Surprised that black people have a higher risk of death from COVID-19? I’m not
- Share via
At age 26, recently engaged and about to start my first grown-up managerial position in city government, I was handed a hefty report summarizing the results of my “comprehensive executive health assessment,” an onboarding requirement for all the city’s newly hired managers. The process had included an extensive physical examination, a lengthy written questionnaire, and an hourlong in-person interview with a nerdy, non-smiling white guy who took detailed notes on my diet, lifestyle and mental health.
I relaxed immediately when I saw I had received an overall rating of “excellent health.” Then I turned to the last page of the report and read some alarming news. If I were to die in the next year, the report informed me, the likeliest cause of death would be homicide.
The next day, my first call was to Mr. Non- Smiley.
“Hey, I got my health assessment,” I began, trying to sound managerial and calm while feeling anything but, “and I have a few questions. Since I was found to be in excellent health, I was a little surprised to learn about my risk of being murdered. Do you know something I don’t know?”
“Well, first, Miss Belk, let me just say we are very objective,” he replied in a dry monotone. “It’s all about data and the model.”
“OK, so why did the model conclude that I’m at risk of being killed?”
“You’re an otherwise healthy African American woman between the ages of 21 and 30. The data show that if you were going to die today, it would likely be the result of a homicide.”
“So, what’s that about? My age, my race, my gender?”
“Oh, race by far,” he said quickly. “If you were white, it would likely be some type of accident. Car, probably.”
The “it” part — the likely cause of death; in my case, homicide — jarred me. Silence. Mr. Non-Smiley, breaking the silence, and finally showing a little compassion in his own awkward way.
“You know, Miss Belk, it’s only data. Besides, once you make it to your 30s, heart disease, stroke and cancer kick in as key data points.”
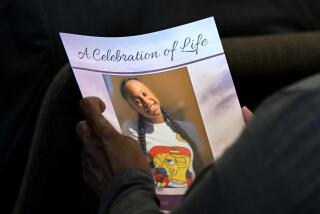
I did make it to 30. But my big sister, Vickie, and cousin Darryl didn’t. They both were murdered, victims of gun violence in their 20s.
Neither of us knew it at the time, but Mr. Non-Smiley had given me my first lesson in what public health professionals call “the social determinants of health,” a fancy way of saying that your income, ZIP Code and race can and often do determine your health, longevity and even your cause of your death.
What I know now is that the long history of racial discrimination in our country has led not only to economic disparities but to poorer health outcomes for black people.
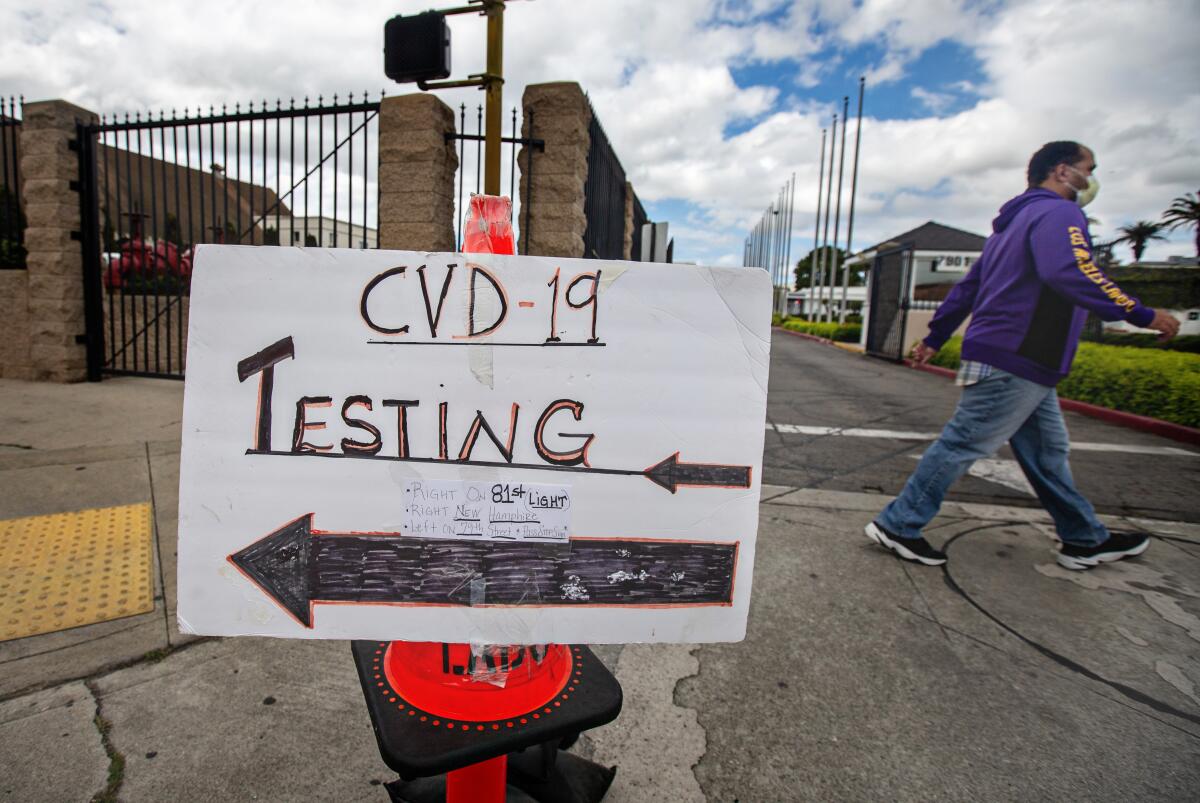
Consider what’s happening right now with the coronavirus. In cities across the country, COVID-19 is disproportionately affecting black and brown communities. In Louisiana, black people account for 32% of the population but 56% of the COVID-19 deaths. In Chicago, black people account for about 55% of the deaths, but only about a third of the population. Americans have lived with this kind of data for a long time, on disease after disease. It’s about time we did some new modeling where racial equity is front and center.
My husband is a physician, and I have spent much of my career working to improve health and wellness and advance racial equity. But that doesn’t make us immune from health disparities and the assumptions that underlie them.
A few years ago, my husband and I were meeting with our financial advisor, a well-meaning white man consumed, as Mr. Smiley had been many years earlier, by data and modeling. He didn’t like what he saw in our retirement planning numbers. He was concerned we wouldn’t have enough money if we both lived to the age his actuary modeling team had calculated for us.
I was feeling a little ornery.
“Did you factor in race?”
My husband just shook his head, hoping I would shut up. He finds it useless to engage in discussions regarding race with most white people.
“What do you mean?” the advisor asked, looking genuinely perplexed.
“Black folks don’t live as long as white people. Our life expectancy is a lot shorter. Go back to the people who do your modeling and tell them to factor in that we’re black.”
By now I was looking at a bemused black husband who knew I was right and a very uncomfortable white man who thought I was crazy.
“Our modeling is pretty solid, but I can tell this is important to you, so I’ll check and get back to you,” he agreed.
He got back to me a week later, and it was a short conversation.
“Uh, Judy, we ran those numbers again. The good news is you and Roger will be just fine. Based on our new calculations, you’ll have enough money to last.”
I couldn’t help but laugh. “So, they factored in our race, huh?”
“Yeah, they did. But I’m still going to manage your portfolio with the expectation you and Roger will be around for many, many years. After all, it’s just data.”
Judy Belk frequently writes about family, race and community. She is president and CEO of the California Wellness Foundation.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.