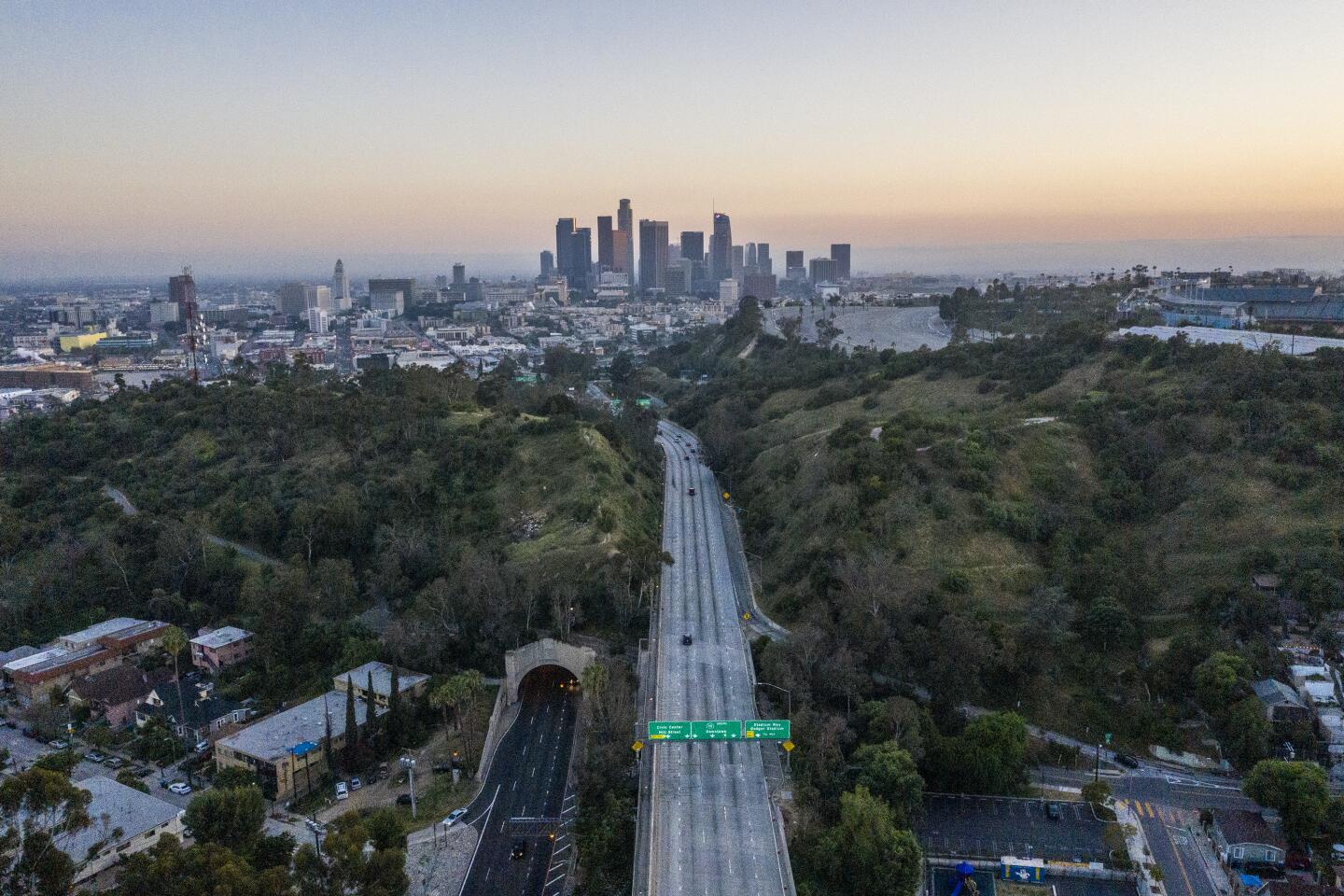
Social distancing may have helped California slow the virus and avoid New York’s fate
- Share via
MILLBRAE, Calif. — For California and Washington, the coronavirus triggers came early. They pushed the two Western states to social distancing measures earlier than the rest of the country.
In the San Francisco Bay Area, the warning came while the Grand Princess cruise ship, carrying infected crew and passengers, lurked outside the Golden Gate. As the coronavirus cases spread in Silicon Valley, health officers as early as March 5 urged employers to consider allowing more employees to work from home, and companies to cancel large gatherings and nonessential travel.
By the time the ship docked in Oakland on March 9, the BART transit system had seen a 24% drop in ridership compared with a typical Monday in February. Ridership was down 75% a week later, the same day the Bay Area issued the nation’s first coronavirus shelter-in-place order.
In Seattle, the early deaths at a suburban nursing home at the end of February shocked many into action. By the first week of March, major tech companies were telling employees to work from home and local officials urged them to do so.
The coronavirus continues to spread rapidly in both places, but so far at a rate slower than in the country’s other hot spots such as New York, New Jersey, Michigan and Louisiana.
To be sure, the epidemic still could get dramatically worse on the West Coast. A San Francisco nursing home with more than 700 beds is contending with an outbreak that has infected two patients and nine staff members. There are signs of the contagion at 11 Los Angeles County nursing homes, too.
But experts are looking to California and Washington for signs that social distancing is making a difference.
With all eyes on the sharply rising curves showing the dramatic rise in cases, “if and when it flattens, you’ll see it here first,” said Dr. George Rutherford, an epidemiologist and infectious disease expert at UC San Francisco.
The implementation of the shelter-in-place orders in the Bay Area “happened closer to the introduction of the virus, so you haven’t had as many generations of transmission. So there are fewer cases per capita in the population,” Rutherford said.
While cautioning that there’s no way to predict the future, it’s plausible the Bay Area’s early action will allow it to avoid a New York-style surge in cases, he added.
Dr. Robert Kim-Farley, an epidemiologist at UCLA, said the numbers of hospitalizations and deaths provide a more accurate indicator of the outbreak’s trajectory than the number of cases identified through uneven testing. On Thursday, the total number of deaths in L.A. County nearly doubled in a single day.
“I will anticipate that we will continue to see increased in hospitalizations and deaths, but I think we should be able to see some leveling off of those numbers in a couple of weeks because of the physical distancing measures,” Kim-Farley said.
Indeed, Gov. Gavin Newsom said Monday that the number of patients hospitalized with COVID-19 had doubled over the course of four days — and the number in intensive care units had nearly tripled.
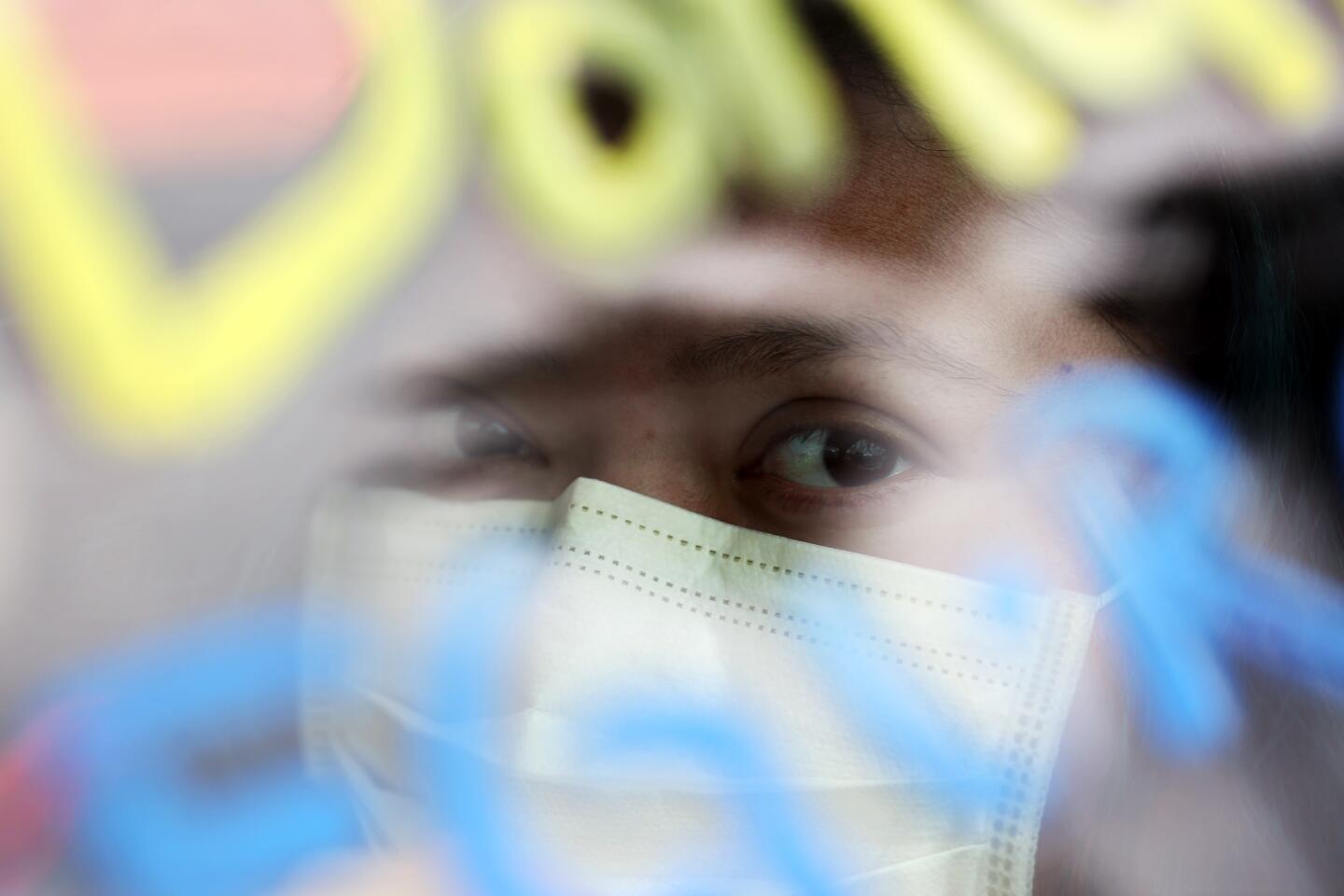
After a person is infected with the coronavirus, it can take two to 14 days for symptoms — commonly fever, cough and shortness of breath — to appear. Then, in cases where the illness becomes severe, it usually takes an additional eight to 15 days for a patient to require treatment in an intensive care unit.
That means it can take weeks for the effects of stay-at-home orders become evident.
And there are a number of things that can still go wrong for California.
The state does not know how many people are flouting the order to stay at home as much as possible and keep at least six feet away from others, said Dr. Otto Yang, an infectious disease expert at UCLA Medical Center, where coronavirus cases have climbed sharply in the last couple of weeks.
A few news accounts suggest that some Californians are skeptical about the threat from the virus and the need for physical distancing.
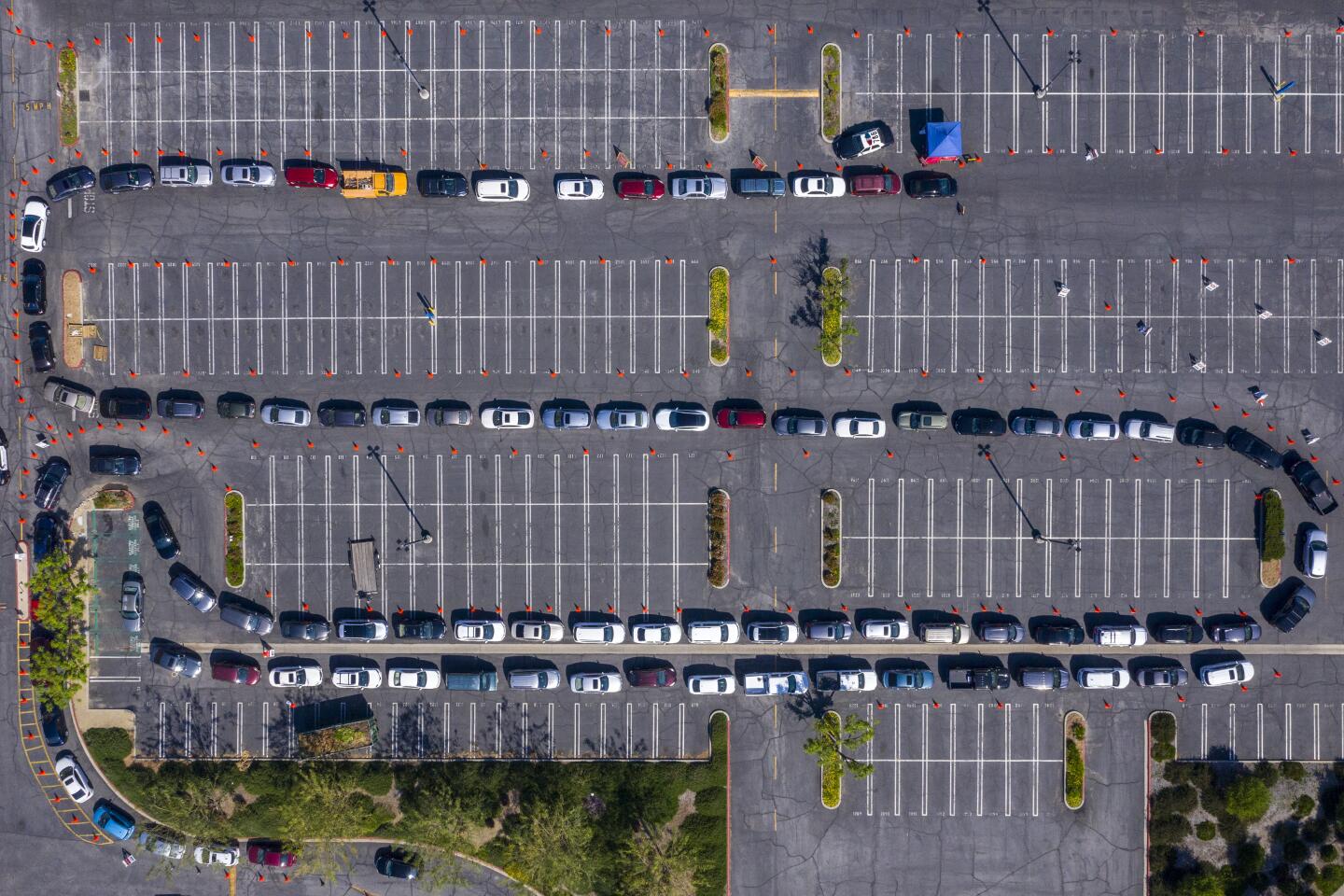
The lack of widespread testing can also mask how many people are actually infected and passing the virus around, Yang said. The true number “is going to determine how much hospital resources are going to be needed,” he said.
The Bay Area stunned the nation on March 16 when health officers in six counties jointly ordered residents to shelter in place to curb the spread of the coronavirus, officially known as SARS-CoV-2. Eleven other California counties soon joined the order, and on March 19 it was expanded statewide by Newsom.
New York state, by contrast, issued a stay-at-home order on March 20, and made it effective on March 22.
California’s earlier, aggressive stay-at-home order is one reason why a model published by the University of Washington’s Institute of Health Metrics and Evaluation suggests that New York state will see its worst day of the epidemic in early April, and that it will be dramatically worse than California’s worst day.
The report projects the peak of hospitalizations and deaths in California to come in late April.
“Given what we’ve been seeing in California, we are expecting the peak of the epidemic — the intensity of it — to be lower than in New York,” said Dr. Chris Murray, professor and director of the Institute for Health Metrics and Evaluation and the author of the report. “That means the surge in the hospitals will be smaller.”
Officials advising President Trump said their model of the pandemic mirrors the University of Washington projections. But other experts have raised doubts about the conclusions.
Nicholas Jewell, a biostatistics researcher at UC Berkeley, said he is “very skeptical” about the work. He said it makes a number of assumptions that remain to be proved — including about the death rate in Wuhan, China, where the disease originated, and in one region of Italy hard hit by the coronavirus.
The University of Washington projections changed from Friday to Monday, as the researchers fed new data into their computer simulation. On Monday, it showed that California would most likely be hit with 4,306 deaths, compared with the 6,109 forecast last week. For New York, the projected death total rose considerably — from 10,243 to 15,546.
Those sharp shifts were another factor giving Jewell pause.
“I am not saying their answer is wrong,” Jewell said. “I am just saying we shouldn’t put too much confidence in it yet.”
A University of Washington biology professor also raised questions about the projections, saying they represent a “best case” model that appears to assume a degree of social distancing equivalent to that achieved in Wuhan.
“It’s not obvious to me, especially in states without control orders, that we will get anything like the shutdown we saw in Wuhan,” said Carl T. Bergstrom, an expert in mathematical and computational biology.
Besides the later stay-at-home order for New York, other potential factors for that state’s sharp rise in cases include New York City’s population density and crowded mass transit system, Murray said.
Unlike the U.S., where tests have been in short supply, Asian cities had the advantages of being able to test for the virus widely, isolating the infected, finding their close contacts, and quarantining those who may have been infected.
Wide availability of tests in South Korea also gave health officials the ability to spot outbreaks before they emerged, allowing authorities to keep those with the potential to spread the virus away from uninfected people.
South Korea has far outpaced other countries including the U.S. in coronavirus testing, a move that could mean early detection and lives saved.
Models projecting the course of an epidemic can be controversial. The modeling is only as good as the data it is based on, and California is at disadvantage because of the lack of available tests, Barbara Ferrer, Los Angeles County’s public health director, said Friday.
Still, Ferrer said she thinks it is plausible that case numbers will continue to increase for three more weeks in L.A. County. Cases could continue to double every four to six days for weeks, given the rapid rise that has been seen so far in the region.
“Given what we know ... we’re likely to have a lot of people here that are going to be infected,” she said.
Dr. Grant Colfax, the director of public health in San Francisco, said it’s still too early to tell whether the rise in COVID-19 cases is slowing down.
“I simply do not know if our aggressive actions early on ... have had the intended effect,” he said. “I certainly am hoping and praying that that is the case. We still need the data to confirm that.”
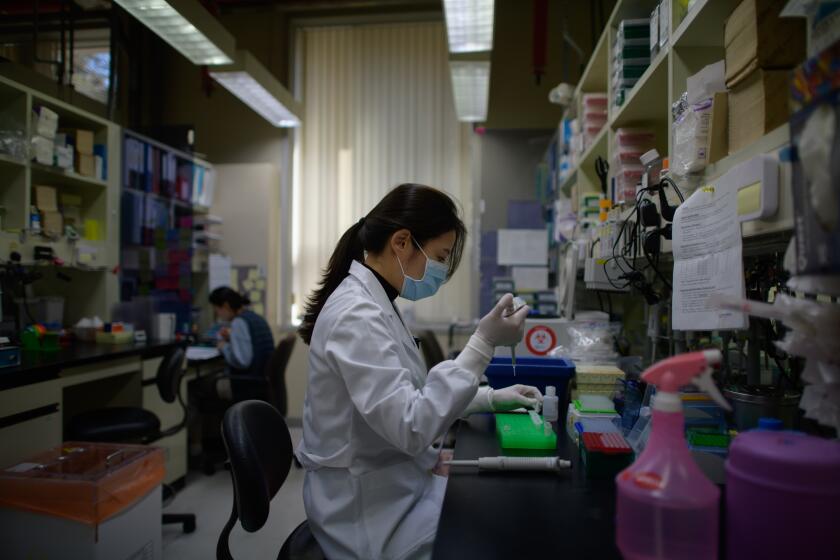
In the meantime, doctors at UCSF Medical Center are using the time to prepare.
“Every single day that goes by, we have an opportunity to get more ventilators, to re-purpose more clinical space, to open up isolation wards, to learn from our colleagues on the East Coast,” said Dr. Jahan Fahimi, medical director of the hospital’s emergency department. “So even when the surge comes … we now have the ability to meet more demand.”
Lin reported from Millbrae, Karlamangla from Los Angeles, Greene from Thousand Oaks and Rainey from South Pasadena.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.