It’s a big mistake to think pandemic is over, despite recent good news, experts say

- Share via
So how much longer will the pandemic last?
No one is sure. Coronavirus cases are falling, but it would be a mistake to think the pandemic is over, experts say.
The last decline in cases means that we’re likely turning to a period of calm in this pandemic, representing a “containment” of the coronavirus, but “that is not the same as the pandemic being over,” Dr. Eric Topol, director of the Scripps Research Translational Institute in La Jolla, wrote in an op-ed for the Los Angeles Times this week.
“Unfortunately, when states or countries proclaim that we just need to live with the virus and end all restrictions, many people interpret that message as meaning the pandemic is actually over — for good,” Topol said. “That would be a fantasy given the myriad opportunities for the virus to haunt us in the months and years ahead.”
What history tells us
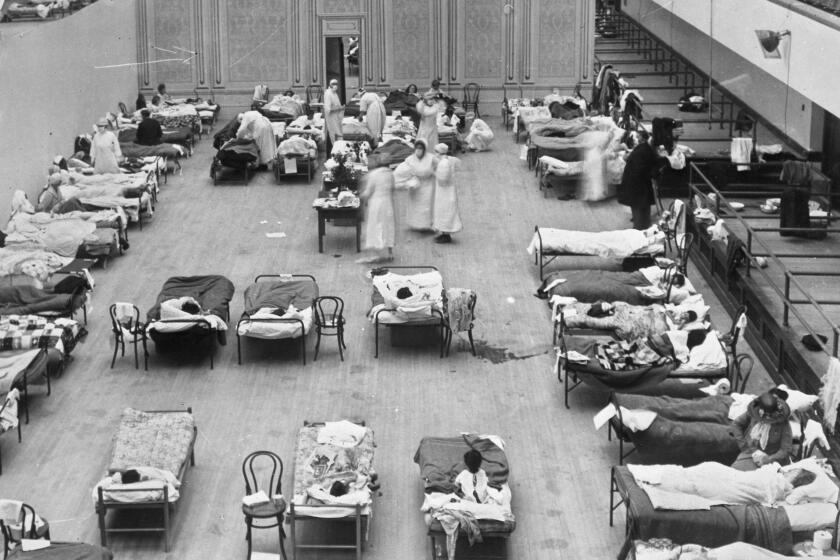
Recent history has shown that pandemics can last for several years. The 1918 flu pandemic persisted into a third year, with a fourth wave in 1920 even deadlier in some U.S. cities than the better-known second wave of late 1918, John Barry, author of “The Great Influenza: The Story of the Deadliest Pandemic in History,” wrote in a recent op-ed.
Lately, scientists are studying the “Russian flu” pandemic that began in 1889 for clues to how the COVID-19 pandemic may turn out — since some scientists suspect that pandemic was actually caused by a coronavirus rather than a flu virus.
There are parallels between the two pandemics. The Russian pandemic was first reported in the spring of 1889 in what is now Uzbekistan. It spread worldwide in three distinct waves over three years, Dr. George Rutherford, a UC San Francisco epidemiologist, said at Friday’s campus town hall meeting.
But, unlike what typically happens with the flu, which is usually hardest on the very young and old, “this just got the old,” Rutherford said. And the distinctive symptoms in the 1889 pandemic included loss of taste and smell — traits similar to those seen with COVID-19.
A detailed report by scientist Harald Brüssow, published last August in the journal Microbial Biotechnology, suggested plausible scenarios in which elevated levels of COVID-19 deaths could last five years or even longer. The 1889 pandemic hit England and Wales in 1890, and deaths remained high through 1892. Deaths declined over the next two years but still remained “substantially higher than in the pre-pandemic period.”
“From these data, one might deduce a protracted five-year course for a COVID-19-like pandemic, suggesting that COVID-19 might occupy us well beyond 2022 if the current vaccination campaigns does not change its ‘natural’ trajectory,” Brüssow wrote.
Still, the author added, “it is by no means clear whether an epidemic with similar basic characteristics will be a replay of one which occurred 140 years ago.” There are a number of differences between that pandemic and the one caused by COVID-19; such as the lack of use of masks during the 1889 pandemic, the lack of quarantine measures and the unavailability of vaccines.
Our species lived through the Spanish flu, polio, ebola, SARS, and swine flu. How have humans gotten themselves out of pandemics in the past? And how might we get out of this one?
Growing optimism
Health officials are optimistic that drugs like Paxlovid will reduce the risk of severe illness and death from COVID-19. But there is a severe shortage of those drugs — one reason why health officials in some California counties, including L.A. County, are retaining local indoor mask orders until case rates drop further, likely for a few more weeks.
It’s possible the virus could still mutate into something potentially worse, overriding immunity provided by vaccines or past infection, Topol said.
That’s why it’s so important to be ready for a worst case scenario, such as being able to meticulously monitor new surges, ramp up wastewater tracking of the virus, improve air filtration and work on a variant-proof vaccine, Topol wrote.
Potential new variants are a big reason why it’s essential that people get vaccinated and boosted, thereby reducing the chances of yet a new mutant strain developing. The U.S. ranks 67th in the world in a comparison of the share of its residents who are considered fully vaccinated, Topol wrote, citing data compiled by the Financial Times, behind countries including Sri Lanka, Colombia, El Salvador, Iran and Mongolia.
“Around the world, there are billions of people unvaccinated and likely without any protection from prior infection,” Topol said. “When the virus is not contained, as is the case in the world now, its spread creates the potential for new variants.”
Moving forward in California
Meanwhile, California is heading back toward a greater degree of normality as the Omicron surge eases. The L.A. Unified School District this week began allowing students to be maskless outdoors on campus for the first time since in-person schooling resumed 10 months ago.
UC San Francisco is on track to allow more staff, faculty and students to work on-site starting Tuesday. The campus is retaining a universal indoor mask mandate, except for people alone in an office or in a vehicle or while eating or drinking, Chancellor Sam Hawgood said in a town hall on Friday.
“We thought long and hard about the return-to-work date. We think it’s safe. The predictions are suggesting that there will be very little community transmission,” Hawgood said, assisted by high vaccination rates, and by the 10-campus UC system’s requirement that all eligible students and staff provide proof that they have received a COVID-19 booster shot.
Daily counts of new coronavirus cases are falling rapidly in California and the U.S., but progress is not even, “and we’ve not quite turned the corner yet on deaths in California,” Rutherford said at Friday’s campus town hall meeting.
Ahead of the holiday weekend, California reported an average of more than 200 COVID-19 deaths a day, the highest rate in 11 months, according to The Times’ COVID-19 tracker.
Nationwide, daily cases on a per capita basis are still quite high in places like Florida — especially in the state’s Panhandle region, southern Texas, the Appalachians, in some parts of the Rocky Mountains, Rutherford said.
In California, transmission levels remain high, according to criteria set by the U.S. Centers for Disease Control and Prevention but have still fallen significantly. Between Feb. 11 and Feb. 17 — the most recent weekly period not affected by lags in reporting related to the holiday weekend — California was averaging about 14,000 new cases a day; during the Omicron peak in early January, it was about 123,000 cases a day.
The latest number is close to the peak of the troubling summer Delta wave, which maxed out at around 15,000 cases a day in California.
California sees regional differences
The San Joaquin Valley and rural Northern California are still seeing higher case rates than other parts of the state. According to a Times analysis, the San Joaquin Valley has a case rate more than 40% higher than Southern California’s, while rural Northern California’s rate is 33% worse.
“So while things are getting better, we really haven’t come all the way back yet,” Rutherford said.
Experts are still closely watching a sublineage of the Omicron variant known as BA.2, which is probably somewhat more transmissible than the main Omicron sublineage, BA.1, with a preliminary report saying it may cause somewhat more severe disease, Rutherford said. But BA.2 accounts for a relatively small fraction of analyzed virus cases worldwide.
“At this moment, it does not look like BA.2 poses a threat as a major new variant, but it would not be surprising if we see another variant in future months that deserves a separate Greek letter designation,” Topol wrote.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.