COVID relief bill would offer more relief on health insurance premiums too

- Share via
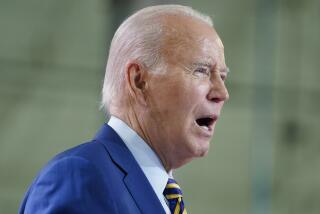
On the campaign trail, Joe Biden pledged to use the Affordable Care Act as a foundation for extending health insurance to all Americans. And in his first major legislative proposal — a $1.9-trillion COVID-19 relief package — Biden is trying to take the first steps in that direction. The moves are significant, but also limited in ways that set up tough choices down the road.
It’s nice to see Washington finally trying to make the ACA deliver affordable coverage to more people, rather than trying to kill it or undermine its protections for people with preexisting conditions. Biden’s proposal, as advanced by the House Ways & Means Committee last week, would provide larger premium subsidies for two years to the vast majority of people who buy coverage through the state Obamacare exchanges.
The state exchanges serve people who aren’t covered by an employer’s health plan or a public program (such as Medicare or Medicaid). That’s a narrow slice of the American public in practice — roughly 19 million Americans buy policies in the nongroup market — but in theory it could be anyone who is self-employed or can’t find work, who retires early or whose workplace offers no coverage.
Under the ACA, the amount of help you receive is tied to your income and the cost of a mid-level policy (that is, a policy that covers 70% of a person’s average annual healthcare bills). For someone with an income equal to or a little above the federal poverty level (which currently sits at $12,760 for a single person and $26,200 for a family of four), premiums for a mid-level policy would be capped at 2% of income. At three to four times the poverty level, premiums are capped at just under 10% of income. Above four times the poverty level, there is no subsidy. As a result, the average mid-level policy last year would have cost a family of four with an income just above four times the poverty level more than 17% of their monthly salary.
Under the Biden proposal, anyone at or near the poverty level could get subsidies large enough to enable them to buy a mid-level policy without paying any premiums. The subsidies would diminish gradually from there, but would be available to people with much higher incomes than the current law provides. The maximum anyone would pay for the benchmark plan — the second least expensive mid-level policy — would be about 8.5% of income.
As you might expect, this is not cheap. The Congressional Budget Office estimates that the federal government’s cost would be $34 billion. That’s because it would cut premiums for millions of Americans by hundreds to thousands of dollars over the next two years.
Peter V. Lee, executive director of Covered California, said the higher subsidies for people earning less than four times the poverty line would cut premiums by an average of $100 a month in this state. For those earning more, Lee said, the expanded federal subsidies would help more than the subsidies that California enacted in 2019, while saving taxpayers here hundreds of millions of dollars.
Larry Levitt, executive vice president for health policy at the Kaiser Family Foundation, noted that people near the poverty line and those who are above the range of the current subsidies “are two groups that have been squeezed by healthcare costs.” The Biden proposal “would fill in some of the big affordability gaps in the ACA as originally enacted,” he said.
But there are downsides, starting with the temporary nature of the increase in subsidies. Unless Congress extends the relief, people who shop at the state exchanges will be in for a rude awakening when their premiums jump in two years.
“It also doesn’t fully resolve affordability issues, such as high deductibles, or do anything to help people with employer coverage who struggle with the high cost,” Levitt observed.
Indeed, the problem with the ACA is that it did little to rein in the rising cost of medical services, devices and pharmaceuticals that have driven premiums and deductibles steadily higher. Instead, it launched a number of experiments aimed at giving doctors, hospitals and insurers more incentive to limit spending, which have encouraged some new approaches but haven’t transformed the industry.
Like the ACA itself, Biden’s temporary plan addresses affordability by pouring more money into subsidies, not by doing the much harder and more controversial work of lowering the cost of healthcare services. But if subsidies are its only response to the problem, the federal government won’t be applying any pressure on the industry to deliver more care for the dollar, and premiums will continue to rise faster than inflation. That’s not making healthcare more affordable, it’s just shifting an ever-growing bill from one payer — people with insurance — to another — people who pay taxes.
The COVID relief bill would buy Congress time to work on a longer-term answer, even though lawmakers may be tempted just to extend the higher subsidies for several more years. At some point, however, they are going to have to grapple with the incessant increase in healthcare spending, or live with the consequences of healthcare bills consuming a larger and larger share of the economy, crowding out potentially more productive uses of our dollars.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.