FDA OKs Pfizer vaccine, opening new front against COVID-19; shots to begin within days

- Share via
Opening a new front in America’s battle against the coronavirus, the U.S. Food and Drug Administration authorized emergency use of the COVID-19 vaccine developed by Pfizer Inc. and BioNTech, clearing the way for widespread immunizations to begin.
The authorization came one day after an FDA scientific advisory panel endorsed the two-dose vaccine, which was 95% effective in clinical trials and easily surpassed the agency’s requirements for both safety and efficacy for use by people 16 and older.
For the record:
2:22 p.m. Dec. 12, 2020A previous version of this article reported that 162 people who received the vaccine during Phase 3 clinical trials developed COVID-19. Those trial participants had received the placebo.
“It is nothing short of a medical miracle to have FDA authorization of a vaccine for COVID-19 just over 11 months since the virus was made known to the world,” Health and Human Services Secretary Alex Azar said in announcing the decision Friday night.
Dr. Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, said he was blown away by the fact that the coronavirus genome was first sequenced in January and now the country will have “a vaccine in somebody’s arm in less than a year.”
“It would have been inconceivable to me a year or two or three ago,” he said.
The official nod from regulators allows states and territories to place orders for the vaccine through a tracking system maintained by the Centers for Disease Control and Prevention. State and local health officials will be responsible for delivering the shots to healthcare workers and other priority access groups.
Pfizer officials have said it would take only a few days to deliver millions of doses of the vaccine to points across the U.S., including 327,000 to California. The company said it can produce as many as 50 million doses by the end of the year.
Scientists, health officials and a beleaguered public all hope the arrival of the first vaccine will mark the beginning of the end of the pandemic, which has infected nearly 16 million Americans and killed almost 295,000. Indeed, on a single day this week, more Americans died of COVID-19 than were killed on 9/11 or D-day.
For months, public health leaders have maintained that the surest way back to a life in which children go to school, adults to go work and friends and family greet one another with hugs and kisses is a vaccine. If roughly 70% of the country is vaccinated, the resulting “herd immunity” will deprive the coronavirus of easy avenues to spread and the outbreak will peter out.
Friday’s decision is the first step in that process.
The FDA’s emergency use authorization will kick off “the most ambitious vaccine campaign in human history,” said Dr. George Daley, dean of Harvard Medical School. But he cautioned that it will be a long haul.
“Vaccines will not offer an overnight solution,” Daley said. “We need to brace ourselves for many more months of infection prevention and distancing measures as the vaccines are rolled out.”
The first COVID-19 vaccine could arrive in California this week. Here is how officials plan to handle the first wave of vaccinations.
In Phase 3 clinical trials involving more than 43,000 volunteers, the Pfizer vaccine consistently reduced the risk of developing COVID-19. It was 94% effective for people 55 and older. It was 95% effective for people with an underlying medical condition that made them more likely to have a serious case of COVID-19. It was 96% effective for people who were obese.
Likewise, the vaccine was 94.5% effective for Latinos, 94.7% effective for non-Latinos and 100% effective for Black clinical trial participants.
The volunteers were tracked for a median of two months after receiving their second dose of either the vaccine or a saline placebo. Of the 170 cases of COVID-19 that developed during that time, 162 involved people who were randomly assigned to receive the placebo. Only eight people who got the vaccine became ill.
No serious adverse events were reported. The most common side effects were fatigue, headache, muscle pain and chills, along with short-term pain at the injection site in the upper arm.
Both Pfizer and the federal government will continue to monitor study participants long-term to watch for other problems and to see how long the vaccine’s protection lasts.
Food and Drug Administration commissioner Stephen Hahn answered questions from The Times about how the agency is reviewing COVID-19 vaccines. “When appropriate, I’ll be first in line,” he told The Times.
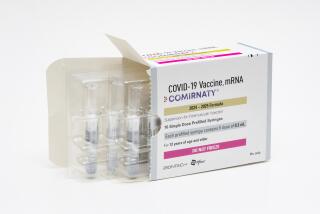
The vaccine, known as BNT162b2, breaks new ground in more ways than one. Not only is it the first COVID-19 vaccine to be authorized by the FDA, it’s the first mRNA vaccine for any disease to pass muster with U.S. regulators.
Rather than using a weakened or killed piece of the coronavirus to prompt an immune response, the Pfizer-BioNTech vaccine relies on a piece of the coronavirus’ genetic code called messenger RNA. That mRNA instructs the muscle cells in the upper arm to create the infamous “spike” proteins that give the virus its crown-like appearance. The immune system responds by creating antibodies that can swing into action in the event of an actual infection.
The antibodies are durable, but the mRNA is not. The fragile material breaks down quickly, lasting only a day and a half in the body, said Dr. Bruce Walker, an immunology and infectious diseases researcher at Harvard and MIT.
To keep it intact until it can be injected, the vaccine must be kept in a deep freeze. It will be shipped in specialized refrigerated containers designed to maintain a temperature of minus-94 degrees Fahrenheit — colder than the coldest parts of Antarctica.
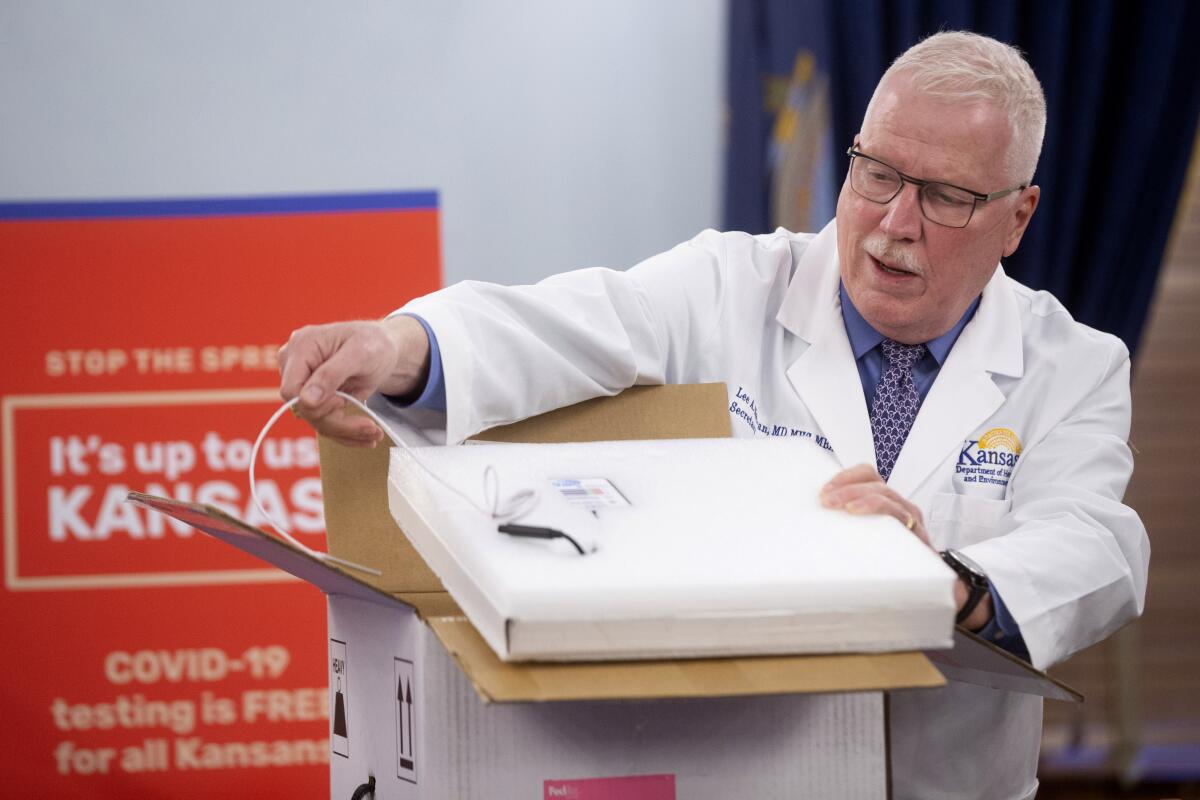
Both FedEx and UPS stand ready to transport the vaccine in packages filled with dry ice, each equipped with a sensor to continuously monitor the interior temperature. The packages are destined for 636 locations around the country, said Army Gen. Gus Perna, who is overseeing the rollout effort for Operation Warp Speed, the Trump administration initiative to accelerate the development and distribution of COVID-19 vaccines.
Syringes, swabs and other supplies needed to administer the vaccine were already on the move, Perna added.
Each state has developed its own distribution plan in consultation with the CDC. Most states have designated healthcare workers and residents of nursing homes and other long-term care facilities as their top priorities for the first wave of vaccinations, in line with guidance from the CDC’s Advisory Committee on Immunization Practices.
State leaders, in turn, have identified regional hospitals and medical centers to administer vaccine to healthcare workers. And pharmacy giants CVS and Walgreens have signed agreements with the federal government to operate vaccine clinics at more than 50,000 long-term care facilities around the country.
Perna said 2.9 million doses of Pfizer vaccine will go out in the first shipments, with states receiving amounts proportionate with their populations. An additional 2.9 million doses are being held back so they can be sent out in 21 days for people to receive the required second dose, and 500,000 doses will be kept in reserve in case of unforeseen circumstances, he said.
The Pfizer vaccine could soon be joined by another mRNA vaccine from Moderna Inc. and the National Institutes of Health. It was nearly 95% effective in Phase 3 clinical trials, and the FDA scientific advisory panel is scheduled to consider it Thursday.
Trump administration officials say they expect 20 million people will receive their first dose of vaccine by the end of the year. Every American who wants a COVID-19 vaccine should be able to get it by the end of June, Azar said.
Ultimately, health experts expect the FDA to approve multiple types of COVID-19 vaccines. That would boost the supply of shots needed to vaccinate about 70% of the population and achieve herd immunity.
But other obstacles stand in the way. State officials say they are woefully short of funds needed to carry out their vaccination programs. Although they’ve requested more than $8.4 billion, they have received only about $200 million, said Katie Greene, a visiting policy associate at the Duke-Margolis Center for Health Policy.
And even if the supply side is squared away, there may be problems with demand. A poll conducted by the Associated Press-NORC Center for Public Affairs Research in early December found that only 47% of U.S. adults said they planned to take a COVID-19 vaccine when it became available; 26% said they would decline it, with the remaining 27% unsure.
Fauci said he recognized that many skeptical Americans would need to be persuaded to trust the vaccines, especially considering how quickly they were developed and vetted. He said he’ll do his part by getting getting vaccinated on camera.
“Definitely I will get vaccinated, and I will get vaccinated publicly,” he said.
Times staff writer Noam N. Levey in Washington contributed to this report.