Opinion: Medicare to help people make the toughest choices for themselves

Hospice volunteers in Lakewood, Colo., caress the hands of a terminally ill patient.
- Share via
The Obama administration’s move this week to promote end-of-life planning is a belated win for Medicare doctors, who will soon be able to bill the program for more of the time they spend counseling patients on that subject. More important, though, it is a win for Medicare patients.
There’s a reason so many medical professionals want people to go through the process of completing an advance directive -- a set of instructions telling doctors what to do with them in the event they’re incapacitated. They want individuals who are faced with crucial decisions about their care to make them for themselves.
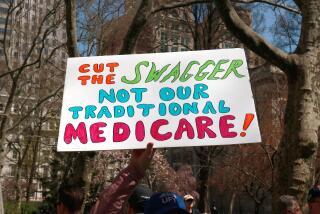
That’s what this issue has always been about. The “death panel” fantasy cooked up by former Alaska Gov. Sarah Palin was based on the nutty idea that letting Medicare pay doctors to advise enrollees about their options while they were healthy was somehow designed to let the government decide who would receive life-saving care and who wouldn’t. (Palin liked the “death panel” concept so much, she later applied it to another aspect of the Affordable Care Act.)
It’s hard to imagine any tougher decision than choosing not to prolong a dying person’s time on this planet. I had that exceptionally unpleasant experience three years ago, when my mom went back into the hospital for what proved to be the last time.
Emphysema and congestive heart failure were killing her, and she was having to work increasingly hard to pull a diminishing amount of oxygen into her bloodstream. After laying out some new options for her to fight back the symptoms, her physician pulled me aside and said that maybe it was time to think about her comfort instead of her survival. He could guarantee the former, he said, but the latter seemed out of reach.
Although I was authorized to make that sort of call, it was the last thing I wanted to do. My role, I thought, was to help my mom find a reason to keep going in spite of how miserable she felt. Fortunately for the both of us, my mom’s mind hadn’t failed her, just her body. She also had completed an advance directive some years before that made her wishes crystal clear, a fact that she reminded her doctors of multiple times during that last stay. She wanted no heroics performed on her behalf; she was ready to stop fighting.
Had the decisions been left to me, I probably would have asked the doctors to try the new course of treatment they’d suggested, even though the odds were slim. That’s exactly why advance directives are important -- because family members and doctors may not know what a patient truly wants if the patient is too sick to tell them.
Granted, it usually saves Medicare money when a patient shifts from treatment to palliative care. Hospitals, on the other hand, make less, as do many of the specialists involved in caring for people who are nearing the end of life. So there are conflicting financial incentives at work, which is all the more reason for individuals to exert as much control as they can over their own treatment.
Medicare already pays doctors to offer end-of-life counseling when new retirees enroll. The proposed rule, which is slated to take effect Jan. 1, would allow them to be repaid for later counseling sessions as well. That makes sense, considering that people’s preferences often change as they age. A 65-year-old still waiting for the first grandchild may want doctors to do everything humanly possible to prolong his or her life; an 80-year-old may not.
These aren’t easy decisions to make, and it helps to have the guidance of doctors who can explain what’s involved and what they’ve seen over the years. Sadly, according to an Institute of Medicine study released last year, millions of older Americans haven’t even started to think about the issue. Medicare’s proposal to reimburse doctors for more of this counseling should help change that.
Follow Healey’s intermittent Twitter feed: @jcahealey
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.