Trump could still be infectious with the coronavirus at the next debate
- Share via
There is no certainty that President Trump will have recovered from COVID-19 by the time of the next scheduled presidential debate on Oct. 15, nor will it be assured that he won’t still be contagious, experts say.
And the 74-year-old president may still take another turn for the worse, as a common progression for severe cases of COVID-19 can involve a sudden deterioration about a week after the illness begins.
Also concerning, experts added, was the labored breathing Trump was observed to be suffering from in videotaped footage Monday. And worth watching for, they said, are the effects that can occur from taking powerful steroids like the one Trump is taking to combat COVID-19. Such medication can cause emotional instability and euphoria.
Those were some of the observations a panel of UC San Francisco physicians and professors made Tuesday, as the nation heads into an election month unlike any in the modern era.
Here are some of the key takeaways:
An Oct. 15 debate may be risky
Physicians likely cannot rule out with certainty whether Trump will have stopped being contagious by the time of the scheduled Oct. 15 town-hall-style debate in Miami with Joe Biden.
The U.S. Centers for Disease Control and Prevention says that people with mild to moderate symptoms may be infectious for up to 10 days after symptoms begin. But some people who are severely ill with COVID-19 can remain infectious for up to 20 days, a time frame that extends past next week’s debate.
In general, people with severe COVID-19 — such as those suffering from inadequate oxygen levels in the body and those needing hospitalization — are more likely to be contagious for a longer duration. Trump is considered to have severe COVID-19, by virtue of his being prescribed a powerful steroid to combat the disease.
“We won’t really be able to assess infectiousness unless we were to culture virus from him,” said Dr. Chaz Langelier, assistant professor of medicine and an expert in infectious lung diseases. “That’s something that is challenging to do. Probably not very feasible.”
It could be days before Joe Biden and his wife can be sure they were not infected, according to medical experts.
Biden probably didn’t get infected by Trump
Seven days have passed since Biden and Trump met at their first presidential debate, and the former vice president again tested negative for the coronavirus on Tuesday. That would mean Biden is “essentially” out of the woods in his risk of contracting the coronavirus from Trump, said Dr. George Rutherford, a professor of epidemiology and biostatistics and an infectious disease expert.
The candidates’ podiums at the debate were more than 12 feet apart.
Trump’s coronavirus infection could endanger the health of Biden and others at debate next week in Miami. Medical experts say Trump might still be contagious.
Trump probably started being contagious the day after debating Biden
Assuming that Trump was exposed to the coronavirus on Sept. 26, when he announced the nomination of Judge Amy Coney Barrett to the Supreme Court in a crowded White House Rose Garden, Rutherford suggested the following timeline: The president probably became hyper-infectious on Sept. 30 — the day after the debate with Biden — and symptomatic on Oct. 1.
Trump told Fox News on the evening of Oct. 1 that he and the first lady were being tested for the coronavirus, and after midnight the next day, tweeted that they had tested positive.
Here’s a typical, rough timeline of a coronavirus infection among people who show symptoms, according to Rutherford:
• On Day 3 after exposure to the virus, testing can begin to confirm infection.
• On Day 4, there’s enough virus in the body to be very infectious.
• On Day 5, symptoms begin, and the person continues to be infectious.
With just a month until the election, President Trump had a busy schedule the week he and First Lady Melania Trump tested positive for the coronavirus.
Super-spreading incidents of contagion are probably fueled by talking
The lengthy duration of talking by unmasked people at the tightly packed Rose Garden ceremony likely contributed to the super-spreading of the virus.
“If I were to attribute one behavior to it, I would say: garrulousness,” Rutherford said. “The more you talk — the closer you talk to people — that’s going to amp up the risk,” he said.
Wearing of masks at the event would have cut down on a number of the infections, Rutherford added.
Dr. Bob Wachter, chairman of the Department of Medicine and host of Tuesday’s panel discussion, said the risk of infection remains even in outdoor settings.
“If you’re close to somebody — and they were hugging and they were kissing, and all of that, and talking at very close quarters — it certainly is not 100% safe,” Wachter said.
A COVID-19 strategy without masks can fail
The president’s infection shows how a COVID-19 containment strategy that relies on rapid testing but not masks or social distancing can fail.
“Simply doing testing is not a substitute for wearing masks,” Langelier said. Even if a test performs the way it’s intended, tests can still result in false negatives.
“So while in theory, the approach of continually testing everyone who comes into contact with the president could work, it’s a strategy that does have flaws,” Langelier said.

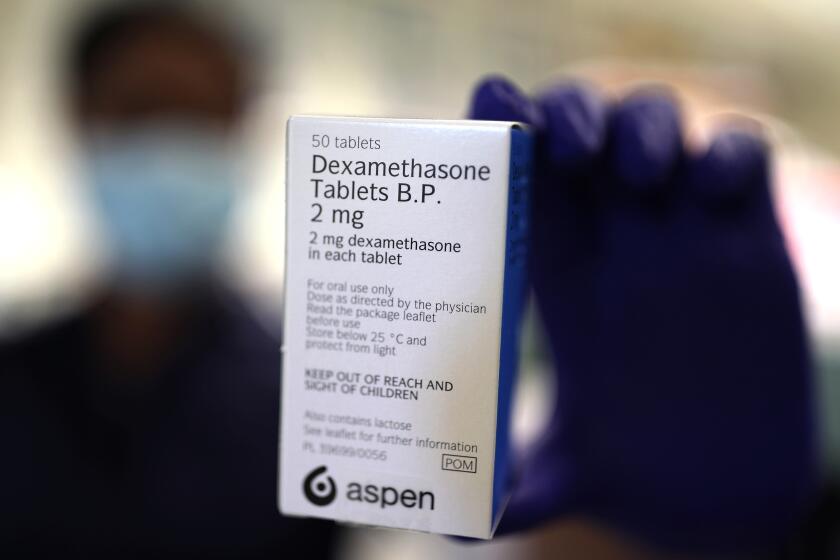
Trump’s medications indicate severe illness
The steroid Trump is taking indicates severe illness. Here’s a look at his medications:
The powerful steroid: Dexamethosone has been found to be especially helpful for critically ill COVID-19 patients in the intensive care unit, said Dr. Annie Luetkemeyer, professor of medicine and an expert on COVID-19 treatment.
The steroid can act to suppress the immune system, which can be a good thing in the illness’ second week, when doctors are trying to rein in an overactive immune system that has begun to destroy the body.
Luetkemeyer said she typically leans toward giving the steroid to people “who are really quite ill and require a lot of oxygen.”
But the drug can sometimes be harmful if given too early in the course of the illness — before the immune system has gone into overdrive.
“If you’re early on — in the first week when we see high viral load, but not as much immune dysregulation — then maybe you’re really not helping by giving someone dexamethosone,” Luetkemeyer said. “Steroids are powerful. ... So typically, for outpatients — or even people who are in the hospital on a low amount of oxygen or no oxygen at all — most of us are staying away from steroids.”
The antiviral drug: Remdesivir is an antiviral drug administered through intravenous fluid that blocks the coronavirus’ ability to reproduce itself, Luetkemeyer said.
If the drug is given, it’s more effective for it to be administered early in the illness, Luetkemeyer said. Administering it, however, is tricky, since it’s only available intravenously.
Early data suggest it reduced the median recovery time from 15 days to 11 days. “Remdesivir was superior to placebo in shortening the time to recovery in adults hospitalized with COVID-19 and evidence of lower respiratory tract infection,” a report in the New England Journal of Medicine said.
The lab-manufactured antibody: The so-called monoclonal antibody Trump has received is made in a lab. It is based on the identification of natural antibodies originally derived from someone who has recovered from the coronavirus that appear to work to bring viral levels down, according to Luetkemeyer.
Monoclonal antibodies have been used to treat other diseases, such as cancer. But they remain an experimental idea for COVID-19.
Trump’s doctors treated his COVID-19 with corticosteroid drug dexamethasone. That suggests his early response to the coronavirus spurred serious worry.
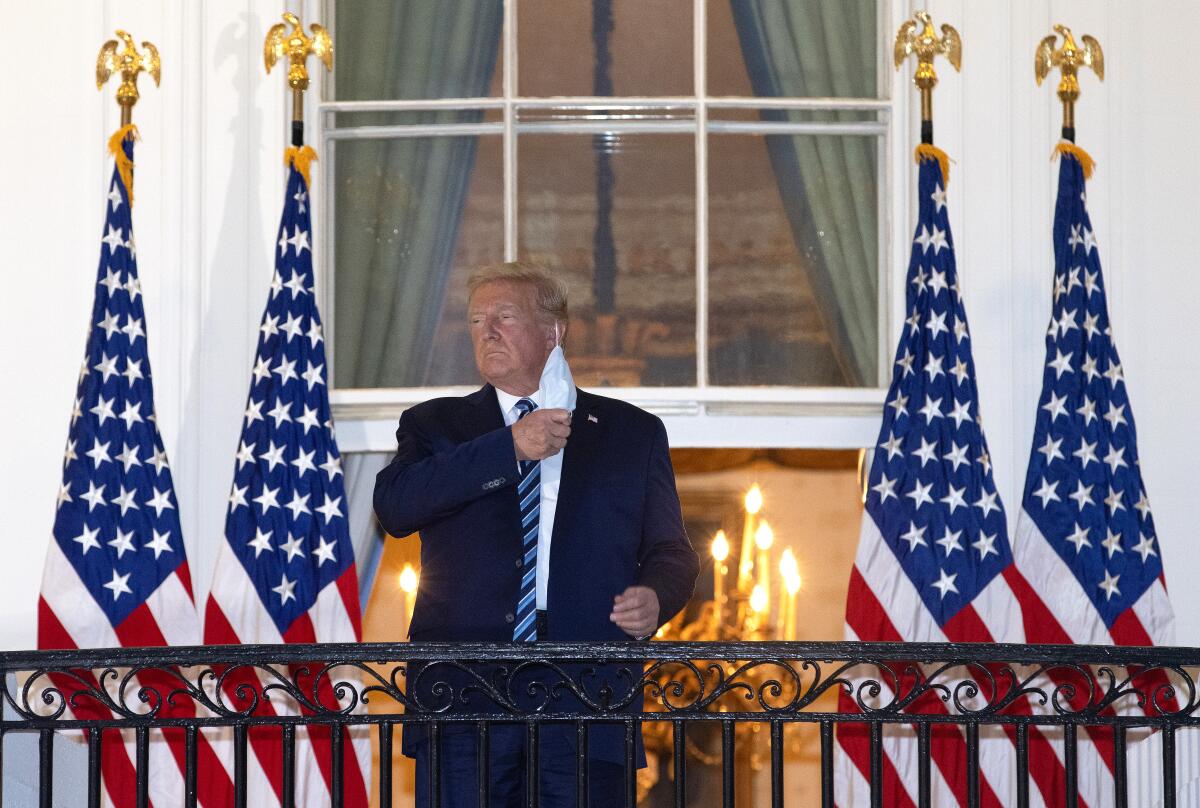
Doctors observed Trump with labored breathing
When Trump returned to the White House on Monday night after being hospitalized at Walter Reed National Military Medical Center, “he did not look good at the top of the steps. He looked like he was breathing harder,” Wachter said.
Wachter cited a tweet by Dr. Talmadge King, dean of the UC San Francisco School of Medicine and a world expert in lung disease, who wrote that the president looked out of breath after walking about 60 paces and up 30 steps. “His ‘energy’ not real, probably side effect of steroids,” King wrote.
“This is what patients look like when a significant part of their lungs can’t exchange oxygen/CO2. A truly scary feeling,” Wachter said on Twitter.
A sudden deterioration in health may still be possible
The CDC has warned that some patients rapidly deteriorate one week after illness onset, something that Dr. Peter Chin-Hong, a professor of medicine and an infectious disease specialist, has also observed.
Sometimes, it’s on that seventh day that the patient suddenly starts needing a lot more oxygen and is forced to come back to the hospital, Chin-Hong said.
President Trump once again finds his handling of the coronavirus crisis coming under fire on multiple fronts.
Euphoria should be monitored in patients taking steroids
Chin-Hong said that among patients taking steroids, people can feel “euphoric.”
“You feel on top of the world,” and the drugs can provide a “steroid buzz,” Chin-Hong said. “That time that I took it ... I felt a little bit like I was the ruler of the universe.”
Langelier also said he felt the side effects of a steroid. “I took 40 milligrams for a week for poison oak. And, man, I wanted to go buy a boat.”
A steroid can be enough to make a patient feel “peppery,” Luetkemeyer said. “It can make people feel differently. And sometimes that’s just a little bit more energy. And sometimes it can be a little more than that.”
Luetkemeyer said when she prescribes steroids or narcotics, she warns patients “that this will change your behavior potentially, you know — it’s not a time to sign checks.”
If Trump needs to head back to the hospital, what are other risks doctors need to watch for?
COVID-19 can lead to blood clots, Luetkemeyer said.
“One of the complications we can see is that people can get blood clots ... that can go to the lungs,” Luetkemeyer said, forming what’s called a pulmonary embolus.
If a patient had a more severe lack of oxygen and trouble breathing, Luetkemeyer said she’d want to know whether the patient had a pulmonary embolus. This risk has caused hospitals to place patients on blood thinners to reduce the risk of such dangerous blood clots.
And even patients who do recover from COVID-19 can experience months of recovery and convalescence. Even among previously healthy young adults with no chronic underlying medical conditions, nearly 1 in 5 still felt sick two to three weeks after testing positive, according to the CDC.
“And,” Chin-Hong said, “if you [have] severe disease, it may take six, eight weeks — and I’m not even talking about those ‘long-haulers,‘” who still feel terrible for months.
“It’s no walk in the park, even if you survive.”
More to Read
Get the L.A. Times Politics newsletter
Deeply reported insights into legislation, politics and policy from Sacramento, Washington and beyond. In your inbox twice per week.
You may occasionally receive promotional content from the Los Angeles Times.