How Obstructive Sleep Apnea Treatment Is Evolving

- Share via
Key Facts
- OSA affects about 1 in 5 adults and increases the risk of heart disease and diabetes.
- Home sleep apnea tests (HSAT) offer accessible and cost-effective diagnosis.
- CPAP remains the gold standard, but many alternatives now exist for nonadherent patients.
- Precision medicine and phenotyping help tailor treatments to individual patient profiles.
- AI, telemedicine, and remote monitoring are reshaping how clinicians manage OSA.
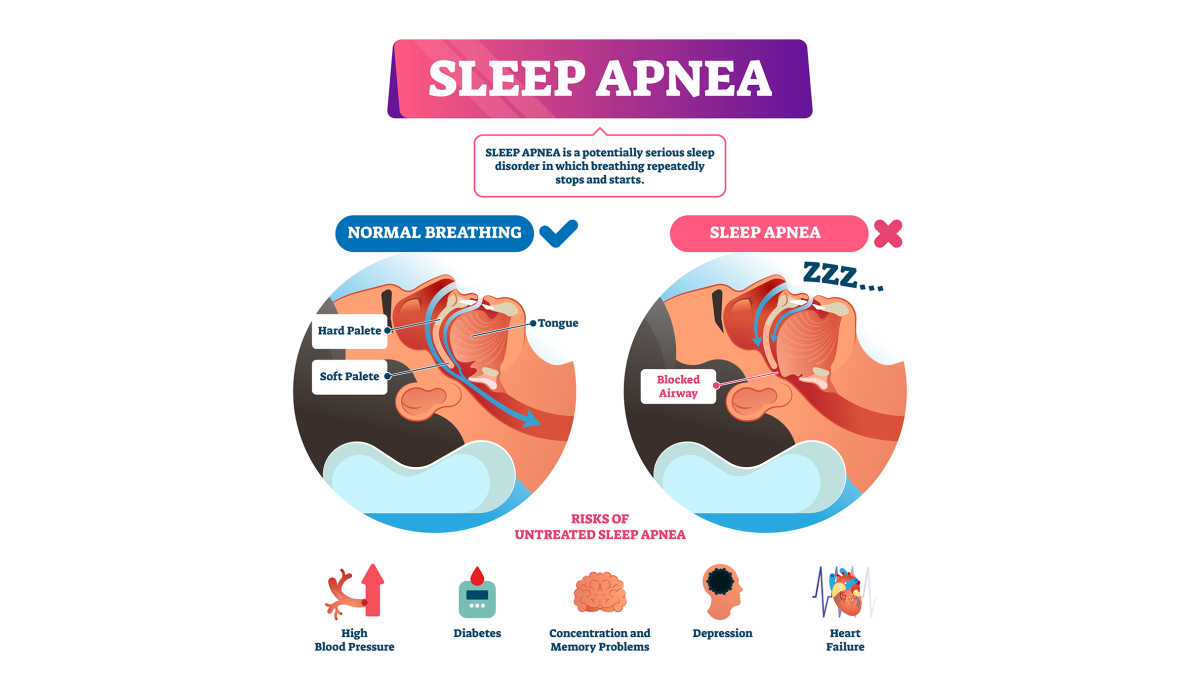
Obstructive Sleep Apnea (OSA) is a common and serious sleep disorder characterized by repeated episodes of upper airway obstruction during sleep. Symptoms of OSA include loud snoring, excessive daytime sleepiness and observed episodes where you stop breathing during sleep. Understanding your individual risk factors is key to diagnosis and management.
OSA affects 1 in 5 adults and contributes to cardiovascular disease, metabolic dysfunction and poor quality of life. Untreated OSA is associated with serious health problems like cardiovascular disease and can reduce life expectancy. With the growth of precision medicine, digital health and behavioral interventions OSA care is moving from one size fits all to personalized approaches.
Table of Contents
- Diagnostic Approaches: From Sleep Labs to Home Testing
- Treatment Foundations: PAP Therapy and Lifestyle Interventions
- Personalized Medicine and Phenotyping
- Telemedicine and Remote Monitoring
- Emerging Technologies: Machine Learning and AI
- Special Considerations: Positional OSA and Pediatric Applications
- Metabolic and Cardiovascular Connections
- Closing Thoughts
- References

Sleep Apnea Diagnosis: From Sleep Labs to Home Testing
Polysomnography (PSG) is the gold standard for diagnosing OSA especially in complex or high risk cases [4] [6]. A sleep study is done in a sleep center and reviewed by a sleep specialist to ensure accurate diagnosis. As part of the assessment a healthcare provider will review your medical history and bedtime routine to evaluate risk factors and sleep patterns.
The diagnosis process involves identifying symptoms of obstructive sleep such as loud snoring, daytime sleepiness and witnessed apneas. There are different types of sleep apnea including obstructive sleep apnea and central sleep apnea. Obstructive apneas and breathing pauses are key findings during a sleep study while central sleep apnea is when the brain fails to send signals to breathing muscles resulting in central sleep disruptions. Something like this is different from other sleep-related issues such as narcolepsy and insomnia.
But recent updates support the growing role of home sleep apnea testing (HSAT), especially for patients with high pretest probability and fewer comorbidities [1] [3]. These tests get obstructive sleep apnea diagnosed. Portable devices now offer reliable data while improving access and reducing costs.
The 2015 systematic review also highlighted the emerging value of biomarkers—like IL-6 and kallikrein-1—as potential tools for assessing OSA severity [12].
Treatment Foundations: PAP Therapy and Lifestyle Interventions
Continuous Positive Airway Pressure (CPAP) is the foundation of OSA treatment especially in moderate to severe cases. Many studies have shown its effectiveness in reducing apnea events, improving sleep quality and lowering cardiovascular risk [1] [4] [5]. CPAP and other interventions keep the airway open and get sleep apnea treated.
But adherence is a major challenge. Alternatives like oral appliances, positional therapy and upper airway surgery are effective in milder cases or when CPAP is poorly tolerated [3] [6] [8]. Surgery may be necessary for patients with severe symptoms or when other therapies fail. Severe sleep apnea and severe OSA may require more aggressive or combination therapies.
Lifestyle changes like weight loss, exercise and alcohol/tobacco cessation are foundational interventions that should be part of any treatment plan [1] [3]. These lifestyle changes are key to managing mild sleep apnea and mild obstructive sleep apnea.
A comprehensive approach is often needed to get obstructive sleep apnea treated and to treat OSA.
Personalized Medicine and Phenotyping
Not all OSA cases are the same. Advances in phenotyping—the classification of patients by symptom clusters, anatomy and comorbidities—are shaping precision medicine approaches [7] [9]. This has led to new algorithms for selecting ideal therapies based on individual traits rather than a one size fits all CPAP prescription.
A 2025 phenotype-based study showed how different comorbidity profiles may predict which patients need early referral and treatment escalation [9].
Telemedicine and Remote Monitoring
The COVID-19 pandemic accelerated the adoption of telemedicine and sleep medicine was no exception. Virtual consultations, remote device monitoring and app-based interventions are being integrated into care. While current evidence is limited to consensus reports, early data suggests improved adherence and symptom tracking when digital tools are used [2].
Emerging Technologies: Machine Learning and AI
Artificial intelligence (AI) and machine learning (ML) are being explored to streamline diagnosis, predict treatment outcomes and detect high-risk phenotypes [10]. A 2025 review noted the need for standardized datasets and validation models before widespread clinical use but the future looks promising.
Special Considerations: Positional OSA and Pediatric Applications
Positional OSA, where apnea events occur primarily when lying on the back, has different cardiovascular outcomes and may respond to targeted interventions like positional therapy [14]. Airway obstruction in positional OSA occurs when the muscles in the back of the throat relax and the airway narrows and collapses.
Meanwhile drug-induced sleep endoscopy (DISE) in pediatric populations is gaining popularity as a tool to visualize dynamic airway collapse and guide surgical decision making [13]. Visualization during DISE often shows collapse at the level of the soft palate which guides surgical decisions.
Metabolic and Cardiovascular Connections
OSA’s role in metabolic disease, including type 2 diabetes, dyslipidemia, metabolic syndrome and diabetes mellitus is being uncovered [11]. Treating sleep apnea may improve insulin sensitivity and reduce systemic inflammation. Cardiovascular risks—including hypertension, arrhythmias and stroke—are significantly higher in untreated OSA patients [5] [14]. OSA is linked to high blood pressure, blood pressure fluctuations, heart failure, congestive heart failure, coronary artery disease. Repeated drops in blood oxygen levels during apnea episodes contribute to cardiovascular problems and increased risk of adverse health outcomes.
Closing Thoughts
OSA management is moving beyond traditional diagnostics and CPAP therapy. Today’s clinicians are using home-based testing, telehealth, AI tools and phenotype-driven care to tailor treatments and improve outcomes. While CPAP is still central, patient engagement, innovation and multidisciplinary care are shaping the future of sleep medicine.
References
[1] Gottlieb, D. J., & Punjabi, N. M. (2020). Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA, 323(14), 1389–1400. https://doi.org/10.1001/jama.2020.3514
[2] Spicuzza, L., Attinà, A., Bignamini, E., Cilla, M., De Bortoli, J., Di Michele, L., Foresi, A., Malorgio, E., Marino, L., Rocca, A., Toraldo, D. M., & Sanna, A. (2025). Telemedicine in the Management of Patients with Obstructive Sleep Apnea: Evidence from the Literature and Practical Issues. A Consensus Document from the Task Force for Telemedicine in Respiratory Diseases, Part of the Italian Society of Telemedicine. Telemedicine journal and e-health : the official journal of the American Telemedicine Association, 10.1089/tmj.2024.0573. Advance online publication. https://doi.org/10.1089/tmj.2024.0573
[3] Maher, L. L. M., & Coke, L. A. (2021). Diagnosis and treatment of obstructive sleep apnea and its impact on cardiovascular disease. Journal of the American Association of Nurse Practitioners, 34(2), 389–396. https://doi.org/10.1097/JXX.0000000000000632
[4] Semelka, M., Wilson, J., & Floyd, R. (2016). Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. American family physician, 94(5), 355–360. https://pubmed.ncbi.nlm.nih.gov/27583421/
[5] White D. P. (2006). Sleep apnea. Proceedings of the American Thoracic Society, 3(1), 124–128. https://doi.org/10.1513/pats.200510-116JH
[6] Hynes, D., & Mansfield, D. (2024). Diagnosis and management of obstructive sleep apnoea in adults. Australian prescriber, 47(2), 52–56. https://doi.org/10.18773/austprescr.2024.010
[7] Labarca, G., Henríquez-Beltrán, M., & Solomons, D. (2025). Precision Medicine to Guide Obstructive Sleep Apnea Treatment Beyond the Continuous Positive Airway Pressure. Seminars in respiratory and critical care medicine, 10.1055/a-2591-5502. Advance online publication. https://doi.org/10.1055/a-2591-5502
[8] Goyal, M., & Johnson, J. (2017). Obstructive Sleep Apnea Diagnosis and Management. Missouri medicine, 114(2), 120–124. https://pubmed.ncbi.nlm.nih.gov/30228558/
[9] Yeşildağ, M., & Duksal, F. (2025). Comorbidities and anthropometric parameters in obstructive sleep apnea syndrome: a phenotype-based study. Clinical and experimental hypertension (New York, N.Y. : 1993), 47(1), 2512136. https://doi.org/10.1080/10641963.2025.2512136
[10] Araujo, M. L. D., Winger, T., Ghosn, S., Saab, C., Srivastava, J., Kazaglis, L., Mathur, P., & Mehra, R. (2025). Status and opportunities of machine learning applications in obstructive sleep apnea: A narrative review. Computational and structural biotechnology journal, 28, 167–174. https://doi.org/10.1016/j.csbj.2025.04.033
[11] Light, M., McCowen, K., Malhotra, A., & Mesarwi, O. A. (2018). Sleep apnea, metabolic disease, and the cutting edge of therapy. Metabolism: clinical and experimental, 84, 94–98. https://doi.org/10.1016/j.metabol.2017.09.004
[12] De Luca Canto, G., Pachêco-Pereira, C., Aydinoz, S., Major, P. W., Flores-Mir, C., & Gozal, D. (2015). Diagnostic capability of biological markers in assessment of obstructive sleep apnea: a systematic review and meta-analysis. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(1), 27–36. https://doi.org/10.5664/jcsm.4358
[13] Xiao, Z., Li, X., Zhou, L., Long, X., Tian, L., & Li, W. (2025). Drug-Induced Sleep Endoscopy and Its Recent Clinical Applications in Combination with Other Procedures in Children: A Narrative Review. Nature and science of sleep, 17, 1067–1077. https://doi.org/10.2147/NSS.S498360
[14] Kang, H., Chow, C., Lobo, J., Logan, J., Bonner, H., Cho, Y., Liu, X., Mazimba, S., & Kwon, Y. (2025). Positional obstructive sleep apnea and cardiovascular outcomes. Sleep & breathing = Schlaf & Atmung, 29(3), 190. https://doi.org/10.1007/s11325-025-03342-y












