America’s broken PPE pipeline is still broken
- Share via
The COVID-19 pandemic has entered a frightening new phase, picking up speed in every state and breaking new records almost daily. California and Texas have passed 1 million COVID-19 cases, and infections show no signs of slowing.
This new wave of coronavirus infections has hospital resources stretched close to the breaking point in several states, as seriously ill COVID-19 patients crowd critical care units. And as bad as it is, the worst is yet to come, experts predict, as people ignore public-health warnings and gather to celebrate the holidays.
At least we have enough medical masks, gloves and gowns to keep healthcare workers safe, right? The supply chains broken by the onset of a global pandemic in spring surely have been repaired by now?
If only that were the case.
While the acuity of the protective gear shortage has lessened over the past few months, the supply chain is still unreliable. Too many healthcare workers, particularly those not in hospitals, still lack adequate supplies of masks, gloves and gowns and are being forced to reuse equipment meant to be thrown away after one wearing. Even the Strategic National Stockpile has only about one-third the N95 masks that the federal government expected to have by now, according to the New York Times.
“People think the problem is solved,” said Dr. Shikha Gupta, executive director of Get Us PPE, a grass-roots volunteer project connecting donations of protective gear to healthcare facilities in desperate need. “We are as bad off now as we were in March,” she added, noting that the need has risen ominously this month and requests have shifted away from hospitals and critical care centers to nursing homes and small medical practices, among others.
The U.S. has had eight months to prepare for the expected autumn surge of coronavirus cases, but somehow these basic infection control tools are still in short supply. Add it to the growing list of ways that the Trump administration has bungled the pandemic response and left the U.S. in the unenviable position of having more COVID-19 deaths than any other country.
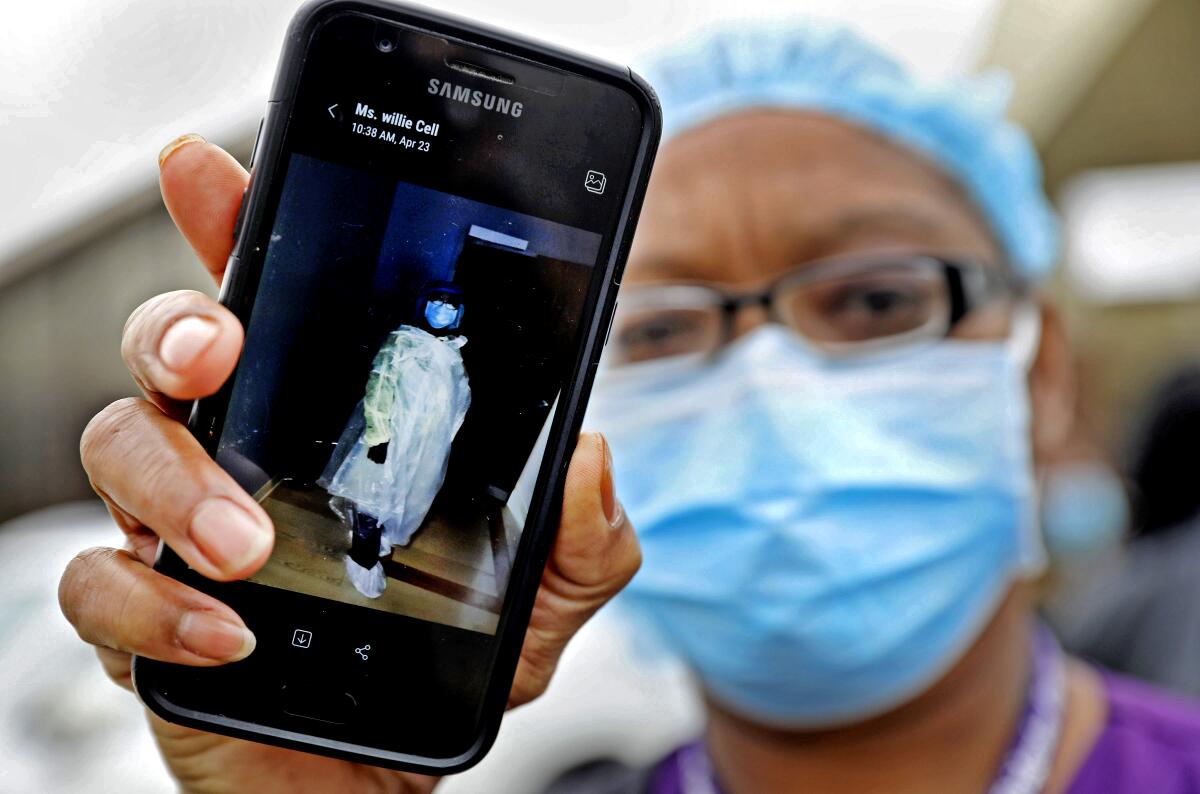
Admittedly, access to protective gear has improved since the dark days of April, when doctors and nurses were forced to wash out disposable N95 masks for days on end and use garbage bags when gowns ran out. Stocks are more reliable, at least for some facilities, and states that had the wherewithal to do so, such as California, have built substantial stockpiles of their own. But the PPE pipeline is far from fixed, and it‘s likely to be strained again as infections rise in the coming weeks.
“The supply chain has improved,” Dr. Susan R. Bailey, president of the American Medical Assn., said in a late October interview. “But there are still many smaller doctors’ offices that don’t have the same access to masks and gowns and face masks that a hospital system would.” And hospitals remain concerned about stable supplies too, particularly nitrile gloves, isolation gowns, N95s and testing supplies, according to the American Hospital Assn.
Most shocking is the situation at nursing homes, which have been particularly hard hit by COVID-19. In California, more than one-third of the COVID-19 deaths were reported at long-term care facilities. Yet these facilities have never stopped struggling to secure enough protective gear for their workers. A study of the PPE supplies of nursing homes by the U.S. Public Interest Research Group found that as of late August, 20% lacked a week’s supply of one or more types of protective equipment and about half had come close to running out between May and August.
“We’re talking about surgical masks. We’re talking about gloves,” said U.S. PIRG’s Teresa Murray of the shortages. “We know how to make this stuff. It’s not difficult.”
No, it’s not, and a functional administration would use the Defense Production Act to compel more production and distribution of protective gear, as medical organizations have been urging. But we have little hope that’s likely to happen, at least until Joe Biden takes over the White House in January. (Indeed, it’s part of Biden’s pandemic plan.)
President Trump seems to believe he’s already defeated the pandemic, using a briefing Friday to tout the progress made on new vaccines and other accomplishments. When he mentioned protective gear, it was in passing and to suggest all was well. Tell that to the doctors and nurses still reusing disposable masks. A vaccine would be invaluable to healthcare workers, but that won’t help keep them from getting infected and possibly dying before it’s widely available.
When the history of the U.S.’s tragic first year of the COVID-19 pandemic is written, it may well be illustrated with photographs of patients in the wealthiest nation on Earth being treated by doctors dressed in garbage bags. Sad.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.






