
- Share via
RED BLUFF, Calif. — Jeremiah Fears sat beneath an elk head mounted on the wall of the volunteer fire department in his little city and rolled up his sleeve for what he hopes is a step toward normality: his first dose of Moderna’s COVID-19 vaccine.
“If we can get vaccinated and do our thing to protect one another and ourselves, we can hurry up and open and go from there,” said Fears, chief of the Corning Police Department. “I know there’s controversy behind it. But it is what it is.”
Fears had come to a vaccination clinic in Corning — population 7,600 — aimed at firefighters and police officers. But in that fire station was a hint of the pandemic skepticism that runs deep in rural Northern California: two elderly people, both on dialysis, who were coming to get their shots.
They had been put on standby because Tehama County health officials, who only brought two small vials containing 20 doses, suspected they might not attract enough firefighters or police officers to use them all.

In the battle against COVID-19, health officials in Northern California face the daunting task of vaccinating more than 683,300 people spread across a mountainous, heavily forested region where calamity — either from illness or physical trauma — can mean hours-long drives to the nearest medical facility.
Among their biggest obstacles: overcoming widespread skepticism that the virus is a serious threat in far-flung towns, fear that the new vaccine is unsafe, and open rebellion against health orders. The pushback in rural parts of California is emblematic of the challenge in many parts of the United States, particularly outside more liberal urban centers.
“We’re getting very frustrated here in Northern California,” said Dr. Richard Wickenheiser, the Tehama County health officer. “We have a lot of anti-vaxxers and a lot of independent people who just feel that COVID was a hoax, that it was going to go away when the election was over. And that didn’t happen. ... The excuses just go on and on.”
Public health messaging, he said, “isn’t working.”
In Shasta County, some speakers at supervisors’ meetings have compared mask mandates to Nazis forcing Jewish people to wear a yellow Star of David and spouted conspiracy theories about vaccines containing tracking devices. The county health officer has been threatened repeatedly.
In Tehama County, where indoor dining is banned by the state, restaurants were still seating maskless customers in recent days. In downtown Red Bluff, signs in store windows read: “Please respect everyone’s personal space. ... Masks are welcome, but not required” and “Due to pre-existing health conditions, some of the staff are not wearing a face mask” and “MASKS OK.”
There is skepticism and defiance across the Golden State. But in California’s conservative northern counties — where a sense of rural abandonment by the state government has long had residents wanting to form a new state called Jefferson — the region is, in some ways, now a victim of its own early luck in the pandemic.
The virus was slower to spread in Northern California than densely populated urban locales farther south, and residents said the state was cracking down too hard on rural communities. In Modoc County, the first coronavirus case was not confirmed until late July. Its first death wasn’t until last month.
The Northern California region — which includes Del Norte, Glenn, Humboldt, Lake, Lassen, Mendocino, Modoc, Shasta, Siskiyou, Tehama and Trinity counties — has been the only one of the five state-designated regions to not be placed under a stay-at-home order based on hospitals’ intensive care unit availability.
But now the area, like the rest of the state, is seeing a post-holiday surge in coronavirus infections. The region has 122 intensive care beds; as of Sunday, ICU bed availability was 24%.
If its ICU availability drops to 15% — which would trigger a stay-at-home order — that would mean there are only 18 beds across an area roughly the size of Indiana, not just for COVID-19 patients, but also for people suffering from heart attacks, strokes and trauma.
Four counties have no ICU beds at all: Glenn, Lassen, Modoc and Trinity.
“In the beginning, it was harder for people to appreciate the real risks to themselves because it seemed so far away in New York and L.A., but that’s not the case anymore,” said Dr. Gary Pace, the Lake County public health officer. “The numbers are up all around.”
In October, Lake County averaged about 33 new cases a week. In December, it averaged around 200.

For the two small hospitals there, the goal is often to stabilize patients needing specialized care before transporting them to bigger facilities, mostly in the Bay Area, Pace said. There’s a trickle-down effect when those urban hospitals become full themselves.
“If we get a huge surge and we can’t transfer people out, we’re going to be in a heap of trouble,” he said. “We’ve been spending a lot of time and sleepless nights thinking about this.”
Last month, Wickenheiser was so alarmed by public indifference that he penned a letter comparing the situation to the kind of emergency that Northern Californians are used to: wildfires.
“Availability of an effective and safe vaccine is hope on the horizon, like a caravan of CalFire trucks,” the letter said. “But we will need to equip ourselves with all these tools until we have manageable spot fires. Like a fire hose, a vaccine has minimal impact during a firestorm, but is effective at putting out a smoldering fire.”
The letter was issued by the Rural Assn. of Northern California Health Officers, a coalition of 11 county health officers, who said they were “gravely concerned” that hospitals could be easily overwhelmed.
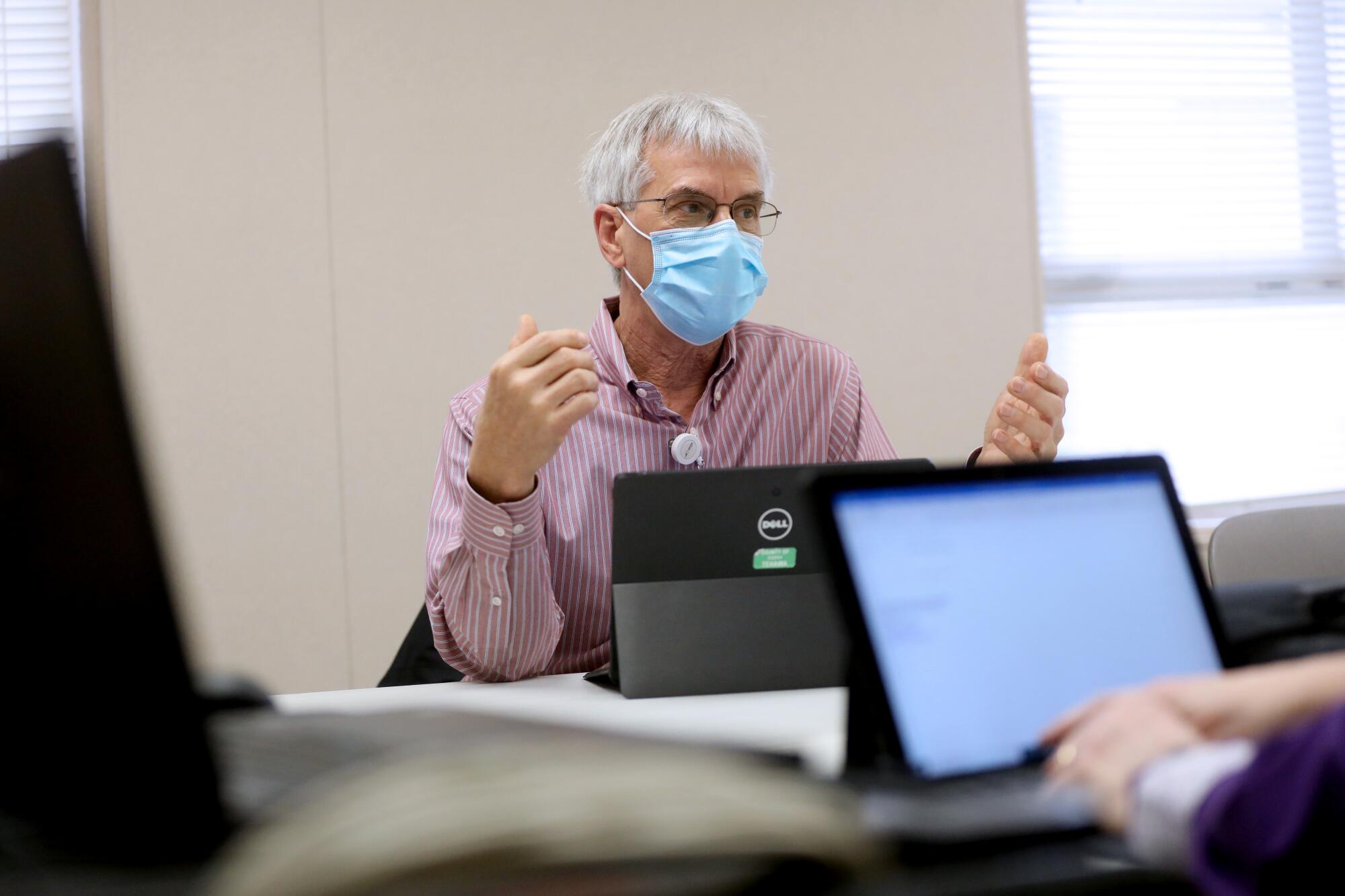
Wickenheiser — an amiable, bespectacled 66-year-old who has been the Tehama County health officer since 1985 — actually retired in 2017 and hopes to eventually spend his days on the tea farm he runs with his son. But as with many rural public health jobs, which pay less and require living and working in small towns, it has taken years to fill the position.
Wickenheiser, whose work badge dubs him “Extra Help,” offered to assist until a replacement arrived. The commitment was minimal. Until the pandemic.
There have been 10 months of seven-day workweeks and the learn-as-you-go logistical nightmare of securing COVID-19 tests when they were in short supply and, now, setting up vaccine clinics.
When it’s fully staffed, the county’s public health department has 41 positions. But it’s almost never fully staffed, said Minnie Sagar, the public health director. Currently, it has 27 employees.
Local health officials have faced another challenge: bearing the brunt of public anger toward health mandates and lockdowns, even though they have no authority to shut down businesses.
“We never thought public health would become so contentious,” Sagar said.

As of Sunday, Tehama County had recorded 3,971 cases and 42 deaths.
During a Jan. 6 meeting of the county’s COVID-response Department Operations Center, there was a quiet urgency as staffers sifted through the logistics of pandemic management.
There was personal protective equipment to order for vaccine clinics, which, in a few days, would start operating five days a week. There were volunteers to find for those clinics — they would reach out to school nurses and figure out how to respond to members of the public who had been calling in, offering to help.
A Red Bluff youth baseball league wanted to know whether it could resume competition. They would figure that out, too.
Michelle Schmidt, the supervising public health nurse, announced that the county had recorded a COVID-related death for three days straight in the first week of the new year.
A few hours later, at the vaccination clinic in the Corning Volunteer Fire Department, Randy Potter, a 67-year-old volunteer fireman, said he had stopped going to emergency calls during the pandemic because of his age. He works at a golf course and as a custodian at a high school and now spends much of his time “spraying everything with COVID killer.”
Asked why he got the shot, he laughed.
“Well, duh,” he said. “I’m hoping this is going to be the fix and things can go back to normal.”
Fears, the 42-year-old police chief, said more than half of his staff of 13 sworn officers and eight civilians have been vaccinated. He doesn’t like masks, which he said make it hard to read facial cues when interviewing suspects, but wears one regularly. He doesn’t push the issue with his officers.
Two hours later, the Palomino Room bar in Red Bluff was hopping. It was karaoke night. Old country hits were queued up. No one wore a mask.
The restaurant’s owner, Carlos Zapata, has refused to close or require facial coverings. He lives in nearby Shasta County and has gained a following since giving an August speech at the Shasta County Board of Supervisors — in which he warned that angry citizens are “not going to be peaceful much longer.”

Asked why he does not require masks, he told The Times: “Why would we? We’re not sick. Masks are for sick people.”
He said he believes the government is using COVID-19 “as a way to create fear in society and create control.” He has heard from state regulators after people complained, but is “not even a little bit” worried about being shut down.
In the bar, Leon Womack, a stout 77-year-old in a leather vest and black cowboy hat, said he was going to sing a cowboy favorite — then surprised the crowd with a soulful rendition of “At Last,” in the style of legendary rhythm and blues singer Etta James.
Womack said he is not worried about COVID-19.
“I don’t smoke. I don’t take drugs,” he said while sipping a brandy and Coke. “I don’t worry about it. If you get it, you get it. It’s no different than the flu.”
Jay Manor, the 30-year-old bartender, joked to a Times reporter that while he might “mask-shame you a little bit,” he didn’t really care whether people wore them. He lost his mother to cancer last month, and he said he’s just grateful to be still working in a small town where people supported him through that tragedy and are more relaxed all around.
“Right now, I don’t want to be anywhere but here,” he said. “I don’t want anyone telling me how to live.”
Times staff writer Matt Stiles contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.














