Sick staff. Endless COVID patients. Doctors ‘just scraping by’ as Omicron sweeps hospitals

- Share via
On a single day this week, 616 staffers called out sick with COVID-19 at Tufts Medical Center in Boston. Without nearly a tenth of its workers — doctors, nurses, administrators and janitors — the hospital assigned the National Guard to help with an unrelenting swarm of patients, many of them critically ill.
Such scenes around the nation have been brutal as the highly transmissible — if less deadly — Omicron variant has set a record of nearly 2 million infection cases each week. That surge has battered healthcare systems, sapped the morale of doctors and nurses, delayed thousands of surgeries, postponed treatments for life-threatening diseases such as cancer and turned hospitals into around-the-clock triage centers where nerves bristle and anger echoes alongside despair.
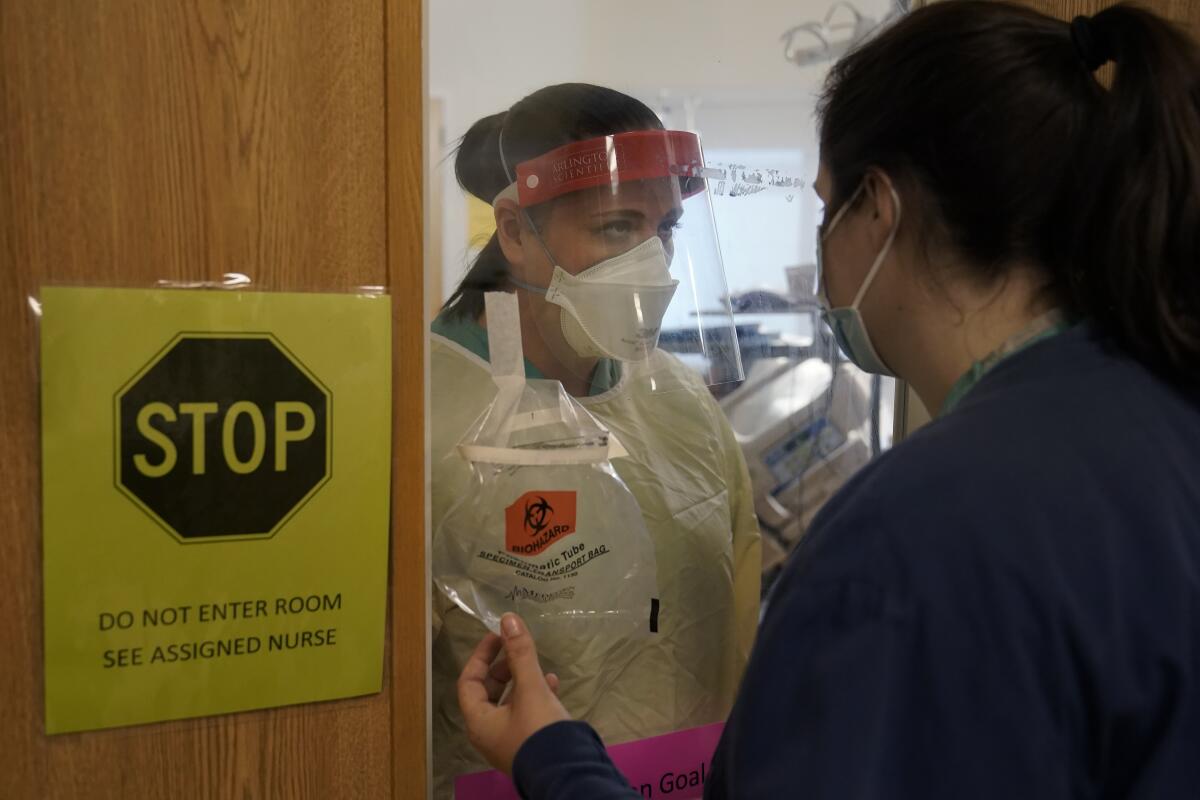
The daily grind of rising infections has left virtually no part of America untouched. It has changed how we think about the virus, the sick and medical communities in cities and towns that are barely coping as the pandemic approaches its third year. Masks and ventilators were once in short supply; now, it is the staff members. Front-line workers used to end their shifts by walking out of hospital doors to the sound of clanging pots and cheers. Today, many are fatigued and some even irate as a sea of unvaccinated Americans seek treatment.
In big cities, hospitals are reporting hundreds or thousands of workers out sick with COVID-19 each week.
Projections suggest Omicron may wane in coming weeks and months. But for now it is raging: This week, COVID-19 hospitalizations broke last January’s record of 132,051. Omicron has essentially changed the game, as if a storm had rearranged the landscape. The constant crush of patients — and the inability of many hospitals to treat them — is straining the patience and compassion of doctors, nurses and other medical staff.
Of the 24 beds in Dr. Jason Chertoff’s unit at the Genesis Hospital in Zanesville, Ohio — a town of 25,000 — four are blocked off and sit empty because there aren’t enough nurses. Nearly every patient is there with COVID-19, and Chertoff said most will die on a ventilator.
“I am used to it. But I am also fatigued. Before COVID, what I did a lot of was treating people with lung cancer. I never felt anything bad toward them if they were smokers,” said Chertoff, 43. “But what I don’t like is what I’m feeling now. I have resentment and anger toward patients not doing their part to curtail the spread of this. I have to put that aside and take care of people no matter their choices. That is my job. But, wow, is it hard.”
Ariana Cellini, a nurse who works 12-hour shifts at the Tufts intensive medical unit, shares the sentiment. She lives with her parents and grandmother, who has Alzheimer’s and diabetes. She still undresses from her scrubs in the breezeway outside her home and doesn’t hug or kiss her grandmother.
“At the beginning, there was great morale on the front lines,” she said. “Then, when people wouldn’t get vaccinated or said it was a hoax, many of us got angry. Now, we’re essentially numb.”

Like much of a restless country wanting to move beyond the coronavirus, especially as vaccinations rolled out last year amid a sense of a return to normality, hospitals were quickly reminded of the inventiveness and staying power of the virus. It has stretched the limits of what hospitals can do against a widespread, sustained threat complicated by testing problems, uneven government policies and a population where 27% of adults remain unvaccinated.
“We had so much hope, as vaccines were being distributed, that that was truly the end. You saw the cases plummet as they were being distributed,” said Dr. Shira Doron, an infectious disease doctor and hospital epidemiologist at Tufts Medical Center. “Delta and Omicron come along and teach you that anything can happen.”
Omicron has shown itself to be less lethal than prior variants, but its rapid, mercurial transmission has presented dangers hospitals and doctors have rarely confronted: “There are way, way, way too many infected employees,” Doron said. “Our curve of infections among staff right now makes all the previous waves look flat.”
At her hospital and others in states including Georgia, Maryland, Delaware and Ohio, the National Guard has been called in to bolster depleted staffs. In rural regions where Omicron took longer to arrive, overstressed small hospitals are once again hiring traveling nurses and transporting patients to cities for lack of beds. In 2020, nearly all hospitals shut down elective procedures to prioritize COVID-19 treatment. Today, those offering them are shifting schedules as routine surgery patients test positive. Some of the worst-hit hospitals are going back to solely serving as emergency COVID-19 treatment centers.
In California, staff shortages have led to an emergency policy that allows hospital workers who test positive for the virus to return to work immediately — with no isolation or additional testing required — if they show no symptoms. The California Department of Public Health put the rule in place as hospitals near capacity, and has told employers to make sure those workers mask up and are assigned to work with patients who are already infected.
In Arizona, leaders of Banner Health, the largest health system in the state and one of the biggest in the country with its 30 locations, warned this week that the worst was to come. The state has repeatedly set records for daily cases, with 18,783 new ones logged Wednesday.
“Nearly a third of our inpatient beds are now occupied by COVID or suspected COVID patients,” Dr. Marjorie Bessel, the chief clinical officer for Banner Health, said in a news conference this week. “Roughly 90% of those COVID patients are unvaccinated.” Intensive care unit beds, meanwhile, are more available than they were during the Delta variant’s peak.
In the Northeast, the first American region to be hit hardest in the current surge, hospital administrators said today’s challenges bear little resemblance to those that emerged when the virus first appeared 22 months ago.

“We are just scraping by,” said Doron, the epidemiologist at Tufts.
Diana Richardson, hospital’s chief operating officer, said an onslaught of patients who delayed treatments earlier in the pandemic has made things even harder. Tufts physicians are seeing “very sick patients that have nothing to do with COVID: cancer conditions that have worsened, orthopedic conditions that are far more painful, cardiac conditions that have progressed because of that deferred care,” Richardson said. “The burden is enormous. The sheer exhaustion among hospital staff is unbelievable.”
An administrator at Yale-New Haven Hospital in Connecticut, Dr. Maxwell Laurans, described dealing with “the most challenging Tetris game you can play to fit all these patients and employees into the slots that are available during this surge.”
Laurans oversees 1,250 employees in the hospital’s surgery division, where cardiac, orthopedic and cataract procedures are common. Those kinds of operations were delayed during the first wave. Now, they are again — but for a different reason.
“Every day, there are tens of surgeries we have to postpone because the patient tests positive,” he said. Then there is the staff. “We were already facing staff shortages prior to the pandemic. Now, we’re facing significant numbers of staff who are testing positive. On any given day, we have to redeploy 5- to 10% of our staff to another area to meet clinical needs.”
In Ohio, where hospitalizations have hit record highs and about 56% of the population is vaccinated, rural hospitals are under enormous burden. Chertoff, who works the overnight ICU shift and is a pulmonary specialist at Genesis Hospital in Zanesville — nearly 55 miles east of Columbus — said lack of vaccination was still the biggest health threat to communities such as the one he serves.
The county where he works, Muskingum, lags behind the state average with 47% of its residents vaccinated.
“The receptiveness to vaccines is lacking. There is such a resistance,” Chertoff said. “You can usually tell immediately when you see someone that they are unvaccinated — because of how severe their symptoms are. It’s such an impediment to getting people better and preventing the spread of the worst cases.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.















