Invasive Lobular Carcinoma: Why It Deserves More Focus

- Share via
Key Facts
- ILC makes up 10–15% of all invasive breast cancers but often goes underdiagnosed due to its diffuse growth pattern.
- The hallmark of ILC is the loss of E-cadherin, leading to its characteristic single-file cell arrangement.
- Genomic tools like the 21-gene recurrence score help personalize chemotherapy decisions in ILC.
- Chemotherapy may offer survival benefits to node-positive ILC patients with high RS scores.
- ILC-specific trials and personalized treatment strategies are critical to improving patient outcomes.
Invasive Lobular Carcinoma (ILC) is the second most common type of invasive breast cancer, accounting for about 10-15% of all invasive cases. Of all breast cancers, ILC is notable for its frequency and biological differences which make it distinct from others.
Invasive Lobular Carcinoma, while related to the more prevalent Carcinomas, exhibits distinct characteristics in its growth, diagnosis, and response to treatment.
Ongoing breast cancer research continues to enhance the understanding of ILC’s biological mechanisms, its variations across subtypes, and the optimization of treatment strategies. However, current clinical knowledge and the development of targeted therapies for ILC still present areas for improvement.
Table of Contents
- Pathology and Characteristics
- Treatment Options
- Treatment Results
- Challenges and Future Directions
- Closing Thoughts
- References
Pathology and Characteristics
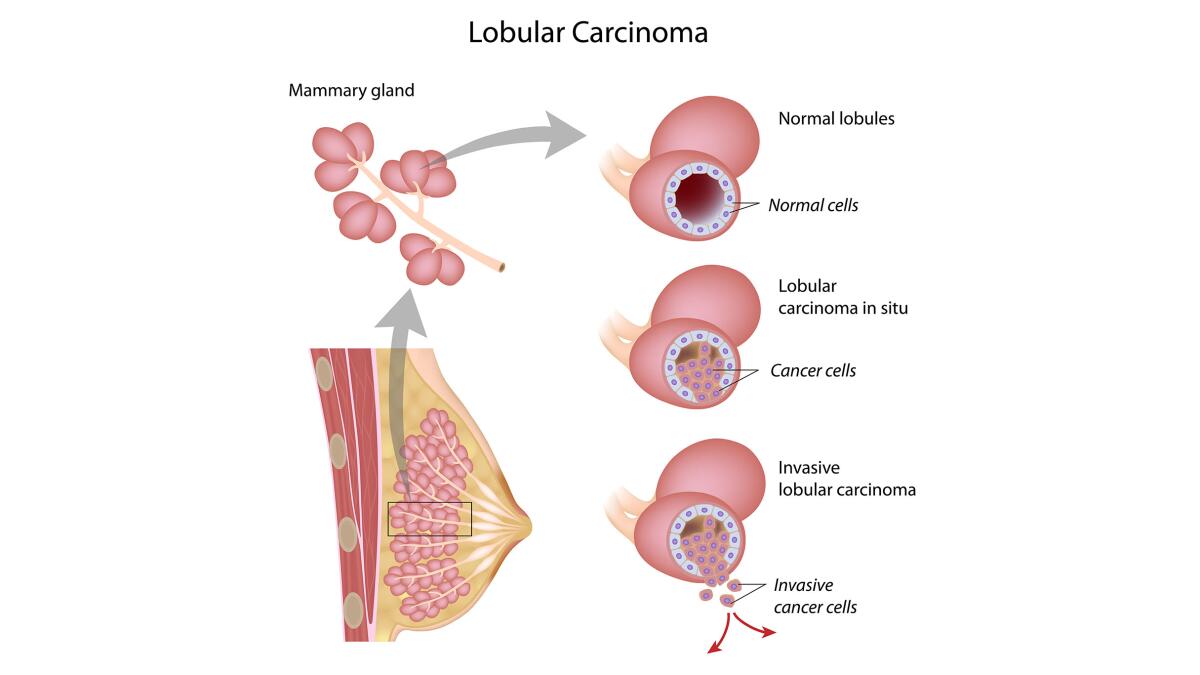
At the cellular level, ILC is defined by the loss of E-cadherin, a protein that helps cells stick together. ILC originates in the milk glands and spreads from these lobules. Without this molecule, ILC cells grow in single file lines rather than forming cohesive tumors like IDC [2], as IDC originates in the milk ducts.
This subtle and diffuse pattern makes it harder to detect on standard imaging tools like mammograms and ultrasounds. ILC begins in the terminal duct lobular units and the loss of E-cadherin is significant in its progression.
ILC is not a one size fits all diagnosis. It has several subtypes—classic, pleomorphic and solid—each with unique biological and clinical behaviors [4]. These variants can differ in how they look under the microscope, how aggressive they are and how they respond to treatment. More than 80% of ILC cases are hormone receptor positive, making estrogen and progesterone receptors significant markers in its characterization and treatment options.
One of the biggest challenges with ILC is that it often goes undetected until later stages. Because the tumor cells infiltrate the breast tissue without forming a lump, patients and doctors may miss early signs, delaying diagnosis and treatment.

Treatment Options
Although ILC behaves differently from IDC, they are often treated the same way—surgery, radiation, endocrine therapy and chemotherapy as needed [2]. But as we learn more about ILC, researchers are finding that a more tailored approach, considering hormone receptor status may lead to better results.
Hormone therapy is a treatment option for hormone receptor positive ILC, often used in combination with other therapies such as radiotherapy and chemotherapy.
One of the breakthroughs in this area is the use of genomic tools such as the 21-gene recurrence score (RS). This test determines whether a patient is likely to benefit from chemotherapy by evaluating the expression of 21 cancer related genes. While it was initially validated in IDC, it’s being used more and more to guide treatment decisions in ILC as well [1].
Breast conserving surgery is also an option for ILC patients, especially when neo-adjuvant therapies are used to shrink the tumor before surgery.
Interestingly, ILC patients with high RS scores are less likely to receive chemotherapy compared to IDC patients with similar risk profiles. This may be due to the uncertainties around how ILC responds to chemotherapy or differing opinions among oncologists. Plus new treatments emerging from clinical trials are showing promise in addressing the unique challenges of lobular carcinoma.
These genomic tests are influencing treatment options, helping to tailor therapies more precisely to the individual characteristics of the cancer.
Treatment Results
When it comes to results, ILC holds its own against IDC but there are nuances. Prognostic factors play a big role in treatment results for ILC patients. For patients with N1 ILC and high RS, chemotherapy does seem to offer a survival benefit. This is a key finding as it reinforces the value of using genomic tests to individualize care.
Early detection of ILC makes a big difference in survival rate, with localized cases having a 99% 5 year relative survival rate. But the survival rate declines as the stage of cancer progresses.
Also, researchers haven’t found significant differences in local recurrence, distant metastasis or overall survival between ILC subtypes [5]. So while subtypes may behave differently biologically, they don’t necessarily translate into different prognosis—at least with current treatment. If the cancer has spread into nearby tissue or lymph nodes, the prognosis is worse, highlighting the importance of staging in determining patient outcomes.
Challenges and Future Directions
ILC presents several clinical and research challenges.
Advanced Diagnosis: The subtle spread of ILC means it’s often found at later stages when treatment is more complex. Conventional imaging can miss ILC lesions, so there’s a need for advanced imaging and potential use of neoadjuvant therapies—treatments given before surgery to shrink tumors [3].
The challenges in detecting ILC mean we need to use multiple diagnostic tests beyond standard mammograms. MRI is particularly useful in producing internal images, helping to assess the size and extent of the tumor.
Conflicting Results: While some studies show ILC patients do as well as IDC patients, others show worse long term results. This may be due to underrepresentation of ILC in clinical trials or lack of treatment guidelines [5]. ILC is often diagnosed at an advanced stage, which complicates treatment, so early detection and specialized care is key.
Personalized Treatment: Given the heterogeneity of ILC, researchers are advocating for more personalized approaches. That means considering not only the subtype but also the molecular profile—factors that may one day lead to more effective, less toxic therapies.
Tailored ILC treatment is crucial due to the unique challenges of this rare cancer, requiring a multidisciplinary approach and ongoing research to improve outcomes.
There’s a growing consensus that ILC deserves the same research attention and funding as IDC. Dedicated clinical trials and precision medicine approaches could make a big difference in care for this overlooked breast cancer subtype.
Closing Thoughts
Invasive Lobular Carcinoma is a distinct yet under-recognized breast cancer, with research focusing on the behavior of breast cancer cells in this subtype. Its diffuse pathology, subtle imaging and varied treatment responses make it different from the more common IDC. Cancer cells are key to ILC progression and diagnostic and treatment decisions.
While traditional protocols have lumped them together, tools like the 21-gene recurrence score are helping clinicians make more personalized decisions for ILC patients. But there’s still work to be done, especially in early detection and outcome prediction.
The way forward requires ILC-specific trials, molecular research and diagnostic innovations so patients get care that matches their disease. Progress in general cancer research and treatment will help with the complexities of all cancers, including ILC.
References
[1] Weiser, R., Polychronopoulou, E., Hatch, S. S., Haque, W., Ghani, H. A., He, J., Kuo, Y. F., Gradishar, W. J., & Klimberg, V. S. (2022). Adjuvant chemotherapy in patients with invasive lobular carcinoma and use of the 21-gene recurrence score: A National Cancer Database analysis. Cancer, 128(9), 1738–1747. https://doi.org/10.1002/cncr.34127
[2] McCart Reed, A. E., Kalinowski, L., Simpson, P. T., & Lakhani, S. R. (2021). Invasive lobular carcinoma of the breast: the increasing importance of this special subtype. Breast cancer research : BCR, 23(1), 6. https://doi.org/10.1186/s13058-020-01384-6
[3] Thomas, M., Kelly, E. D., Abraham, J., & Kruse, M. (2019). Invasive lobular breast cancer: A review of pathogenesis, diagnosis, management, and future directions of early stage disease. Seminars in oncology, 46(2), 121–132. https://doi.org/10.1053/j.seminoncol.2019.03.002
[4] Bozkurt, E., Kaya, C., Ucak, R., Demircioglu, M. K., Guven, O., & Mihmanli, M. (2021). Invasive lobular carcinoma of the breast: clinicopathological features and patient outcomes. Annali italiani di chirurgia, 92, 494–499. https://pubmed.ncbi.nlm.nih.gov/34795114/
[5] Mouabbi, J. A., Hassan, A., Lim, B., Hortobagyi, G. N., Tripathy, D., & Layman, R. M. (2022). Invasive lobular carcinoma: an understudied emergent subtype of breast cancer. Breast cancer research and treatment, 193(2), 253–264. https://doi.org/10.1007/s10549-022-06572-w












