Coronavirus Today: A recipe for disaster?
- Share via
Good evening. I’m Karen Kaplan, and it’s Tuesday, Aug. 17. Here’s the latest on what’s happening with the coronavirus in California and beyond.
If you’ve been following the news, you already know there are plenty of reasons to be worried about the Delta variant. It replicates far more quickly than its predecessors, which means it takes less time to spread from one newly infected host to another. Even people who are fully vaccinated are transmitting the virus before their immune systems have a chance to knock it back.
In early May, when Delta accounted for less than 2% of all infections across the United States, weekly cases were below 300,00 and falling. Today, nearly 99% of U.S. infections are due to Delta, and weekly cases are nearing 900,000 and climbing — even though the proportion of Americans fully vaccinated against COVID-19 increased from about one-third to one-half during that time.
Not scary enough for you? You can thank my colleague Melissa Healy for laying out the true nightmare scenario a more dangerous coronavirus variant could pose.
Unfortunately, this scenario sounds a lot like the situation we’re currently in.
There are multiple factors that encourage the evolution of a vaccine-resistant viral strain. They include:
About half of the country is fully vaccinated — and half is not
If there were no COVID-19 vaccines in the picture, the coronavirus would have no evolutionary reason to develop resistance to them. Sure, random mutations might arise that would be helpful for evading vaccines, but without an actual vaccine to go up against, those mutations wouldn’t give them any competitive advantage, so there’d be no reason for them to spread.
On the other hand, if vaccination rates were high enough to achieve herd immunity, the coronavirus would be having trouble finding people to infect. Without new hosts to spread to, the virus would be deprived of chances to replicate, and if it’s not copying itself, it’s not generating new mutations that could help it dodge our vaccines.
Unfortunately, the United States is right in the middle of these two scenarios. That means we’re providing the virus with both the motive and the opportunity to evolve in ways that create vaccine-resistant variants. And the longer we are stuck in this middle ground, the more chances the virus will get.
The Delta surge will create more superspreader events
It stands to reason that with the highly transmissible Delta variant spreading around the country, superspreader events are more likely. Those aren’t a problem simply because they accelerate an outbreak. Superspreader events are also essential for giving fledgling variants a foothold in the community.
Models of coronavirus transmission demonstrate their importance. If a new variant doesn’t get a superspreading boost in the weeks following its birth, it’s likely to die on the vine. But if that variant can spread to just five additional people, it will gain enough momentum to stay in the game. And if it can spread to 20 people or more in a single event, it could be well on its way to dominating its community.
We’ve got the surge. We’ve got plenty of places for large groups of people to gather — many of them unvaccinated and not wearing masks. If superspreader events inevitably follow, all that will be missing is the vaccine-resistant variant. (See above.)
Kids are going back to school
A surge in coronavirus infections tied to school reopenings “can’t not happen,” warns Dr. Gregory Poland, a vaccinologist at the Mayo Clinic.
The vaccination rate for teens is even lower than it is for adults. According to the Centers for Disease Control and Prevention, 42.9% of 16- and 17-year-olds are fully vaccinated, as are 32.4% of adolescents ages 12 to 15. And kids younger than 12 aren’t even eligible for COVID-19 vaccines.
Nevertheless, kids are returning to classrooms by the tens of millions. In California, masks are required on campus, but mask mandates don’t apply nationwide. (Let’s pause for a shoutout to the school districts in other states that are requiring masks in defiance of their governors’ orders.) If kids become infected at school, they’ll bring the virus home to their families.
Before Delta, kids didn’t play a key role in the coronavirus spread. But that may be changing. Nearly 94,000 cases involving children were tallied during the week that ended Aug. 5, according to the American Academy of Pediatrics. Nationwide, the number of kids who were hospitalized with COVID-19 hit 239 in the week that ended Aug. 9. It may not sound like a lot in a country as big as the U.S., but it’s more than any previous point in the pandemic — and nearly 30% higher than it was the week before.
Vaccine protection is waning
Like everything else regarding the coronavirus, the length of time that COVID-19 vaccines remain effective is something we’re learning as we go along. But scientists do expect their effectiveness to wane sooner or later.
Pfizer and BioNTech, who produced the first COVID-19 vaccine to receive emergency use authorization in the U.S., said late last month that the efficacy of their shots slipped from 95% to 84% after six months.
U.S. health officials have been monitoring breakthrough cases involving healthcare workers, who were the first to start receiving the shots in December. They’ve been looking OK so far, but preliminary studies from Israel suggest the vaccine has lost some effectiveness at preventing serious cases of COVID-19 among people who were vaccinated in January.
Federal health officials are expected to advise all Americans to get COVID-19 booster shots eight months after their last dose. That recommendation could come later this week. So far, only people with weakened immune systems are eligible for boosters.
That would address the problem of the vaccines wearing off, but we’re still vulnerable on the other three counts.
And that’s not even considering the fact that the approaching winter will force more people indoors, where they’ll be clustered into cooler, drier environments that are more conducive to coronavirus spread.
And there’s more. I highly recommend giving Healy’s story a read.
By the numbers
California cases, deaths and vaccinations as of 7:25 p.m. Tuesday:
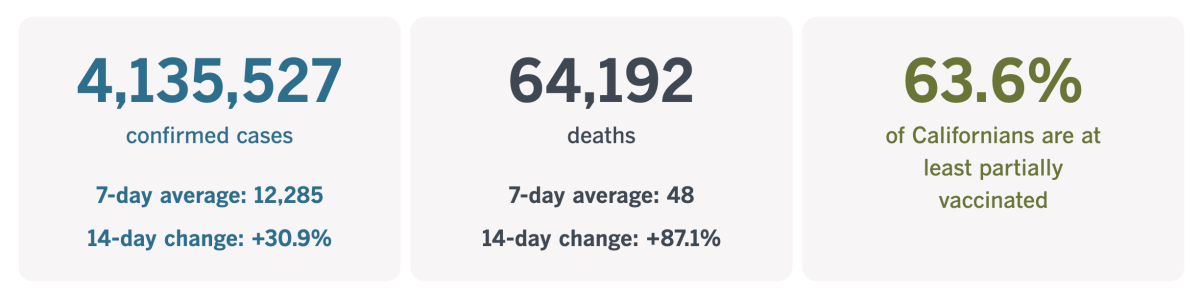
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
How to compensate people injured by COVID-19 vaccines
Maybe you’ve heard of the vaccine court. That’s the colloquial name for the National Vaccine Injury Compensation Program, a federal system set up to reimburse people who are harmed by the routine childhood immunizations that are required for school entry.
Cases of vaccine-related harm are exceedingly rare, but lawsuits making such claims were becoming enough of a problem in the 1980s that vaccine makers were at risk of walking away from the business. In an effort to stop that from happening — and averting a resurgence in vaccine-preventable diseases — Congress created the vaccine court to make those lawsuits go away.
In the 35 years since, more than 8,000 families have received in excess of $4 billion to compensate them for the effects of severe allergic reactions, a type of brain swelling called encephalopathy, an intestinal problem called intussusception or other serious problems.
The vaccine court covers injuries stemming from vaccines for diphtheria, tetanus, pertussis, measles, mumps, rubella, polio and a host of others. But it does not cover COVID-19 vaccines.
Rep. Lloyd Doggett, a Democrat from Texas, hopes to change that. He and Rep. Fred Upton, a Republican from Michigan, have introduced a bill that would update the vaccine court in a variety of ways. That includes making it available to people who are injured by COVID-19 vaccines, a spokesperson for Doggett said.
In the meantime, people with COVID-related claims are advised to go to the Countermeasures Injury Compensation Program. Although COVID-19 is listed as one of the ailments covered by this program — along with Ebola, Zika and smallpox, to name a few — it has yet to pay a single cent to anyone hurt by a COVID-19 vaccine.
Generally speaking, the CICP system is more daunting than the vaccine court. Decisions are made by administrative fiat instead of judges; it has only seven staffers and contractors; and it doesn’t reimburse fees for lawyers who help victims bring claims.
On top of that, the evidence required to prove an injury is harder to pin down. Experts say it must be backed up by solid scientific and medical evidence, a burden of proof that’s all but impossible to meet since the vaccines are so new.
But the victims need help now — people like Angela Marie Wulbrecht, a previously healthy nurse of 23 years who drove three hours to get a shot of the Moderna vaccine in January.
Twelve minutes after her injection, her heartbeat was racing and her blood pressure was soaring. In the months since, she has contended with severe fatigue, brain fog, balance problems and other symptoms. She’s spent about $35,000 of her own money on medical bills, including five trips in an ambulance.
“I wanted to get vaccinated as soon as I could to help fight the pandemic,” Wulbrecht told our friends at Kaiser Health News. “But it would help those who are hesitant if they took care of those of us who got injured.”
Katharine Van Tassel, a vaccine law expert at the Case Western Reserve University School of Law in Cleveland, agreed. Cases like Wulbrecht’s are rare, but “if you’re going to take one for the team, the team has to have your back,” she said. “That’s a moral imperative.”
Despite her own problems, Wulbrecht still backs the COVID-19 shots. Her husband was vaccinated, and her 12-year-old daughter Gabriella is scheduled to get her first dose on Wednesday.
California’s vaccination progress
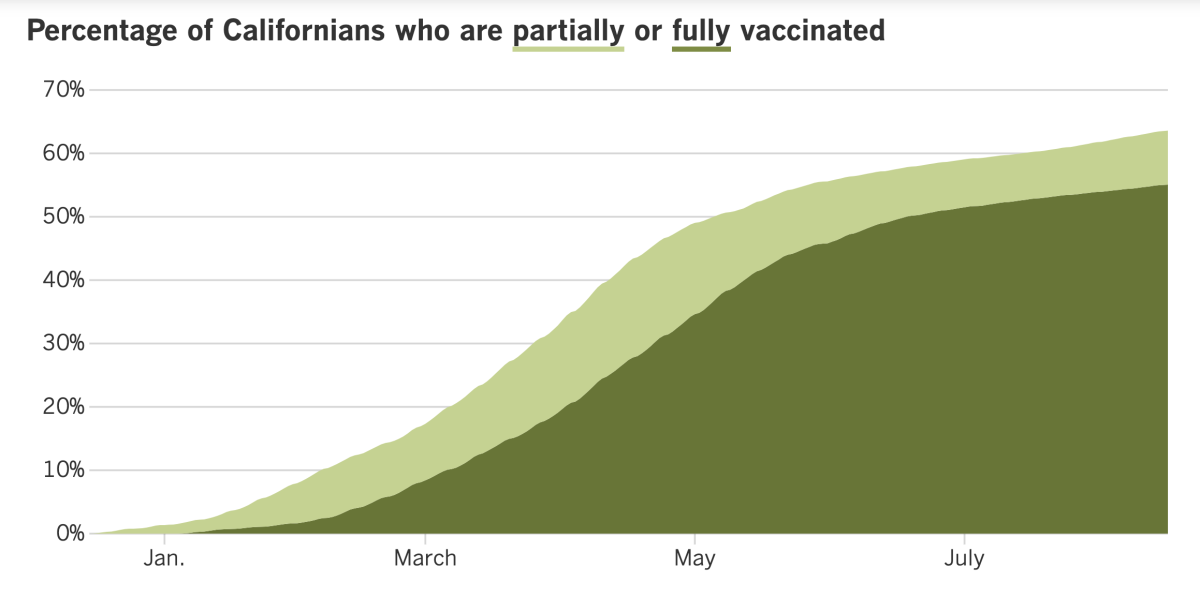
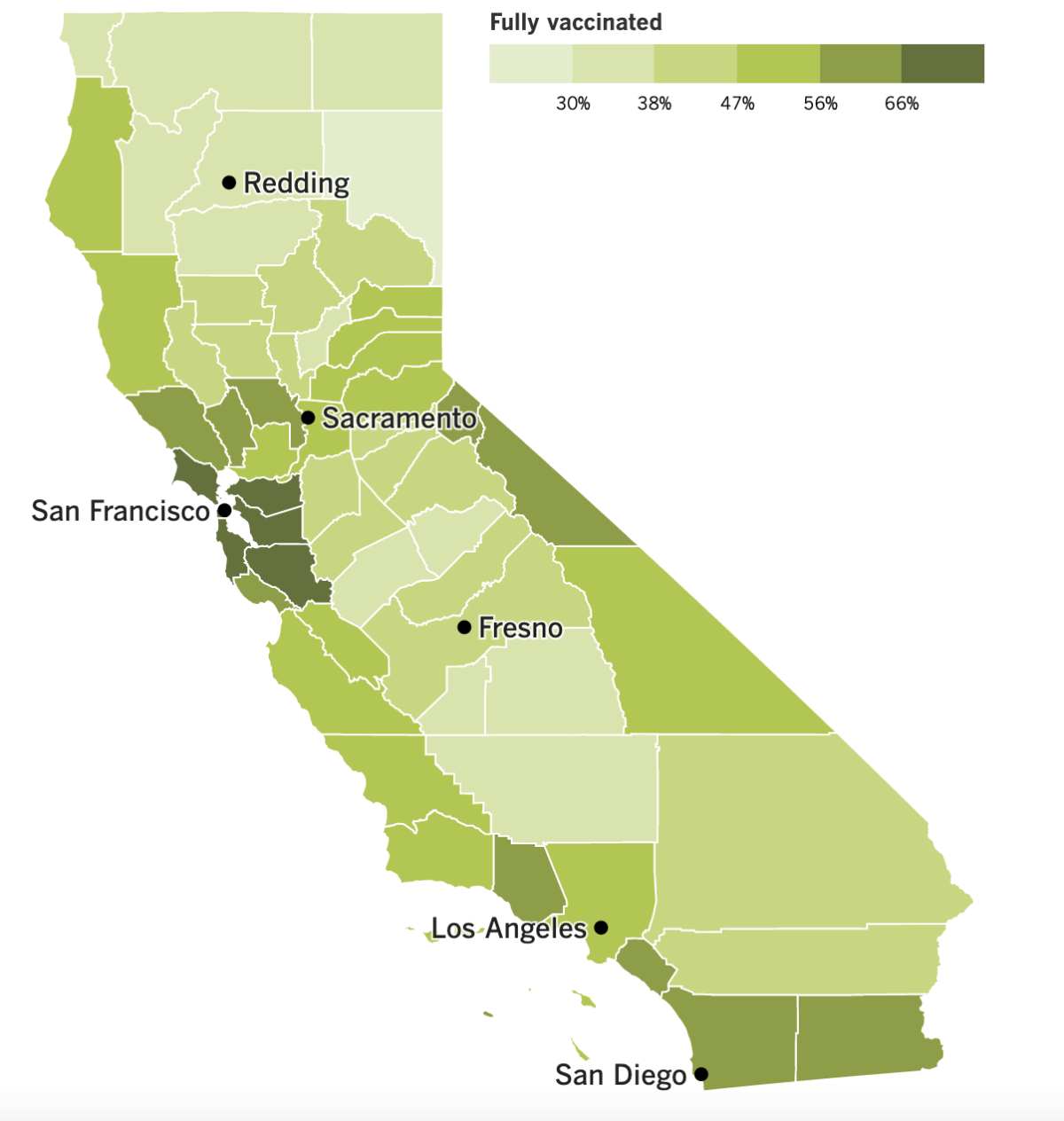
See the latest on California’s vaccination progress with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
In other news ...
Congratulations, California: You’re flattening the curve.
The Golden State is now reporting about 11,800 new coronavirus cases per day over the last week. Though that’s up 7% from the previous week, the rate of growth is considerably slower than in the previous week, when daily cases increased by 30%. In early July, the week-over-week growth was 86%.
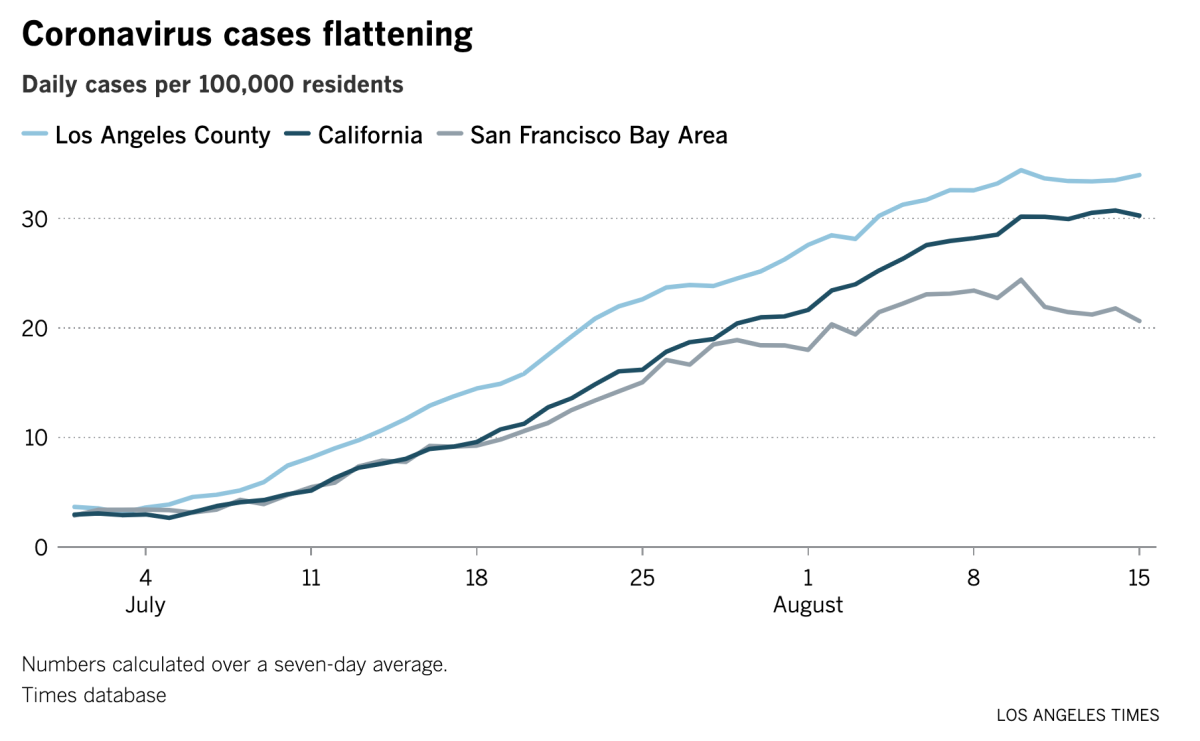
Hospitalizations are slowing too. As of Sunday, there were 7,166 people with COVID-19 in California hospitals, up 20% from the prior week. But in late July, the number of statewide hospitalizations was growing by 50% week-to-week.
Epidemiologists and infectious disease experts say we have our better-than-average vaccination rate to thank, along with local rules recommendations for wearing masks indoors, even if we’re fully vaccinated. But they also caution that it’s too soon to say the worst of the current surge is over.
“The key here is to recognize we probably are turning the corner, that we can’t just let down our guard so quickly, but we should still feel comforted, said UC San Francisco epidemiologist Dr. Kirsten Bibbins-Domingo.
L.A. County isn’t letting its guard down. Indeed, health officials here have upped the ante with a new health order requiring face coverings for people attending concerts, baseball games and other large outdoor events that draw more than 10,000 people. The face coverings can be removed only briefly to eat or drink.
The order will apply to everyone, regardless of their COVID-19 vaccination status. It goes into effect at 11:59 p.m. on Thursday.
Students in the Los Angeles Unified School District began a new school year Monday, returning en masse to their campuses for the first time since March of 2020. Thousands of them faced long waits to get to their classrooms though, due to the failure of the district’s health screening system.
The “Daily Pass” system was unable to keep up with demand and process all the required health checks. Some students were delayed for 30 minutes; some waited more than an hour.
The system asks students or their parents to log on to a district website before school to answer questions about whether students are experiencing a cough, fever or fatigue. Only if they are feeling well will they receive a scannable code to come on campus that day. The irony was that the online system was meant to save time by allowing students to bypass an in-person health screening.
The new system appeared to be running as intended on Tuesday.
LAUSD prepared for its first day of school by administering coronavirus tests to students over the past two weeks, an effort to establish a baseline of infections. The results of that testing were announced Tuesday: 8 in 1,000 students tested positive, as did 6 in 1,000 staffers.
The actual number of student infections totaled 3,255, out of more than 450,000 students. Ominously, the infection rate has been creeping up since summer school ended on July 23. About 44,000 students were tested during each week of summer school, and the test positivity rate rose steadily during that time.
Amid early signs that the protection offered by COVID-19 vaccines is waning, federal health officials appear poised to recommend booster shots to the general vaccinated public.
Just last week, officials advised people with weakened immune systems — such as transplant recipients and cancer patients — to get a booster. The new action would make anyone eligible eight months after they’ve received their second dose.
Healthcare workers and nursing home residents were the first to get vaccinated, and their second doses occurred as early as mid-January. That means they’ll start hitting the eight-month mark in mid-September.
The plan, which hasn’t been announced but was described by people speaking on the condition of anonymity, calls for the third doses to be dispensed after the Food and Drug Administration grants full approval to the Pfizer-BioNTech, something that’s expected to occur in the coming weeks.
Data from Israel have some experts concerned that the potency of the vaccines is waning too quickly to keep up with Delta. One study found that the Pfizer vaccine’s effectiveness peaked at 96% two months after the second dose; four months later, it was down to 90%, and by six months it had dropped to about 84%.
Texas Gov. Greg Abbott might wish he’d gotten a booster shot. He tested positive for a coronavirus infection on Tuesday, despite having been vaccinated in 2020.
Abbott’s office said he is in good health and experiencing no COVID-19 symptoms. He is isolating in the governor’s mansion and receiving monoclonal antibody treatment.
The positive test result came the day after Abbott tweeted a picture of himself speaking to a group of Republicans at an indoor event in Dallas. The governor, a staunch opponent of mask mandates, wasn’t wearing a face covering, nor were most members of the audience.
Meanwhile, New York City will implement a vaccine mandate tomorrow, making the shots required for patrons of gyms, museums, restaurant dining rooms and other venues. And New York state ordered workers in hospitals and nursing homes to get inoculated if they want to keep their jobs.
Finally, you may recall my amazement last week that Australia’s capital city of Canberra went into a one-week lockdown in response to a single confirmed coronavirus infection. Now they’ve been one-upped by New Zealand.
The entire country was locked down Tuesday after one Auckland resident was found to have a community-acquired infection. Both Auckland and Coromandel, a town the infected man visited, will remain shut down for a week. The rest of the country will be in lockdown for at least three days.
“We have seen what happens elsewhere if we fail to get on top of it,” Prime Minister Jacinda Ardern said in announcing the action. “We only get one chance.”
Your questions answered
Today’s question comes from readers who want to know: Are teachers and school staff members required to get vaccinated against COVID-19?
In some places, yes, but not everywhere.
In California, school employees are required to be vaccinated or subject themselves to regular testing. Gov. Gavin Newsom announced that policy last week and gave the state’s 1,000 or so public school districts, as well as private schools, until Oct. 15 to comply.
Some school districts already had rules like that on their books. And some districts have taken a more aggressive approach. The Los Angeles Unified School District implemented a vaccine mandate that requires all teachers and staff to be fully vaccinated by Oct. 15.
The nation’s top infectious disease expert, Dr. Anthony Fauci, said he’d like to see vaccine mandates for all teachers. So would Randi Weingarten, president of the American Federation of Teachers, as long as they were implemented with fairness and sensitivity.
K-12 students who are old enough to be eligible for COVID-19 vaccines are encouraged to get them but not required to do so.
Got more back-to-school questions? We’ve got you covered! Check out our comprehensive guide here.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

For some girls, the quinceañera is out and the dieciseis-añera is in.
Latina teens who missed out on the traditional coming-of-age rite for 15-year-olds are now catching up on the celebrations, at age 16. That’s keeping people like Celia Barrios, who runs a quinceañera planning business, on her toes.
Before the pandemic, Barrios was organizing three events a week. Now she’s getting up to 30 calls a week, and her calendar is booked into 2023.
“I am booked back to back and loving it,” she said. “It’s such a special event for our culture.”
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




