Coronavirus Today: Inside our struggling hospitals
- Share via
Good evening. I’m Amina Khan, and it’s Wednesday, Dec. 16. Here’s what’s happening with the coronavirus in California and beyond.
We’ve been feeling a little brighter now that the first batch of authorized COVID-19 vaccines is being deployed in California. But that shouldn’t obscure the extraordinarily bleak situation we’re facing in the pandemic — or the overwhelming burden that it’s putting on doctors and nurses statewide.
California has logged nearly 1.7 million coronavirus cases and more than 21,800 COVID-19 deaths. There are now nearly 15,000 people hospitalized across the state, a figure more than six times what it was at the end of October.
If those numbers don’t telegraph the strain that healthcare workers are facing, listen to the nurses and doctors inside those facilities who are desperate to stem the flow of the sick and dying — and trying to remain calm in the process.
Take Annel Meza, an emergency room nurse at Riverside University Health System, who told my colleague Hayley Smith that hospitalizations are rising so fast that staff has been forced to put patient beds in the hallway. “Sometimes there’s no beds at all,” she said.
Or Dr. Hari Reddy, an intensivist at St. Bernardine Medical Center in San Bernardino, where the flood of COVID-19 patients has forced him to make wrenching life-or-death decisions. “There’s been times when we’ve had multiple patients having cardiac arrest at the same time, and we’ve had to really triage to figure out which patient to resuscitate first,” he said. “If there’s multiple emergencies, I try to gauge which patient I can make the most difference in.”
Hospitals too have been forced to make tough choices, some of which my colleagues Rong-Gong Lin II and Luke Money describe. They’ve canceled scheduled surgeries, kept critically ill patients in emergency rooms and sent intensive care unit patients into step-down units earlier than they would in normal circumstances. They’ve trained nurses from other departments to help with intensive care and increased the numbers of patients that an ICU nurse can treat.
Emergency rooms are so crowded that some ambulances have been forced to wait up to six hours to offload patients. Some patients arriving by ambulance have been asked to sit in the emergency department so that their ambulance can depart.
California is scrambling to find enough nurses, doctors and other medical staff to deal with the pandemic’s rising demands, but just one out of every 10 temporary contracted positions needed to manage the surging caseloads has been filled. And the state’s Health Corps, created in March, has not been able to make up the difference, because only a small fraction of the thousands who signed up to volunteer have been available to staff the overloaded facilities, my colleague Melody Gutierrez writes.
“Staffing has gone to places that started surging a month and a half ago,” said Joanne Spetz, an associate director of research at Healthforce Center at UC San Francisco. “That makes our scramble harder.”
This surge has created new challenges for doctors already handling a heavier caseload. Reddy said that while the pandemic’s first wave was characterized by clusters, such as nursing home residents swept up in an outbreak, he’s now seeing the virus in younger people in their 20s and 30s. Often, entire families are infected.
That family factor has become harder to ignore, and many experts have pointed to Thanksgiving gatherings as a flash point for the current surge. Officials say they hope people will learn from the past and abide by health warnings to stay home for Christmas.
“I would love for any one of them to come live life in the day of a nurse or a respiratory therapist who has to go into a COVID room multiple times every hour, or just walk through the ICU to see how sick patients are,” Reddy said. “I think it would really change people’s opinions.”
By the numbers
California cases and deaths as of 5:02 p.m. PST Wednesday:
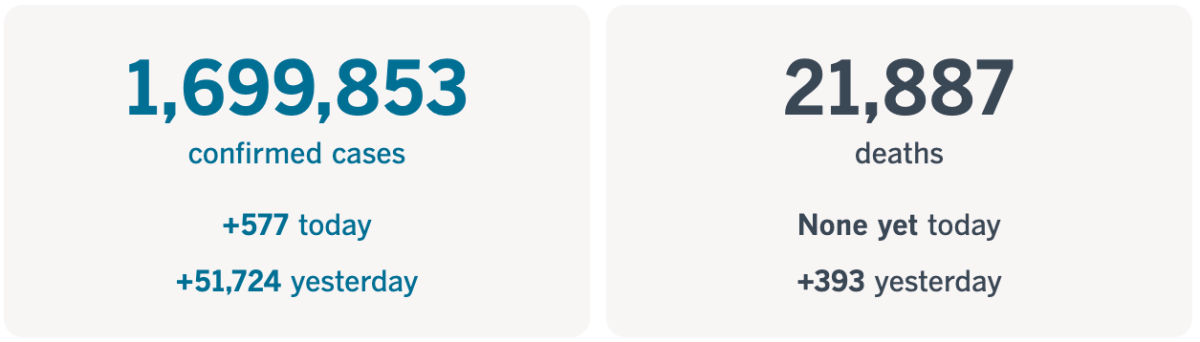
Track the latest numbers and how they break down in California with our graphics.
Across California
I know that was rough to read. So here’s some more hopeful news: California expects to receive 1 million more COVID-19 vaccine doses this month, which should help arm the state’s healthcare workforce at a pivotal moment in the pandemic.
The additional 393,900 doses of the Pfizer-BioNTech vaccine should be on their way, and if Moderna’s vaccine is authorized by the Food and Drug Administration as expected, some 672,000 doses of it could also make their way to the state. Both would be welcome additions to California’s first allocation of roughly 327,000 doses.
Health workers and nursing home residents will get priority for the vaccines, both of which require two doses (spaced three weeks apart in the case of the Pfizer vaccine and four weeks apart for Moderna’s). Facilities in Los Angeles, San Diego, San Francisco and Eureka received vaccines Monday; 24 other sites were expected to receive shipments Tuesday and five more Wednesday.
In L.A. County, Keck Medicine of USC and USC Verdugo Hills Hospital are scheduled to receive about 2,500 vaccine doses between them this week. Officials say the plan is to start vaccinations within four hours of picking up the doses Thursday.
“We have the vaccine; that’s amazing,” said Dr. Neha Nanda, medical director of infection prevention at the USC Keck School of Medicine. “It took more than 10 years to get the polio vaccine. ... Now, within nine months, we have a vaccine. It is going to change our lives.”
The help can’t come soon enough. California shattered another single-day record for COVID-19 deaths, with 295 lives lost Tuesday, according to the L.A. Times’ tracker. This easily breaks the last single-day record of 219 deaths, set Dec. 8 and repeated Friday.
Multiple counties set single-day death toll records too, with 93 in Los Angeles, 32 in San Diego, 24 in Santa Clara, nine in Yolo, six in San Luis Obispo and five in Santa Cruz.
Gov. Gavin Newsom acknowledged the devastation, saying state officials have had to order 5,000 body bags and 60 refrigerated storage units for storing corpses.
“Let’s deal with some sober realities,” Newsom said. “This is a deadly disease. And we need to be mindful of where we are in this current journey together to the vaccine: We are not at the finish line yet.”
In response to soaring numbers of COVID-19 patients, Orange County will be deploying mobile field hospitals to relieve some of the pressure on the region’s healthcare system. Three hospitals — Fountain Valley Regional, St. Jude Medical Center and UC Irvine — have already requested the mobile units, which will add 25 to 50 beds to their existing capacities.
The latest state data show that there were 1,486 hospitalized coronavirus-positive patients in Orange County on Tuesday, an all-time high that has more than doubled from just two weeks prior. And the county’s number of COVID-19 patients in intensive care had risen to 319 as of Tuesday; a month ago, there were 85.
“I think what we’re seeing is not a surge — more like a tsunami, I’m sorry to say,” said County Supervisor Doug Chaffee.
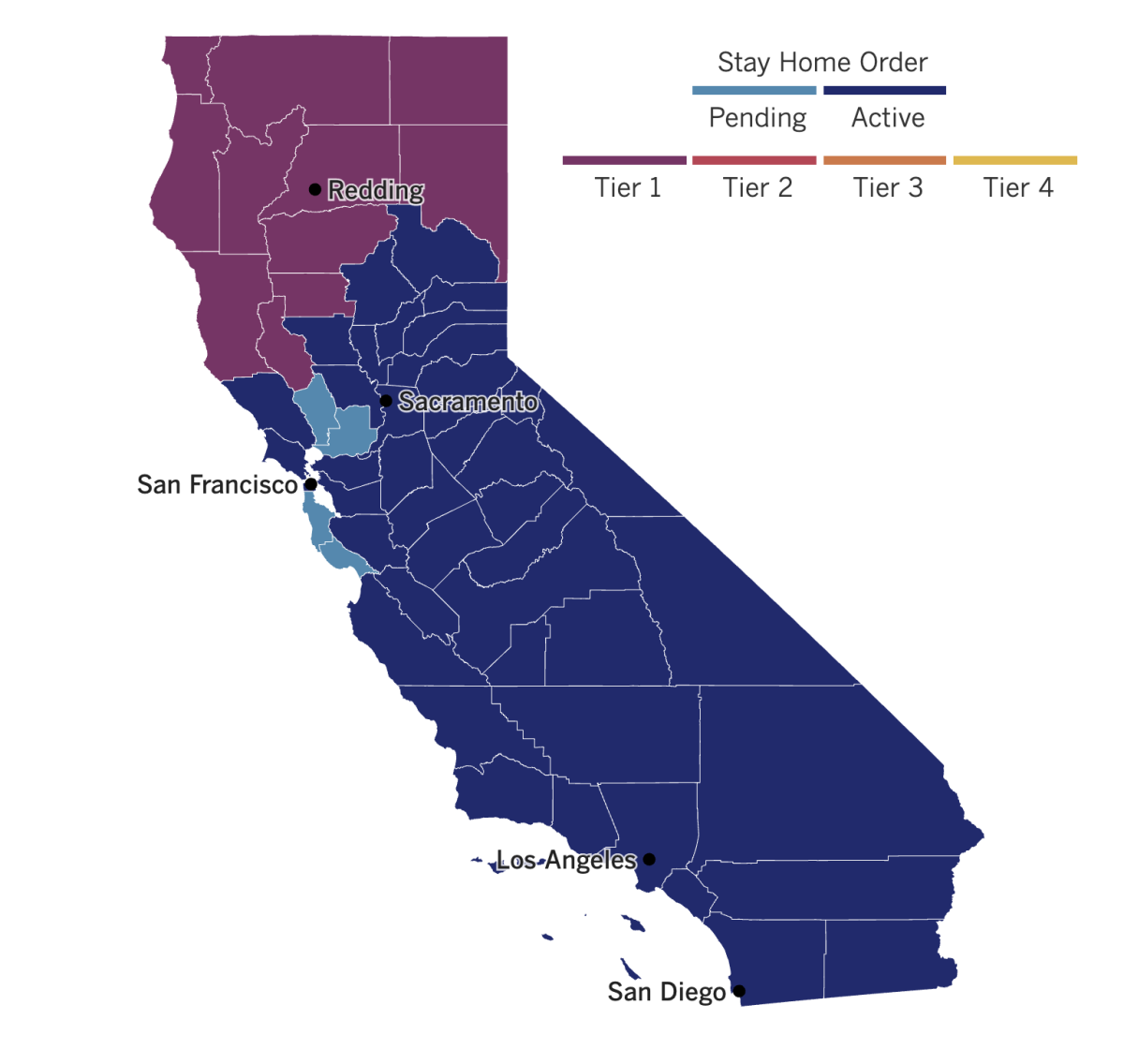
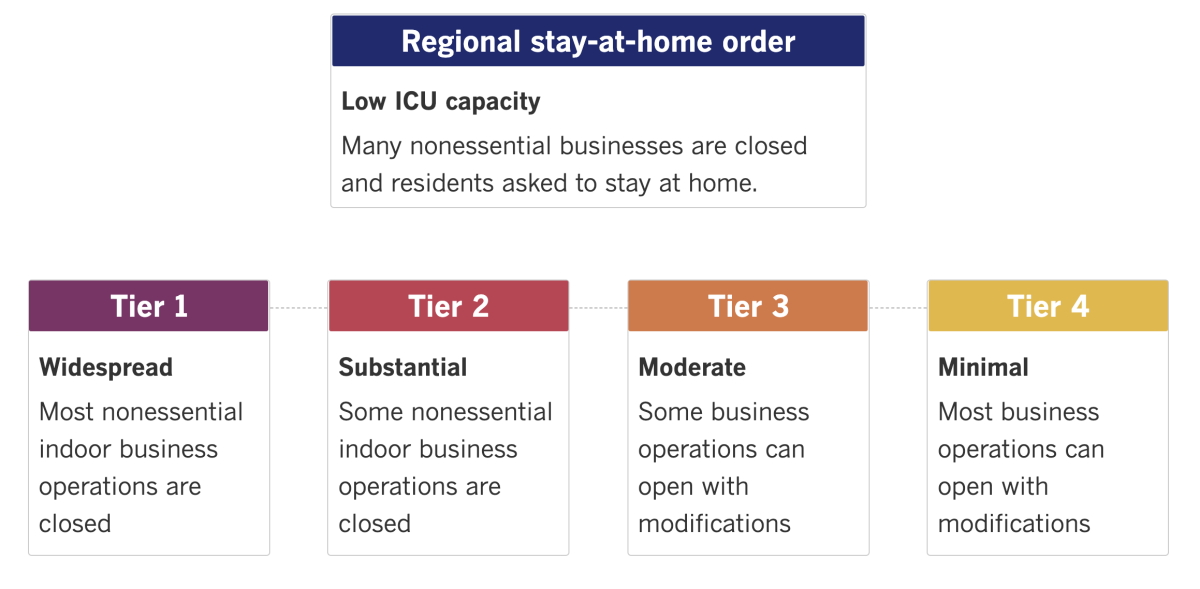
See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
The first over-the-counter home test for COVID-19 should be on U.S. store shelves soon. Federal regulators have authorized the rapid test, which can be done entirely at home — marking a small but important step toward expanding coronavirus testing options. (A similar test was given the go-ahead last month, but that one requires a prescription.)
Health experts have stressed the need for fast and widely available home testing so that people can regularly screen themselves and avoid contact with others if they’re infected. But the vast majority of tests still require a nasal swab performed by a health worker that must then be processed in a lab, which usually means waiting days for results. Roughly 25 tests allow people to collect their own sample at home via nasal swab or saliva, but those must be shipped to a lab as well.
The new kit includes a nasal swab, a chemical solution and a testing strip. It also requires a smartphone app to display the results and help users interpret them. The test will cost $30, still a high price point for many. And initial supplies will be limited, though the Australian maker says it expects to ramp up production in the first half of next year.
In western Kansas, Dodge City Mayor Joyce Warshaw has resigned after her public support for a mask mandate prompted threatening emails and phone calls and left her concerned for her safety. The city commission, which Warshaw headed as mayor, voted 4-1 on Nov. 16 to impose a mask mandate, with several exceptions.
Some of the threatening emails have been turned over to police. But Warshaw said she still doesn’t regret voting for the mandate. Dodge City sits in Ford County, which has logged 4,914 coronavirus cases in a population of 33,600 residents.
“This is harder for me than people realize,” Warshaw said as she began to cry. “I really love this city with all my heart. I still believe in this city, and I believe in their ability to not harm one another.”
In Washington, D.C., congressional leaders are closing in on an economic aid package worth about $900 billion. It’s expected to add $300 per week to state compensation for the unemployed and provide a one-time direct payment of at least $600 for most Americans, my colleague Sarah D. Wire reports.
The package is also expected to include another round of Paycheck Protection Program loans for small businesses as well as money for vaccine distribution, food assistance, rent payments, child care and schools.
Federal Reserve Chairman Jerome H. Powell, who has urged legislators to pass additional federal relief as the pandemic continues to devastate Americans’ economic outlook, welcomed the news. “The case for fiscal policy right now is very, very strong,” he told reporters. “With the expiration of unemployment benefits, the expiration of eviction moratoriums, with the virus spreading the way it is, there’s a need for households and businesses to have fiscal support.”
In Brussels, a hack of COVID-19 vaccine data prompted the European Union to develop a plan to revamp the 27-nation bloc’s dated cybersecurity rules. The new plan will be debated by EU countries and the European Parliament, and substantial changes are likely.
Pfizer and German pharmaceutical company BioNTech said last week that data on their new COVID-19 vaccine were “unlawfully accessed” during a cyberattack on the European Medicines Agency’s servers. Officials said the attack should not affect the agency’s timeline for reviewing and potentially authorizing the Pfizer-BioNTech vaccine, which has already been deployed in Great Britain, the United States and Canada. The agency plans to meet to review the vaccine Monday.
Pfizer and BioNTech, meanwhile, said that none of their own systems had been breached and they were not aware that any study participants had been identified as a result of the data hack.
Your questions answered
Today’s question comes from readers who want to know: If I get the vaccine, do I still have to wear a mask?
The short answer is yes, absolutely, you should continue to mask and keep following all other social distancing protocols for the time being. I discussed this question with Dr. Marc Sala, a critical care and pulmonary specialist at Northwestern University Feinberg School of Medicine, to understand why.
“There are two reasons that someone who receives a COVID-19 vaccine should still wear a mask and commit to social distancing,” Sala explained. First, the Pfizer and Moderna vaccines were shown to prevent cases of COVID-19, but because of the way the clinical trials were designed, it’s not clear that they’ll be able to prevent coronavirus transmission. Second, he said, “the rollout of these vaccines will take many months, and we want to continue [to] protect those people who will not receive the vaccine until later (or who cannot receive it for any reason).”
By way of example, a vaccinated person could in theory be exposed to someone with the virus. Even though they’re vaccinated, the virus might hang out in their respiratory tract for a presumably brief amount of time as it tries (and probably fails) to get a foothold in their system. During that time, if they’re unmasked, they could laugh or cough or just breathe near someone else, who might then become infected and potentially develop COVID-19.
While someone who has received the vaccine may not feel ill, they “could still spread the virus to another person,” Sala said.
That means that until we achieve herd immunity, people should continue to mask up and social distance — regardless of whether they’ve gotten their shots.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




