Coronavirus Today: Running out of patience for patients
- Share via
Good evening. I’m Karen Kaplan, and it’s Friday, Jan. 14. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Dr. Jason Chertoff is a pulmonary and critical care specialist in Zanesville, Ohio. He was drawn to medicine by a desire to help people. But nearly two years in, the pandemic has sucked away his sense of compassion — and he’s not happy about it.
“Before COVID, what I did a lot of was treating people with lung cancer. I never felt anything bad toward them if they were smokers,” said Chertoff, 43. “But what I don’t like is what I’m feeling now. I have resentment and anger toward patients not doing their part to curtail the spread of this.
“I have to put that aside and take care of people no matter their choices,” he continued. “That is my job. But, wow, is it hard.”
It was a striking admission for a doctor to make: He doesn’t judge lung cancer patients for being smokers, but he does judge COVID-19 patients for being unvaccinated. He’s not proud of those feelings, but he shared them with my colleagues Jaweed Kaleem and Emily Baumgaertner because he wants people to understand just how critical the situation has become.
Across the country, the Omicron-fueled surge has exhausted the morale of medical personnel, turned hospitals into round-the-clock triage centers and forced patients with conditions like cancer and heart disease to postpone necessary surgeries and treatments.
This week, the number of COVID-19 patients in U.S. hospitals surpassed last January’s record of 132,051. The sheer number of people infected with the coronavirus — both patients and the people who care for them — adds a new level of complexity to the mix. In some cities, hundreds or even thousands of hospital employees are being sidelined by COVID-19 each week.
In other words, medical workers have become the new ventilators — the crucial piece of hospital material that’s in dangerously short supply.

“There’s just a lot more virus out there in the community. And healthcare workers, just like anybody else, are getting infected,” said Dr. Christina Ghaly, director of the Los Angeles County Department of Health Services.
It’s not just doctors and nurses, Ghaly added. Hospitals are grappling with shortages of “respiratory therapists, radiology techs, lab staffs — the whole gamut of what is needed to run a hospital safely.”
California has adopted a controversial strategy for dealing with the problem: allowing hospital workers with active coronavirus infections to come to work as long as they have no COVID-19 symptoms, wear proper face masks and work only with patients who are already infected themselves.
In Massachusetts, Ohio, Georgia and other states, hospitals are calling in the National Guard to shore up their staff.
The reinforcements are welcome. Healthcare workers are feeling overworked and underappreciated. The era of being thanked every evening with signs, cheers and clanging pots is long gone.
“At the beginning, there was great morale on the front lines,” said Ariana Cellini, a nurse who works 12-hour shifts in the intensive medical unit at Tufts Medical Center in Boston. “Then, when people wouldn’t get vaccinated or said it was a hoax, many of us got angry. Now, we’re essentially numb.”
By the numbers
California cases and deaths as of 4:44 p.m. on Friday:
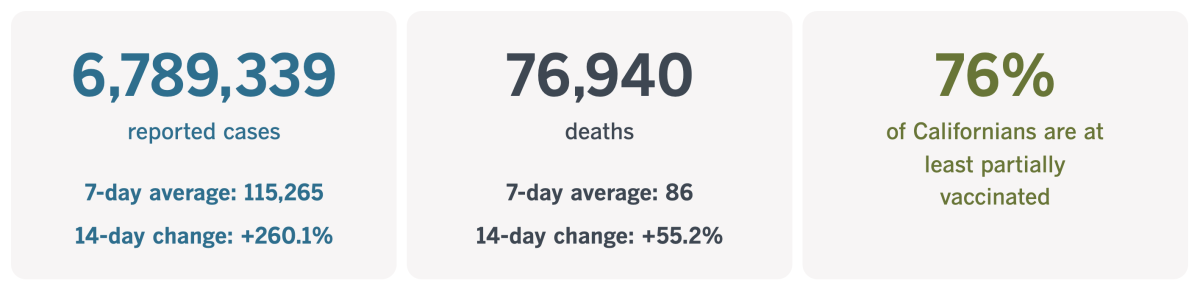
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Surprise! Your boss misses you
Google is making plans to move workers into an office complex that used to be the Westside Pavilion. Adidas just agreed to lease the top floors of the California Market Center in downtown L.A.’s Fashion District. The Roku Channel streaming service has become so popular that it’s moving to bigger digs in Santa Monica.
Why are these and other companies doubling down on office space? Hasn’t the pandemic proved that workers can be just as productive at home? And is there anyone who actually misses their commute?
Perhaps absence makes the heart grow fonder. Although companies in many industries have learned to adapt to managing a remote workforce, they’ve also come to appreciate the upside of bringing employees together.
Bosses are laying out the bucks to make it happen. In L.A. County, companies leased more new office space in the last three months of 2021 than they let go, my colleague Roger Vincent reports.
Workers see some upsides, too. In a survey conducted last month by Korn Ferry, a workforce consulting firm, 64% of respondents said being with their co-workers in an office would make them “happy.” In addition, 49% said getting back into an office would have “a positive impact” on their mental health. (To be fair, the remaining 51% said it would have “a negative impact,” and 12% said they would quit their jobs if they were suddenly forced to go back, even on a part-time basis.)
The companies investing in offices don’t necessarily expect their employees to be there 40 hours a week.
People “like the hybrid model” of working from home and getting out of the house, said CBRE real estate broker Todd Doney. “Offices will be an important component for companies going forward.”

Indeed, there seems to be a correlation between the lure of a company’s office and its overall performance.
A survey conducted by the architecture firm Gensler found that in top companies — that is, those that appeared on lists of “most admired” and “best places to work” — employees cited many reasons for wanting to be in the office. Among them: brainstorming with colleagues, having a place suitable for deep concentration and working on creative tasks.
By contrast, workers at run-of-the-mill companies saw fewer reasons to be there in person.
“People are realizing how important relationships are for doing great work, not just being productive,” said Elizabeth Brink, a regional managing principal in Gensler’s workplace consulting practice.
Bosses are coming to understand that an appealing physical workspace can prompt employees to work together better, driving performance and innovation. Indeed, some companies say they’ll need even more office space in the future to create the kinds of collaborative, engaging environments that will make workers want to commute.
Brink cited one more upside of going to the office: Working alongside your peers improves your state of mind. With year three of the pandemic approaching, who couldn’t use a boost like that?
“I firmly believe the overall mental health of employees is improved by coming in some of the time,” she said. “Interaction is really critical to mental health.”
California’s vaccination progress
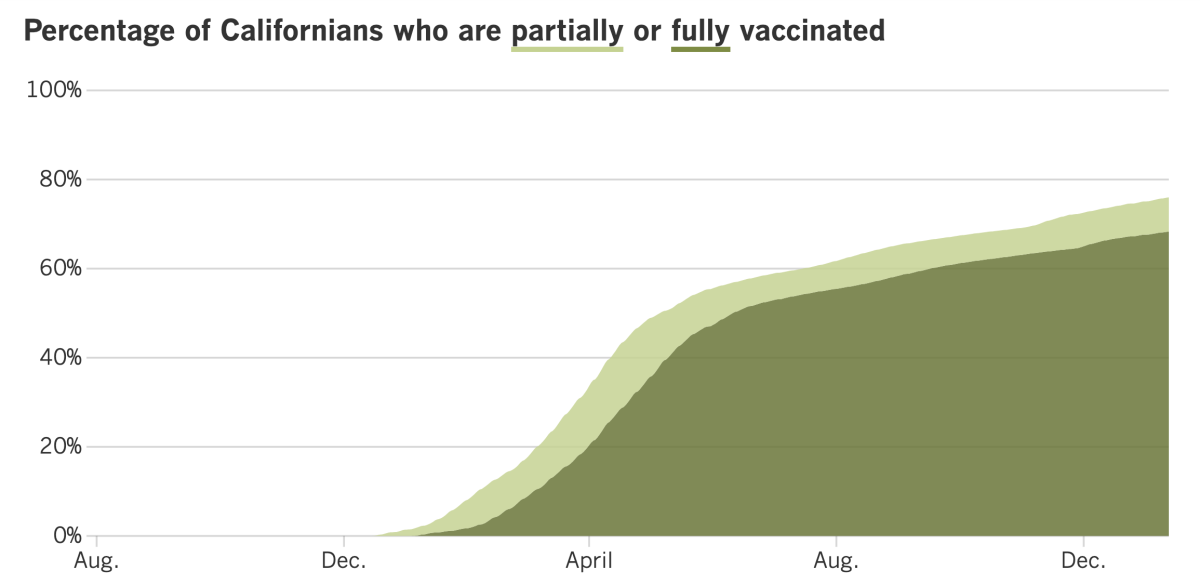
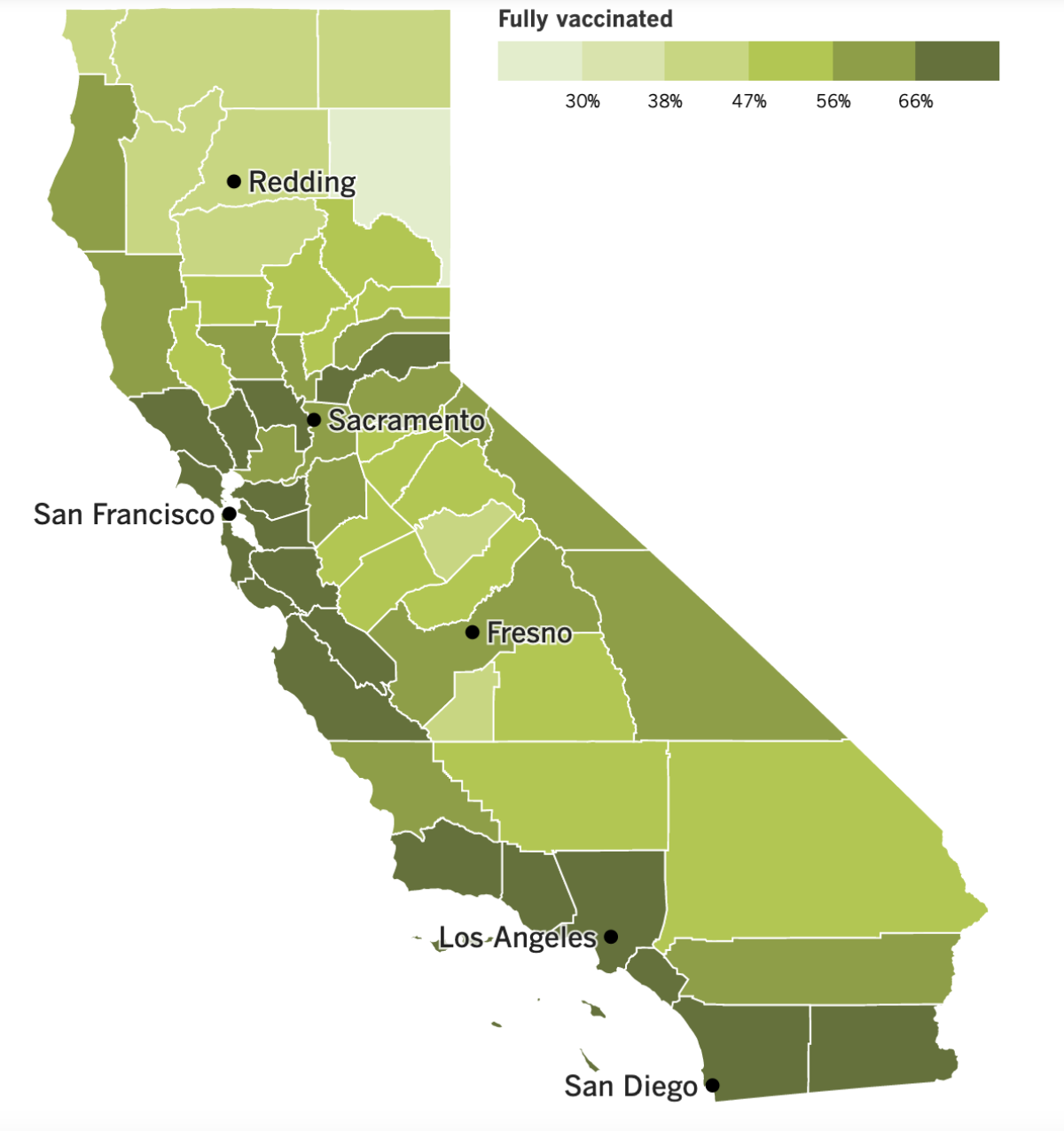
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
The end of the Omicron surge may be in sight.
Computer models suggest the onslaught of new cases may peak as early as next week, or else in late January, according to Dr. Kirsten Bibbins-Domingo, chair of the UC San Francisco Department of Epidemiology and Biostatistics. There will still be cases after that, of course, but, she said, “I do think it is reasonable by the middle of February that we will really be in a substantially better place.”
Gov. Gavin Newsom seconded that forecast. In other countries, and even in other parts of the United States, “we’re starting to see, in the last three or four days, some case leveling,” he said. “That’s going to happen here in the state of California as well. ... We’re going to get through this — just a few more weeks.”
In the meantime, Newsom said 4.5% of Californians infected with Omicron are winding up in hospitals, way below the 15% to 20% from last winter. But before you get too excited about that apparent progress, consider that the total number of infections is so much higher that more COVID-19 patients are going to emergency rooms now than they were a year ago. In fact, the total number of hospitalized patients statewide has more than tripled since Christmas.
To help weather the surge, Los Angeles County health officials are urging the public to postpone nonessential gatherings and avoid activities that include people who are unmasked, unvaccinated or more vulnerable to a severe case of COVID-19. (The Los Angeles Homeless Services Authority apparently took that recommendation to heart and delayed its annual homeless census until Feb. 22-24. The count, which was canceled last year amid the winter surge, involves roughly 7,000 volunteers.)
COVID-19 deaths are rising in California — the state has averaged 108 deaths per day over the past week, more than double the level two weeks ago — but health officials suspect the Delta variant is largely to blame.
“Many people are sick for quite a while, and many are hospitalized for quite a while before they pass away, so it is likely that most of the deaths we are seeing are still related to Delta, although not entirely,” said L.A. County Public Health Director Barbara Ferrer.
Here’s another Omicron-vs.-Delta comparison: A preliminary study based on the medical records of nearly 70,000 Southern Californians found that those infected with Omicron were 53% less likely to be hospitalized with COVID-19, 74% less likely to require treatment in the ICU and 91% less likely to die of the disease.
As expected, Omicron has complicated the return to school after winter break. L.A. Unified campuses reopened Tuesday, and the district has already marked about 130,000 students absent. That’s about one-third of LAUSD’s total enrollment.
Students went back to Culver City public schools last week, but that may have been premature. On Friday, the district said its schools would be closed next week to give its 7,100 students and 900 staff time to “recoup and recover” from a surge in coronavirus cases.
Problems like these aren’t unique to Southern California. About 4% of schools across the country have dealt with some kind of COVID-related disruption this week, according to Burbio, a K-12 school-opening tracker. Most of the schools that closed were in the Northeast and Midwest, though those in the West and South are starting to catch up.
An increasingly vocal contingent of students is calling for stronger safety measures in their schools or, failing that, a return to remote learning. Pupils in Oakland are threatening a strike if their pandemic health and safety concerns aren’t addressed. In New York, hundreds of students have boycotted classes and staged walkouts over concerns about testing.
Parents aren’t happy, either. Some don’t want to go back to distance learning, and some don’t want to send their kids to coronavirus-laden campuses. I’m sure the uncertainty of not knowing from one day to the next whether their kids will be on campus or at home is no great shakes, either.
One thing that is in parents’ control is getting their kids vaccinated. But misinformation, doubt and complacency have conspired to keep vaccination rates for children alarmingly low, authorities say.
A pediatric dose of the Pfizer-BioNTech vaccine was authorized for 5- to 11-year-olds more than two months ago, yet as of Thursday, only 17.9% of children in this age group were fully vaccinated, according to the Centers for Disease Control and Prevention’s COVID Data Tracker. Even among 12- to 17-year-olds, who have been able to get the shot for at least eight months, only 54.3% are fully vaccinated.
Vaccinations among the elementary-school set surged after the shots were introduced in the fall, but demand has flattened since then. Even Omicron hasn’t persuaded many parents to make vaccination a priority.
The low rates are “very disturbing,” said Dr. Robert Murphy, executive director for the Institute for Global Health at Northwestern University’s Feinberg School of Medicine. Parents who hesitate “are taking an enormous risk and continuing to fuel the pandemic,” he said.
The CDC says 73.5% of U.S. adults are fully vaccinated. President Biden was hoping that figure would rise after the Occupational Safety and Health Administration required employees of companies with at least 100 workers to get the shots or submit to a weekly coronavirus test.
But the Supreme Court ruled Thursday that OSHA lacks the authority to implement a vaccine mandate. In a 6-3 ruling, the court’s conservative majority said the agency can protect people from workplace threats, but the coronavirus doesn’t qualify because it is “untethered, in any causal sense, from the workplace.”
About 84 million Americans would have been subject to the vaccination mandate. Biden said he was disappointed with the ruling and called on states and businesses to institute vaccine requirements on their own.
In a separate decision, the high court upheld a smaller, more targeted regulation that requires about 17 million workers in hospitals and nursing facilities to be vaccinated. That one passed muster because it was based on the Medicare and Medicaid Acts, which authorize federal health officials to set standards to protect the health and safety of elderly and sick patients.
Earlier Thursday, Biden gave a speech outlining his plans to reinforce a healthcare system being swamped by Omicron. Among other things, he said his administration would double its purchase of coronavirus tests — from 500 million to 1 billion — and distribute them through a website that goes live next week.
In addition, the military will dispatch 120 medical personnel to hospitals in six states as part of a program that could ultimately send 1,000 service members all over the country. Biden added that “while the military is stepping up as they always do, there are others sitting on the sidelines or, worse, standing in the way.”
Some health experts said the new measures, although better than nothing, are too little, too late. The Omicron wave may be subsiding by the time some of these initiatives come to fruition, said Dr. Amesh Adalja, a senior scholar at the Johns Hopkins Center for Health Security.
Your questions answered
Today’s question comes from readers who want to know: Has Omicron made my cloth mask obsolete?
Any mask, including a cloth mask, is better than no mask. But since the Omicron variant spreads so much more readily than its predecessors, health officials are encouraging us to up our mask game.
The California Department of Public Health says an effective mask has two key qualities. The first is “good fit,” meaning there are no gaps between the edge of the mask and the face where the coronavirus could slip through. The second is “good filtration,” which means the viral particles can’t pass through the mask itself.
Doing both of those things well is a tall order for an all-cloth mask. Even if made with three or more layers of fabric, all-cloth masks have been placed in the “least effective” category by state officials.
A better cloth mask contains two layers of tightly woven fabric sandwiching a filter insert made of polypropylene or another synthetic fabric. It should have a wire to create a tight fit around the nose and adjustable ear loops or head straps to minimize or eliminate gaps elsewhere on the face.
But California knows you can do better. It says a regular surgical mask is “effective,” and a fitted surgical mask is “more effective.” A fitted version includes a nose wire and adjustable ear loops or straps. It should also meet certain standards for filtration efficiency. (You can view those standards here.)
Another option to convert a regular surgical mask into a fitted one is to layer it with a cloth mask or a mask brace that holds the edges close to your face.
KN95 and KF94 masks are also listed as “more effective” options, and N95 respirators stand alone in the “most effective” category. None of these masks needs to be layered with a second mask.
If you opt for a KN95, however, the CDC wants you to know that about 60% of these masks in the U.S. are counterfeit. The agency offers this advice for spotting fakes.
The CDC on Friday updated its own guidance on face masks. It says the best mask is one that fits snugly and is comfortable enough for you to wear consistently. Well-fitting cloth masks and surgical masks are OK in the CDC’s book; KN95s provide more protection; and N95s that fit correctly offer “the highest level of protection,” the agency says.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

That, of course, is Dr. Anthony Fauci. The picture was taken this week during a Senate hearing on the federal government’s response to COVID-19.
We talked earlier about some of the criticisms leveled by senators from both sides of the aisle. But there was a subplot involving Fauci and his chief critic, Republican Sen. Rand Paul of Kentucky (who happens to be a doctor as well).
Paul has repeatedly accused Fauci of lying about the pandemic, and in Tuesday’s hearing, Paul added the charge that Fauci tried to “take down” scientists who didn’t agree with him.
Fauci fired back, accusing Paul of using the pandemic “for your political gain.” He noted that Paul’s website includes a call to “#FireFauci,” accompanied by an invitation to donate to his campaign.
Fauci also complained that Paul’s rhetoric “kindles the crazies out there,” including a Sacramento man who planned to kill Fauci and other people in power. The man was en route to Washington, D.C., with an AR-15-style rifle, ammunition and body armor in his car but was arrested in Iowa after being pulled over for speeding.
It was Sen. Roger Marshall who made Fauci loose his cool. The Republican from Kansas accused the infectious-disease expert of hiding financial disclosure forms; Fauci responded that they were publicly available upon request.
“You’re so misinformed that it’s extraordinary,” Fauci told the senator.
Later, a microphone caught Fauci muttering off-camera. “What a moron,” he said.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




