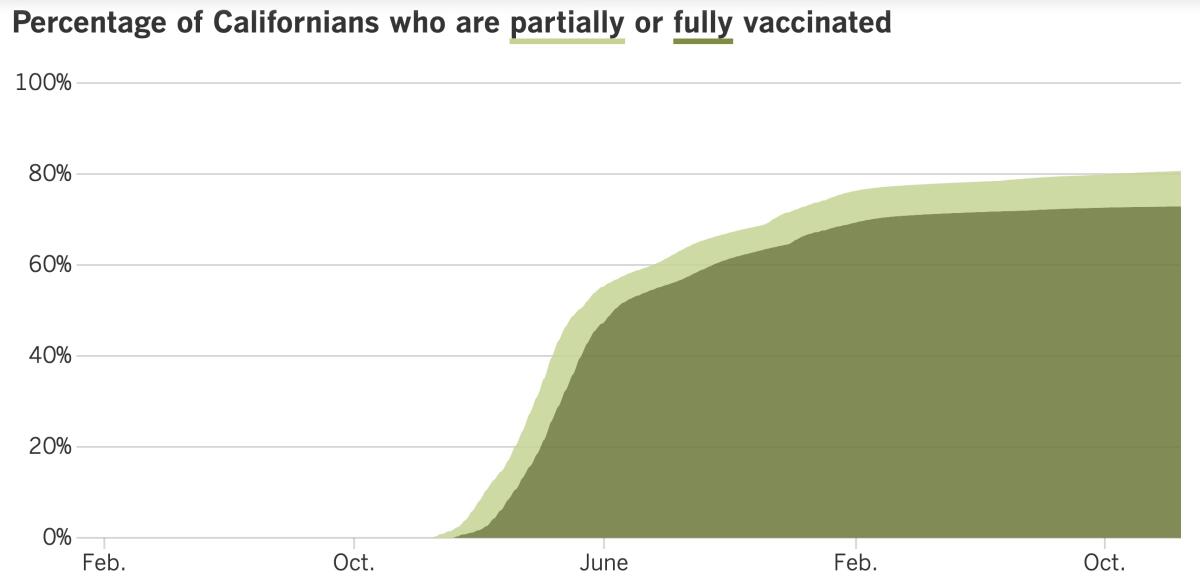
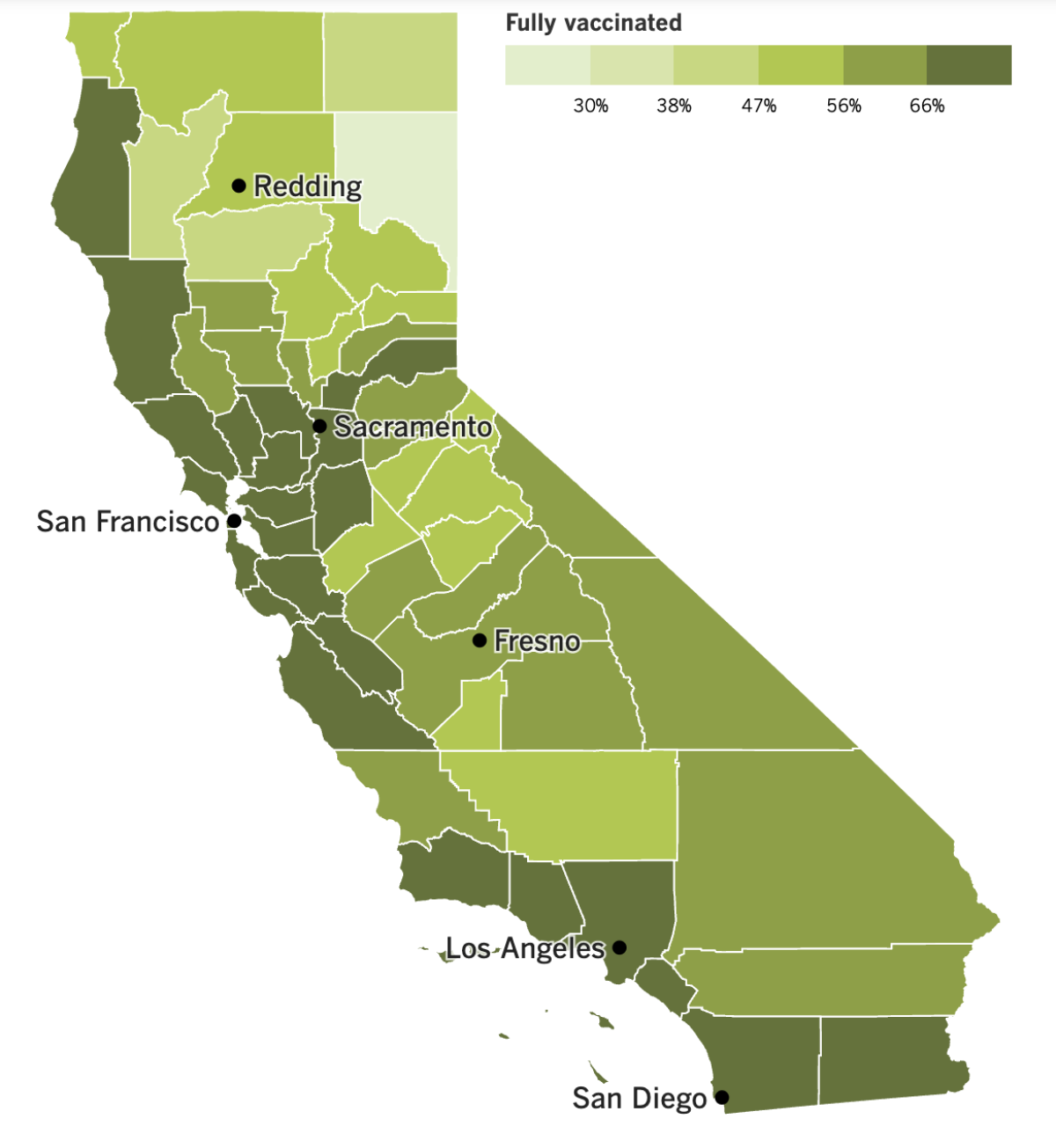
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Good work, Los Angeles County! You’ve managed to stem the rise in coronavirus cases — for now, anyway.
The county tallied 2,911 cases per day in the week that ended Friday, which works out to 202 cases per 100,000 residents per week. That rate is more than double what it takes to qualify as a “high” rate of transmission, but it’s still 20% lower than it had been a week earlier.
Barbara Ferrer, the county’s director of public health, isn’t ready to say cases are on the downswing, only that they’ve plateaued. Wastewater surveillance indicates that there’s plenty of coronavirus going around, with viral levels in early December surpassing the peak seen during the BA.5 wave this summer. And holiday celebrations could give the virus a boost, potentially putting a countywide indoor mask mandate back on the table.
“As we get closer to Christmas and Kwanzaa and there’s Hanukkah, winter solstice ... I think that might drive another increase in our cases,” Ferrer said, adding “but I don’t have a crystal ball.”
L.A. County is now one of only two counties in California with a “high” COVID-19 community level, according to the Centers for Disease Control and Prevention. The other is Imperial County, just east of San Diego County. Six other Golden State counties that were in the “high” category last week have since dropped into “medium” or “low” territory.
Hospital admissions involving coronavirus-positive patients fell 4% week to week in the L.A. area, the CDC said. Still, combined with the “tripledemic” threats of influenza and respiratory syncytial virus, or RSV, the number of available beds in the county fell to 242 last week, the lowest level since the start of the pandemic, Ferrer said.
And here’s an ominous statistic from the CDC: L.A. County’s latest COVID-19 mortality rate rose 46% in a single week. It now stands at 1.05 deaths per 100,000 residents per week.
An excellent way for infected people to reduce their risk of serious illness or death is to start treatment with Paxlovid as soon as possible. In one study involving more than 2,200 patients, those who were randomly assigned to take the drug were 89% less likely to become severely ill. Yet for some reason, many doctors aren’t prescribing it.
Some frustrated doctors have complained on Twitter about their colleagues’ reluctance to take advantage of Paxlovid and another antiviral called molnupiravir. Dr. Taison Bell, an infectious-disease specialist at the University of Virginia, called out the physician who declined to prescribe Paxlovid to his wife’s grandmother, who is in her 90s.
“This is exactly the kind of person you definitely want to get Pax,” he tweeted, referring to Paxlovid. “And she was denied.” (After calling the grandmother’s doctor, the prescription came through, he added.)
Dr. Purvi Parikh, an immunologist at New York University’s Grossman School of Medicine, is also mystified. “Why are doctors still so afraid to rx (prescribe) Paxlovid,” she tweeted. “It’s been a game changer for my patients. Treat early and aggressively!”
Whether they take Paxlovid or not, people with active coronavirus infections should stay home from work. For two years, the state of California has dissuaded sick people from showing by guaranteeing sick pay to those who caught the virus while on the job.
That guarantee is coming to an end next year. The California Occupational Safety and Health Standards Board voted to drop it on the grounds that in the Omicron era, it can be extremely difficult to tell whether someone became infected at work or somewhere else.
Speaking of government interventions, a new report from the Economic Roundtable credits a few key ones with keeping thousands of people off L.A. County streets during the pandemic. The research organization’s study estimated that although homelessness in the county rose 13% from 2020 to 2022, it would have increased 23% without eviction moratoriums and cash from stimulus payments and extended unemployment insurance. Similar measures should be used again next year if the economy falls into recession, the study authors wrote.
Los Angeles’ nearly 3-year-old eviction moratorium is now in its waning days. This month, the City Council confirmed that L.A. landlords will be able to evict tenants who don’t pay their rent starting Feb. 1. However, landlords still won’t be allowed to raise rents for more than 650,000 rent-controlled units until February 2024.
On the research front, a new study from the CDC has found that the mysterious condition known as long COVID was a factor in at least 3,544 deaths in the U.S. Researchers arrived at that figure by scouring deaths certificates recorded through June that referenced terms like “long COVID,” “long-haul COVID” or “post-COVID syndrome.” However, they suspect their number is an undercount because of the inconsistent way causes of death are coded.
Heart arrhythmias, blood clots, anxiety and sleep difficulties are some of the long COVID symptoms that can lead to premature death, experts said. Symptoms like these can crop up even in people whose coronavirus infections were asymptomatic, they noted.
And finally, China is continuing to ease up on its “zero COVID” rules. Last week, the government said it would stop keeping track of asymptomatic infections because they’re impossible to identify without widespread coronavirus testing. This week, some local governments told residents it was fine to go to work with an active case of COVID-19 as long as their illness was mild. A city in the southern Guizhou province said this advice applied even to medical, health and emergency workers, among others.
The country’s official death toll is slowly rising. On Monday, authorities announced two COVID-19 deaths in Beijing, the country’s first pandemic fatalities since Dec. 4. Five more deaths were announced today, all of them in Beijing.
Officials in the U.S. are expressing concern that new coronavirus variants could arise in China as the virus spreads through a country with 1.4 billion people.
“When it comes to the current outbreak in China, we want to see this addressed,” a State Department spokesman said Monday. “We know that any time the virus is spreading in the wild that it has the potential to mutate and to pose a threat to people everywhere.”
Your questions answered
Today’s question comes from readers who want to know: How can I celebrate the holidays without getting COVID-19?
If you’ll be spending time around other people, you may find yourself spending time with the coronavirus as well. The last two pandemic holiday seasons have made this abundantly clear.
That said, there are things you can do to reduce your risk of getting sick if the virus crosses your path. Nothing on this list should come as a surprise, but the items do bear repeating:
Get up to date with your COVID-19 vaccines. If you haven’t finished your primary vaccination series, there’s no time like the present. And if you have, be sure to get your bivalent booster shot if you’re eligible. The only reasons to delay are if you’ve received a dose of vaccine in the last two months or if you came down with COVID-19 in the last three months.
Consider wearing a mask. Face coverings are not required in L.A. County, but they’re strongly recommended in indoor public settings. State health officials also recommend masks for people at risk of developing a severe case of COVID-19.
Maximize ventilation. You don’t want to breathe in air that may contain aerosolized virus. An outdoor gathering is less risky than an indoor one, but if you are indoors, you can reduce your risk by keeping doors and windows open, turning on fans to boost circulation, and using indoor air filters.
Wash your hands. Good hygiene counts. That includes covering your sneezes and coughs.
Test before you gather. You could have an active infection and not even realize it. That’s why it’s useful to take a rapid test the day you plan to meet other people. Yes, you could wind up burning through a lot of tests this way, but remember that while the federal public health emergency is still in effect, your health insurer must cover the cost of eight tests per person per month. Your household can also get four tests for free courtesy of the federal government.
Stay home if you’re sick. If you test positive for a coronavirus infection, stay home. If you test negative but are having active COVID-19 symptoms, stay home. It may be tempting to see your friends and family members, but rest assured: COVID-19 is not the gift they want to get from you this year.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

Remember how good it felt to finally hug people again after COVID-19 vaccines came out last year? Then you can imagine how excited Connie Su feels about seeing her parents, siblings, nieces and nephews in Taiwan next week.
Su, pictured above, is a dental hygienist who works in Newport Beach. She’s also the only member of her family in the United States. She hasn’t seen her relatives in person since the summer of 2019. It was possible to visit them before now, but a trip would have been a lot more time-consuming.
“Before, you had to sit in a quarantine hotel for 14 days waiting to exit to get to your loved ones,” she told my colleague Anh Do. “Who has that kind of time?”
Now those onerous rules are gone in most parts of Asia, spurring Asian immigrants to board planes to Taiwan, Hong Kong, South Korea and Japan this holiday season.
Grace Yoon of Fullerton is heading to Seoul with her family. Her parents will get to hug their 5-year-old grandson for the first time since he was an infant. Yoon also plans to visit the grave of her own grandfather, who died of pneumonia during the pandemic’s first year.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




