Esophageal Strictures: Causes, Types, and How They’re Treated

- Share via
Key Facts
- Peptic strictures, caused by acid reflux, account for nearly 68% of esophageal stricture cases.
- Esophageal strictures are classified as simple or complex based on length, shape, and treatment difficulty.
- Dysphagia is the most common symptom, often making eating and drinking stressful or painful.
- Endoscopic dilation is the go-to treatment, but recurring strictures may require steroid injections or self-dilation.
- Incidence increases with age, making esophageal strictures a growing concern in aging populations.
When something as simple as swallowing becomes a daily struggle, it’s often a sign that something more complex is happening beneath the surface. That’s exactly what occurs with esophageal strictures—a condition where the esophagus, the muscular tube that carries food to your stomach, becomes narrowed. While this narrowing may seem like a small issue, it can profoundly affect eating, nutrition, and overall quality of life.
Let’s break down what causes esophageal strictures, how doctors classify and treat them, and why early, tailored care matters.
Table of Contents
- What Are Esophageal Strictures?
- Types and Classifications
- How Common Are They?
- What Causes Esophageal Strictures?
- What Happens in the Body?
- How Strictures Affect Daily Life
- How Are They Treated?
- Reference
What Are Esophageal Strictures?
An esophageal stricture is exactly what it sounds like: a narrowing of the esophagus that makes it hard for food and liquids to pass through, not too different from Esophagitis, but essentially, esophagitis is the inflammation, while stricture is a consequence of that inflammation. The telltale symptom is dysphagia, or difficulty swallowing, which can start subtly—like food getting stuck or meals taking longer—and then worsen over time [3], [6], [7].
This condition can be benign (non-cancerous) or malignant (cancer-related), with benign causes being much more common.
Types and Classifications
Doctors typically classify esophageal strictures into simple or complex types. Here’s what that means in practice:
- Simple strictures: These are short (usually under 2 cm), straight, and easy to stretch open with endoscopic tools.
- Complex strictures: These are longer, twisted, or severely narrowed, and more difficult to treat [11].
Classification also considers how easy it is to perform dilation (a procedure to widen the narrowed section), and how likely the stricture is to return.
How Common Are They?
While esophageal strictures aren’t extremely common, they’re not rare either. One study found that about 1.1 people per 10,000 develop them each year, and the likelihood increases with age [2]. As populations continue to age, especially in the U.S. and Europe, healthcare providers are expecting to see more cases over time.
What Causes Esophageal Strictures?
There isn’t just one trigger for esophageal strictures—many different conditions can lead to this problem. That’s why doctors tailor treatment based on the underlying cause. Here are the most common culprits:
- Peptic strictures: These make up around 68% of cases and result from chronic acid reflux or GERD, which damages the esophageal lining over time [2].
- Caustic injuries: Swallowing corrosive substances—either accidentally or intentionally—can severely burn the esophagus [10].
- Eosinophilic esophagitis: An allergic inflammatory condition, often triggered by food allergens, that leads to chronic inflammation [7].
- Radiation therapy: Used for cancers near the esophagus, radiation can cause scarring that leads to narrowing.
- Surgical resection: Operations involving the esophagus can cause scar tissue to form.
- Lower esophageal sphincter dysfunction: When the valve that controls food flow to the stomach doesn’t work properly, it can cause backup and irritation [4].
What Happens in the Body?
Most esophageal strictures develop in three stages [1]:
- Damage to the inner lining of the esophagus—often due to acid, inflammation, or injury.
- Chronic inflammation sets in as the body tries to repair the damage.
- Fibrosis (scarring) thickens and narrows the esophageal tissue.
Over time, the esophageal passage becomes so tight that even swallowing liquids can become challenging.
How Strictures Affect Daily Life
Dysphagia isn’t just an inconvenience—it can be emotionally and physically draining. People often feel anxious around mealtime, avoid social gatherings, or lose weight because eating becomes painful or slow [5].
In severe cases, individuals may resort to soft or pureed diets just to get by. These dietary adjustments can leave people malnourished or dehydrated without realizing it [8].
How Are They Treated?
Treating esophageal strictures usually involves a combination of procedures and medications. Here’s a look at the main options:
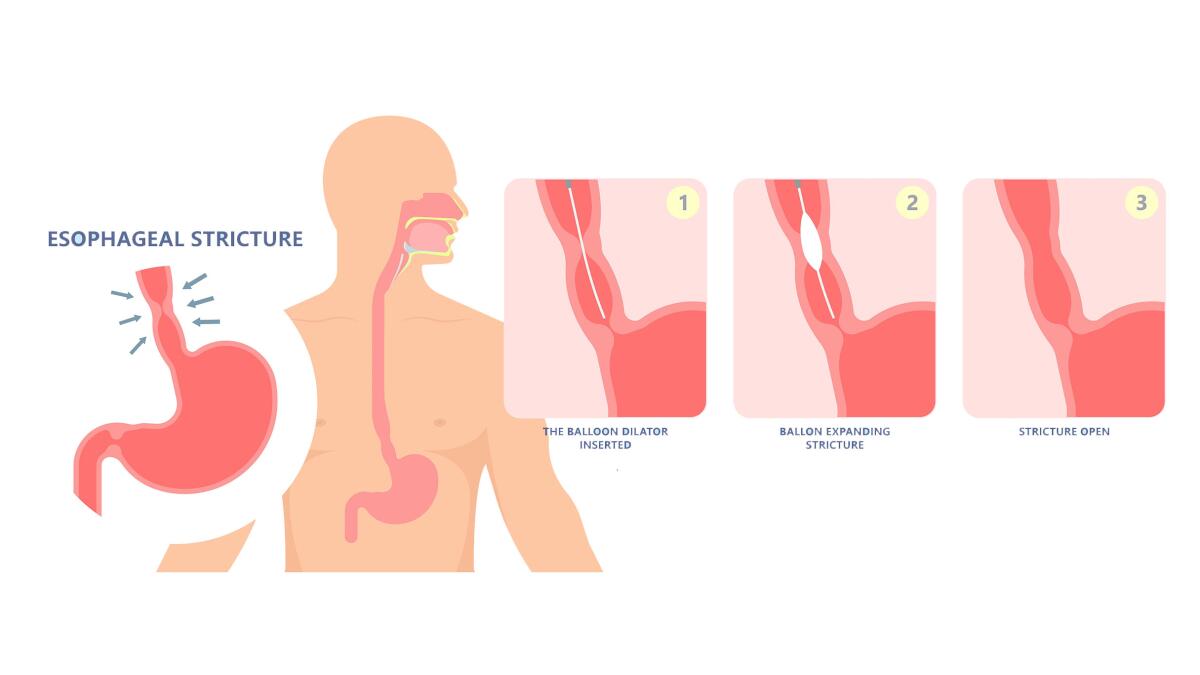
- Dilation: This is often the first line of treatment. Using an endoscope, doctors gently stretch the narrowed area to open it up [6].
- Acid Suppression Therapy: For peptic strictures caused by GERD, proton pump inhibitors (PPIs) are prescribed to reduce stomach acid and prevent further damage [5].
- Steroid Injections: In some stubborn cases, doctors inject corticosteroids like triamcinolone directly into the stricture to reduce inflammation [12].
- Esophageal Self-Dilation: For patients with refractory strictures—those that keep coming back despite treatment—self-dilation using prescribed tools may be recommended [9].
- Surgery: Reserved for the most severe cases, especially when dilation fails or the anatomy is highly complex [11].
Each treatment plan is highly individualized. For example, a young adult with eosinophilic esophagitis might benefit more from diet changes and topical steroids, while an older adult with peptic strictures may need lifelong acid suppression.
For more insights on treatment innovations, see this overview of self-dilation techniques, or this recent review on managing refractory strictures.
Closing Thoughts
Esophageal strictures may be a common problem, but that doesn’t mean they should be ignored. With causes ranging from acid reflux to allergies to radiation therapy, it’s clear that no two cases are the same. Early recognition of dysphagia and getting to the root of the cause is key to improving outcomes. Thanks to advances in endoscopy, medications, and even self-care strategies, most patients can return to eating—and living—more comfortably.
References
[1] Yang, F., Hu, Y., Shi, Z., Liu, M., Hu, K., Ye, G., Pang, Q., Hou, R., Tang, K., & Zhu, Y. (2024). The occurrence and development mechanisms of esophageal stricture: state of the art review. Journal of translational medicine, 22(1), 123. https://doi.org/10.1186/s12967-024-04932-2
[2] Ruigómez, A., García Rodríguez, L. A., Wallander, M. A., Johansson, S., & Eklund, S. (2006). Esophageal stricture: incidence, treatment patterns, and recurrence rate. The American journal of gastroenterology, 101(12), 2685–2692. https://doi.org/10.1111/j.1572-0241.2006.00828.x
[3] Siersema P. D. (2008). Treatment options for esophageal strictures. Nature clinical practice. Gastroenterology & hepatology, 5(3), 142–152. https://doi.org/10.1038/ncpgasthep1053
[4] Smith C. D. (2015). Esophageal strictures and diverticula. The Surgical clinics of North America, 95(3), 669–681. https://doi.org/10.1016/j.suc.2015.02.017
[5] Burr, N. E., & Everett, S. M. (2019). Management of benign oesophageal strictures. Frontline gastroenterology, 10(2), 177–181. https://doi.org/10.1136/flgastro-2018-101075
[6] Norton, B. C., Papaefthymiou, A., Aslam, N., Telese, A., Murray, C., Murino, A., Johnson, G., & Haidry, R. (2024). The endoscopic management of oesophageal strictures. Best practice & research. Clinical gastroenterology, 69, 101899. https://doi.org/10.1016/j.bpg.2024.101899
[7] Fugazza, A., & Repici, A. (2021). Endoscopic Management of Refractory Benign Esophageal Strictures. Dysphagia, 36(3), 504–516. https://doi.org/10.1007/s00455-021-10270-y
[8] Poincloux, L., Rouquette, O., & Abergel, A. (2017). Endoscopic treatment of benign esophageal strictures: a literature review. Expert review of gastroenterology & hepatology, 11(1), 53–64. https://doi.org/10.1080/17474124.2017.1260002
[9] Halland, M., Prichard, D. O., Kahn, A., Lavey, C. J., Katzka, D. A., & Alexander, J. A. (2024). Esophageal Self-Dilation in Benign Refractory Esophageal Strictures: Outcomes from a Randomized Controlled Trial and a Prospective Observational Study. Digestive diseases and sciences, 69(8), 2883–2889. https://doi.org/10.1007/s10620-024-08402-z
[10] van Boeckel, P. G., & Siersema, P. D. (2015). Refractory esophageal strictures: what to do when dilation fails. Current treatment options in gastroenterology, 13(1), 47–58. https://doi.org/10.1007/s11938-014-0043-6
[11] Csendes, A., & Braghetto, I. (1992). Surgical management of esophageal strictures. Hepato-gastroenterology, 39(6), 502–510. https://pubmed.ncbi.nlm.nih.gov/1483661/
[12] Kochhar, R., & Makharia, G. K. (2002). Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointestinal endoscopy, 56(6), 829–834. https://doi.org/10.1067/mge.2002.129871












